![]()
![]() Category: Diagnostic
Category: Diagnostic
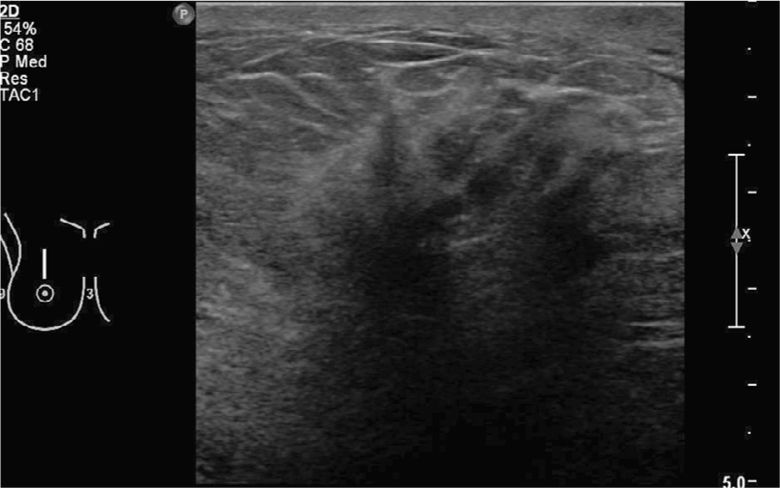
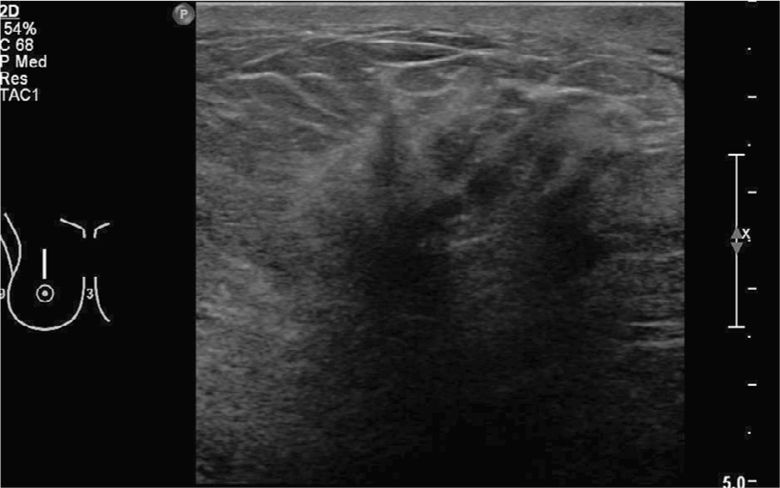
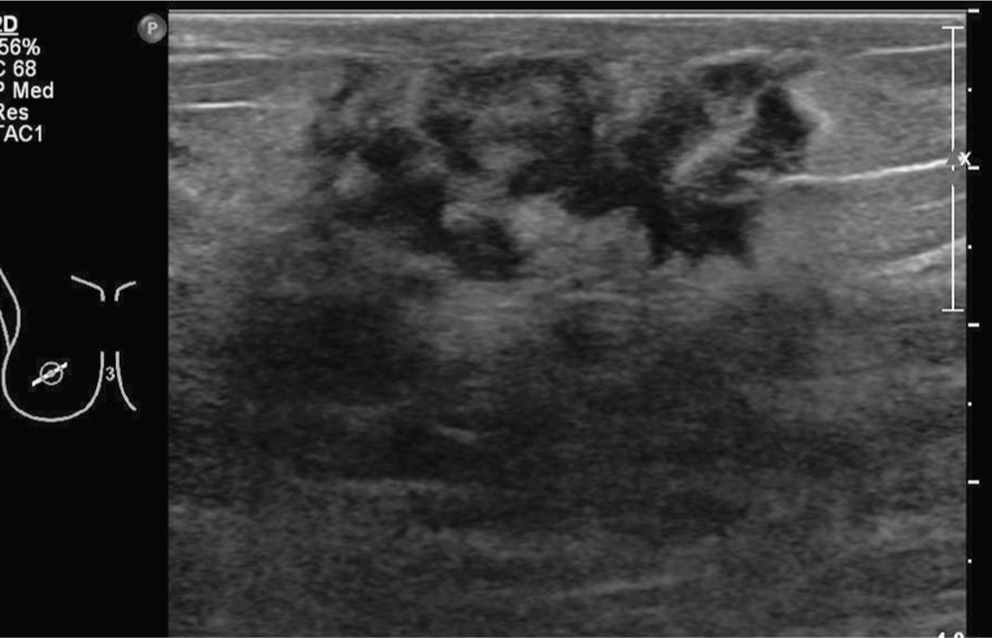
Gray-scale ultrasonography demonstrating large, highly suspicious mass in the right superior breast with “posterior acoustic shadowing” that corresponds to the mammogram finding.
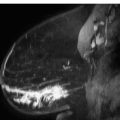
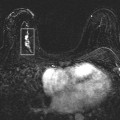
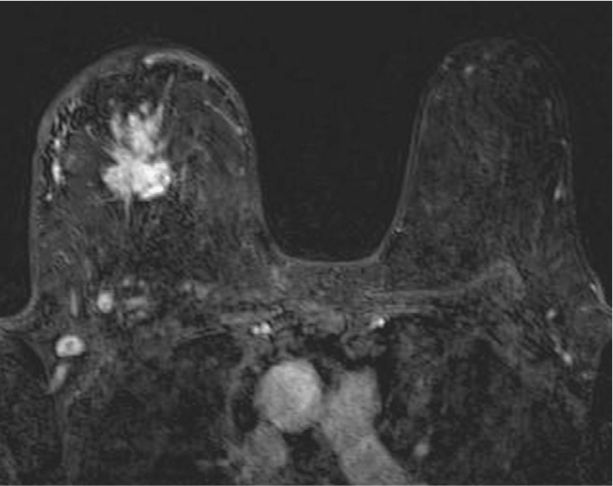
T1-weighted postcontrast sequence demonstrates the additional lesion near the chest wall.
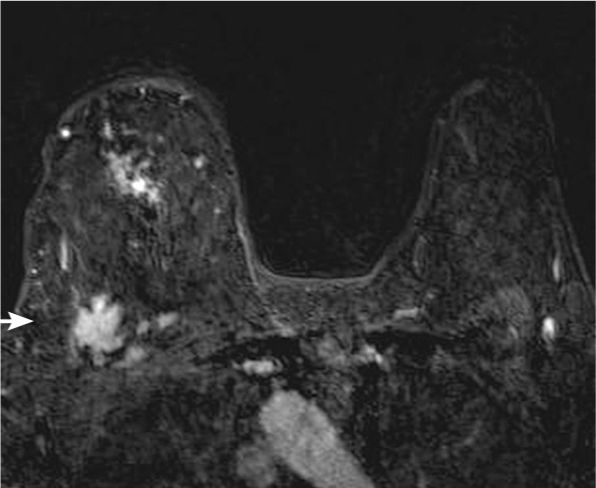
T1-weighted postcontrast sequence demonstrates the index lesion in the central right breast.
Answers
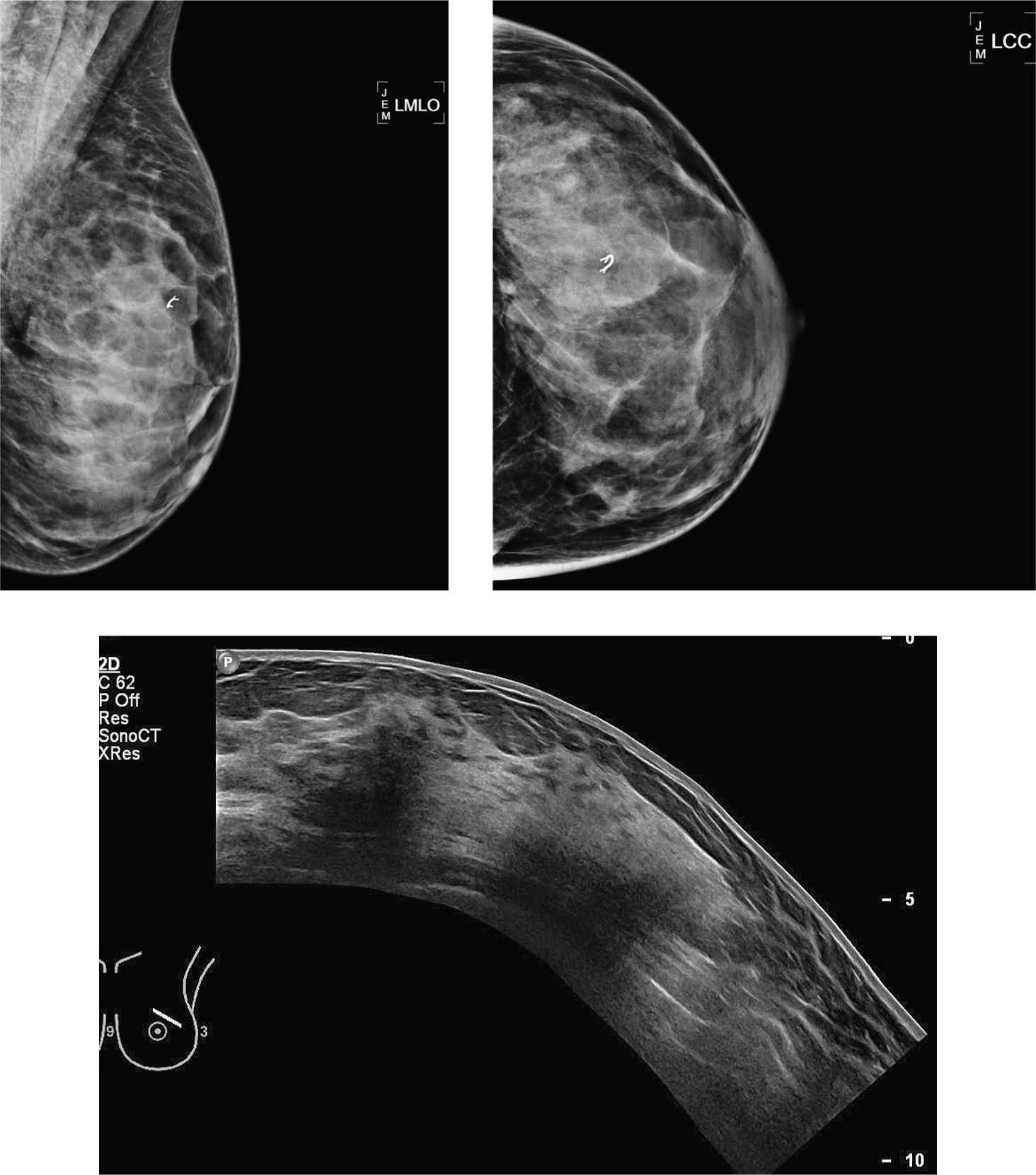
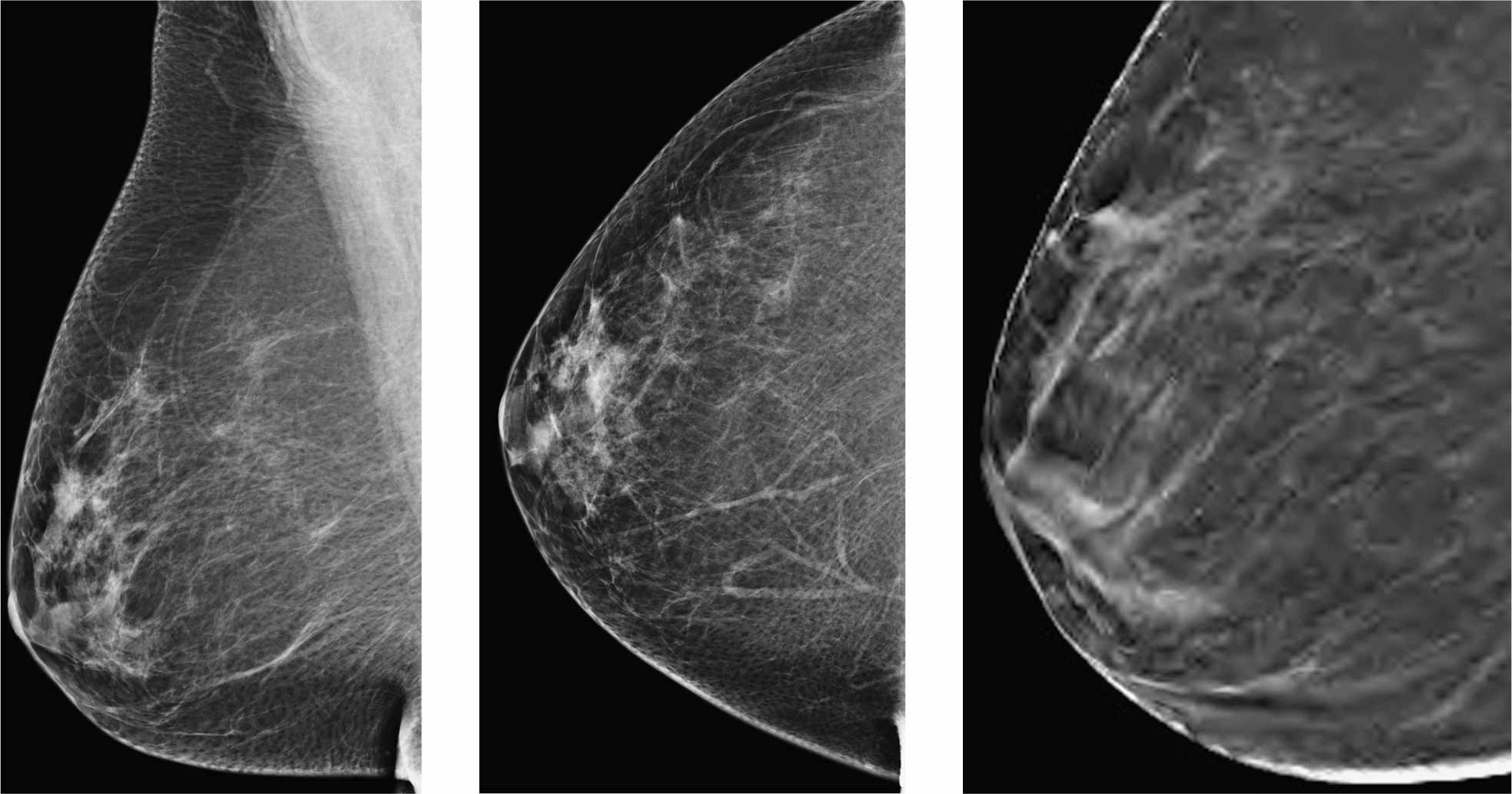
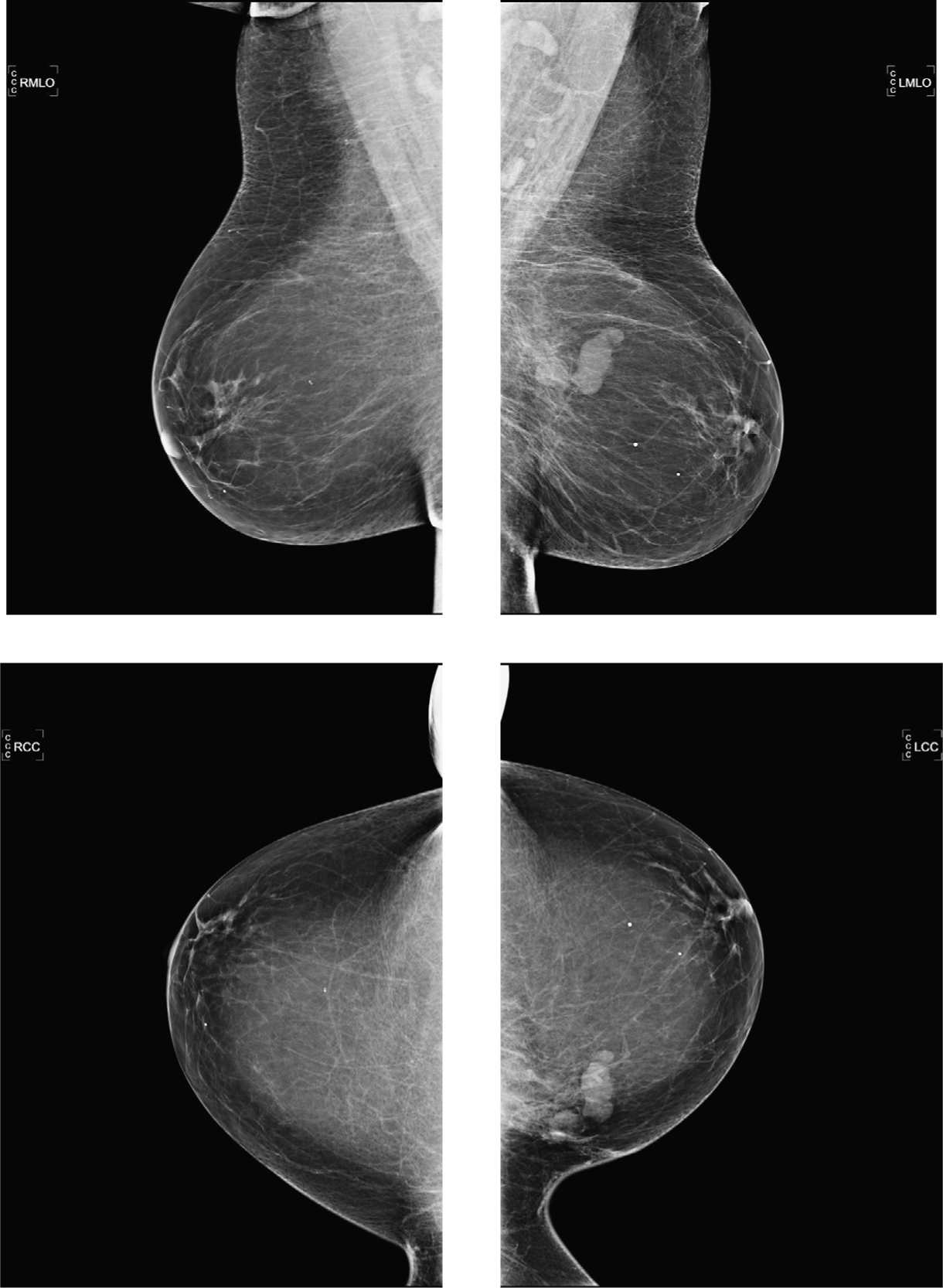
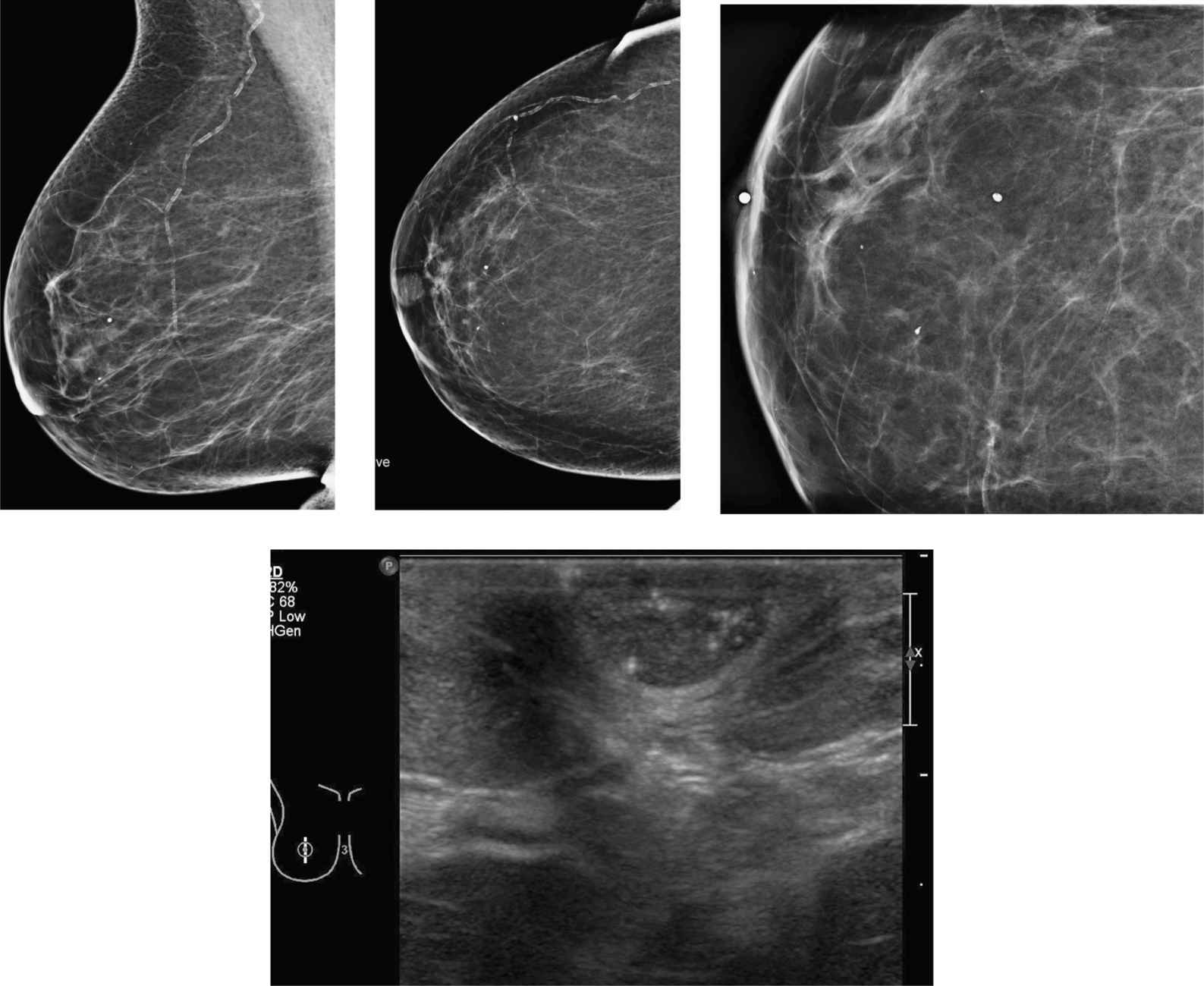
1. On the standard views (the spot compression views are not submitted), noted is a large area of “focal asymmetry” in the right superior breast with underlying “architectural distortion” and associated microcalcifications. Also noted is significant thickening of the right skin.
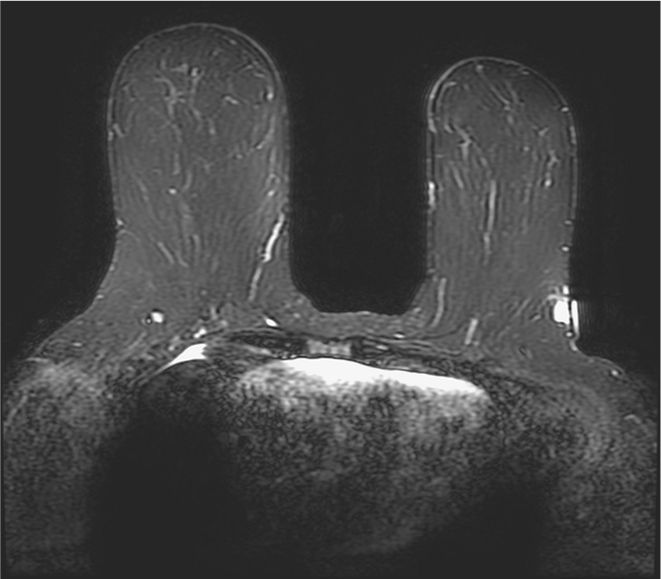
2. Noted on the MRI image is, in addition to the index lesion, additional 1.5-cm mass with strong enhancement in the lateral posterior right breast. This is better seen on the axial images. It is not well seen on the mammogram. It does show chest wall infiltration.
3. The index lesion as seen on mammogram demonstrates corresponding hypoechoic mass with strong posterior acoustic shadowing.
4. In general, the size of the lesion in comparison with the size of the breast will determine the need for mastectomy. In general, a mass or malignancy larger than 5 cm in an average-size breast likely requires mastectomy. Also the presence of skin or chest wall involvement and the presence of multicentric disease require mastectomy.
5. Based on a study by Fan et al looking at numbers of private community practice, surgical management is being changed after breast MRI in about 24%. Additional malignancies are being found in about 15% in the ipsilateral breast and in about 5% in the contralateral breast.
Suggested Readings
Fan C, Nemoto T, Blatto K, et al. Impact of pre-surgical breast magnetic resonance imaging (MRI) on surgical planning—a retrospective analysis from a private radiology group. Breast J. 2013;19(2):134-141.
Gutierrez RL, DeMartini WB, Silbergeld JJ, et al. High cancer yield and positive predictive value: outcomes at a center routinely using preoperative breast MRI for staging. AJR Am J Roentgenol. 2011;196(1):W93-W99.
Schell AM, Rosenkranz K, Lewis PJ. Role of breast MRI in the preoperative evaluation of patients with newly diagnosed breast cancer. AJR Am J Roentgenol. 2009;192(5):1438-1444.
Patient with palpable abnormality in the left breast, history of type II diabetes—status post old benign biopsy in the left breast
1. What are the findings on the mammogram?
2. What is the ultrasound finding corresponding to the palpable mass?
3. What is an appropriate next step?
4. What would be concordant pathology results of the previous left biopsy?
5. What is the consequence of the diagnosis of diabetic mastopathy?
Diabetic mastopathy 999
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
Ultrasound-guided biopsy of left breast.
Answers
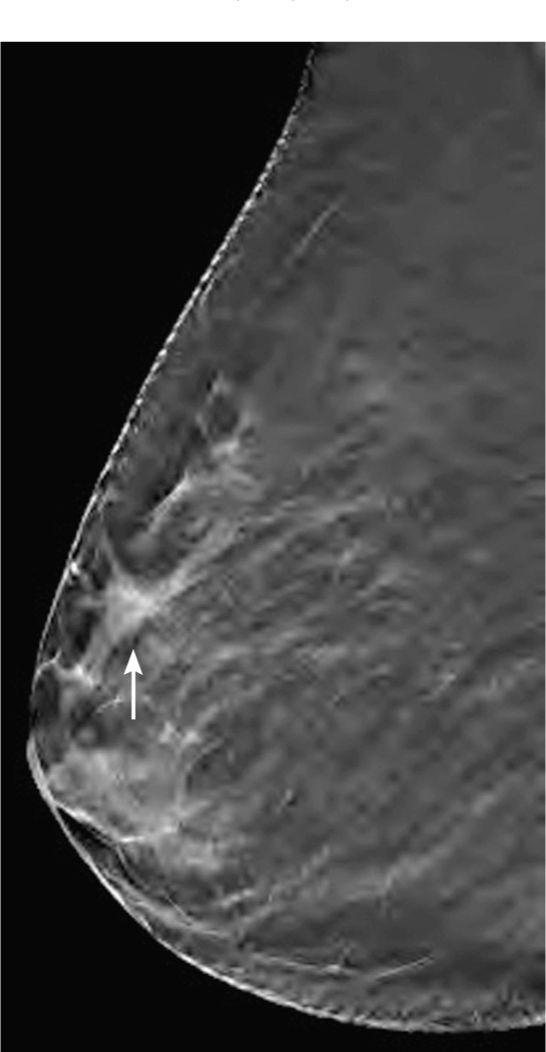
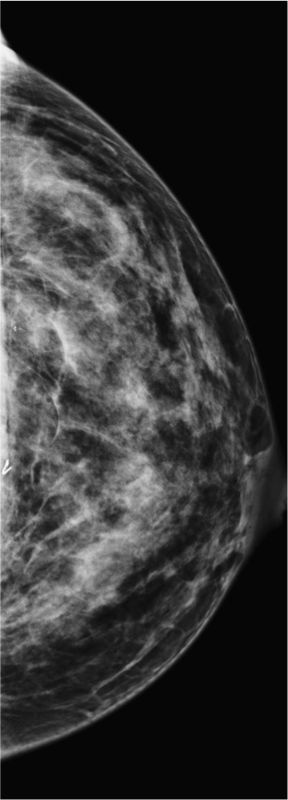
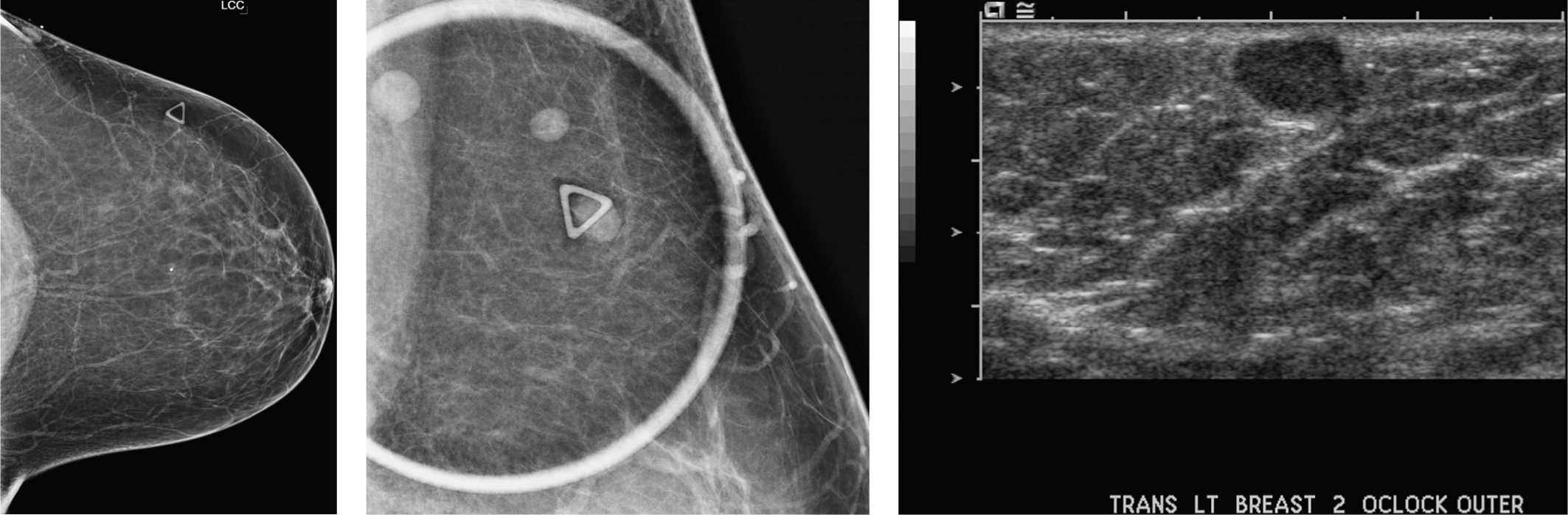
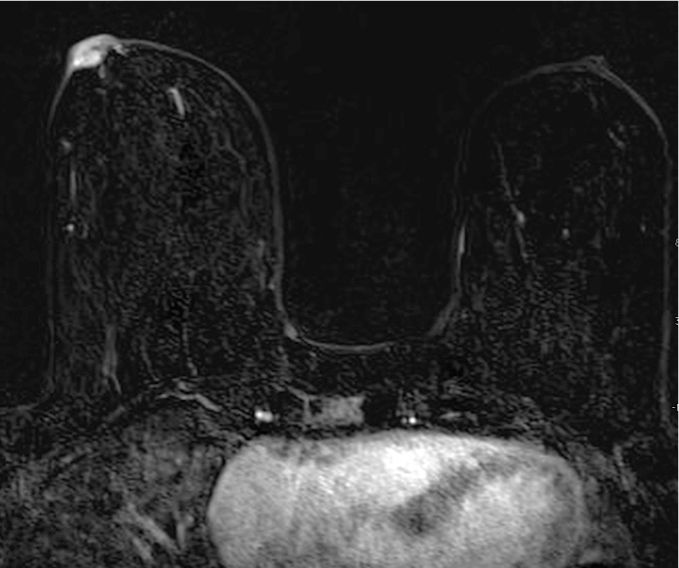
1. This is a mammogram with extremely dense fibroglandular tissue. There is clip in the superior breast from prior biopsy.
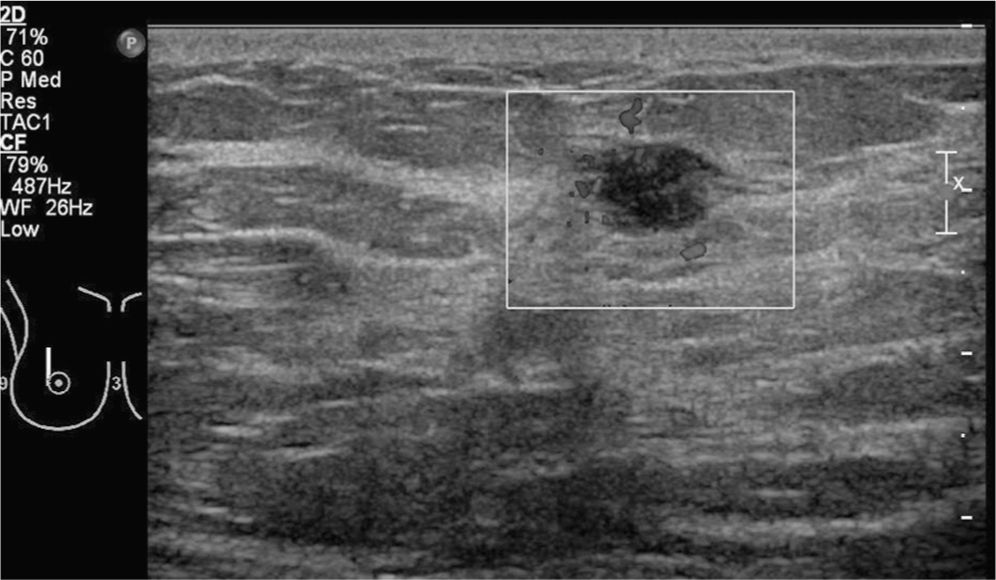
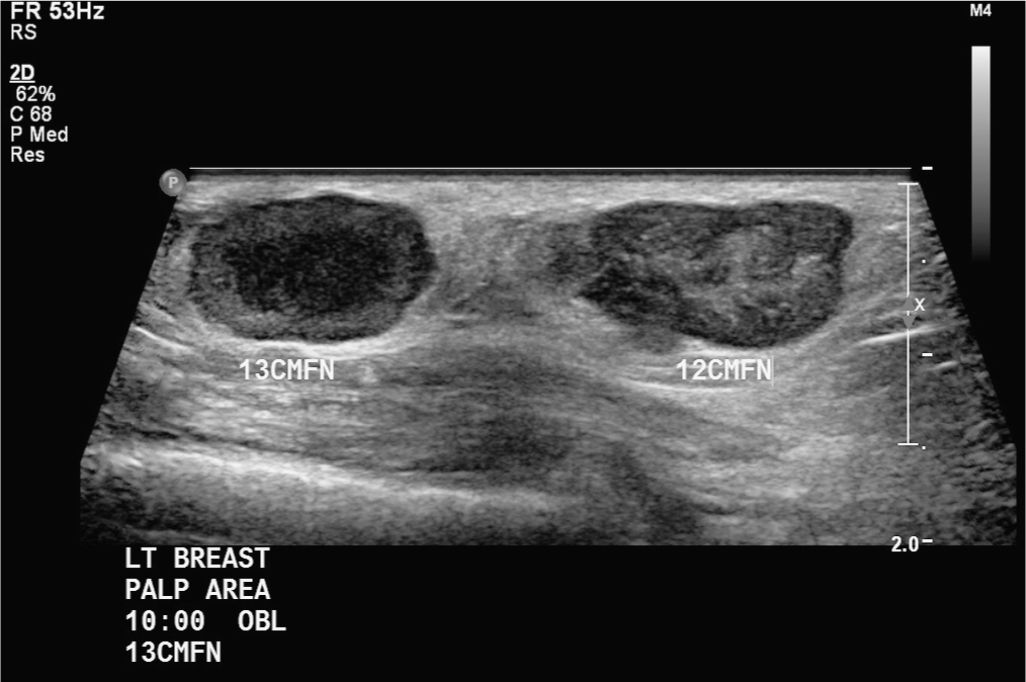
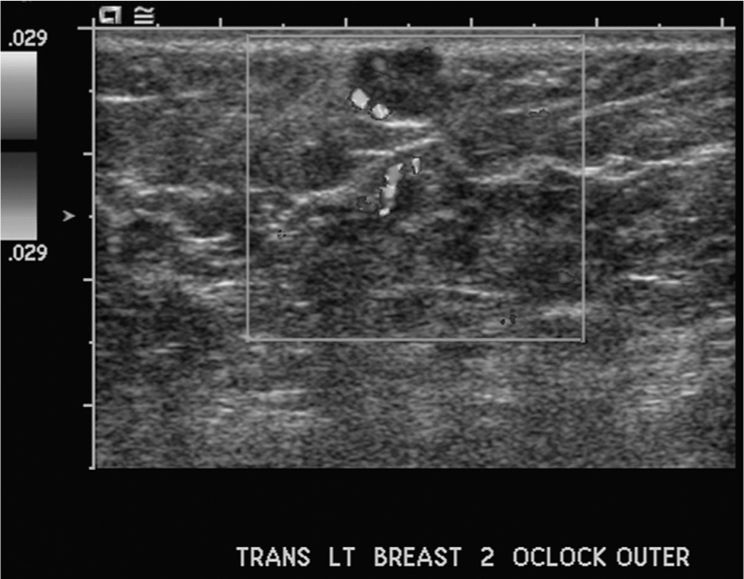
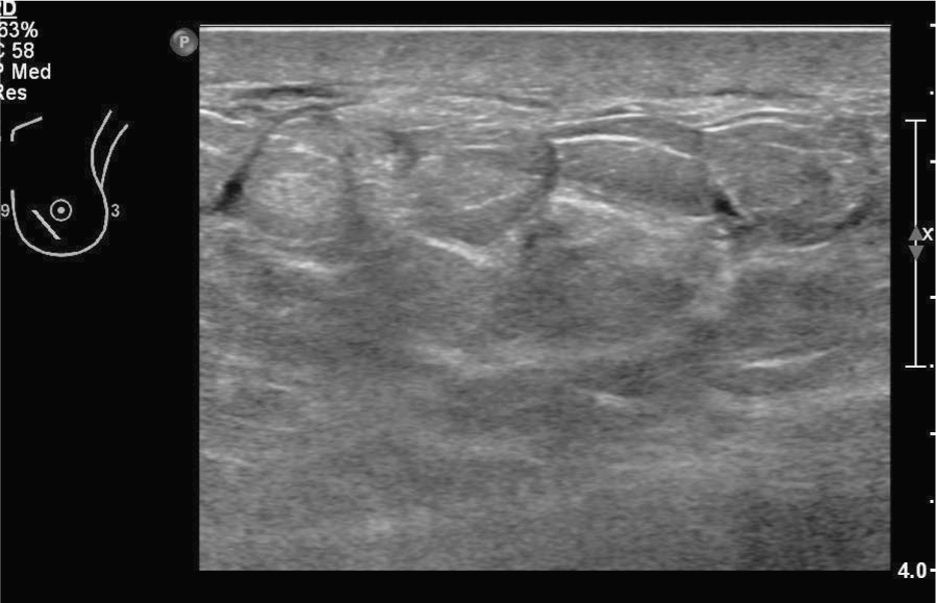
2. Corresponding to the palpable abnormality is a large hypoechoic mass extending into all quadrants with “posterior acoustic shadowing.” There was similar appearance of the right breast on ultrasound.
3. Ultrasound-guided core biopsy might be the first step. However, if patient had already prior biopsy, like in this case, which shows findings suggestive of diabetic mastopathy, and has a history of type I diabetes and if the finding on ultrasound is scattered throughout both breasts, it can be assumed that this is most likely a case of diabetic mastopathy and follow-up might be sufficient. There are reports that MRI might be helpful to distinguish malignancy from diabetic mastopathy.
4. All would be concordant, except the presence of benign fibroadenoma. The ultrasound finding could be malignant but would also be concordant with benign fibroproliferative changes including findings consistent with diabetic mastopathy. Diabetic mastopathy usually shows the presence of collagenous stromal fibrosis.
5. Diabetic mastopathy is a benign lesion and patient can return to screening mammography. Depending on the situation, further follow-up might be considered over a period of 2 years.
Suggested Readings
Gabriel HA, Feng C, Mendelson EB, Benjamin S. Breast MRI for cancer detection in a patient with diabetic mastopathy. AJR Am J Roentgenol. 2004;182(4):1081-1083.
Goel NB, Knight TE, Pandey S, Riddick-Young M,
de Paredes ES, Trivedi A. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics. 2005;25(6):
1547-1559.
Sakuhara Y, Shinozaki T, Hozumi Y, Ogura S, Omoto K, Furuse M. MR imaging of diabetic mastopathy. AJR Am J Roentgenol. 2002;179(5):1201-1203.
65-year-old woman with recall for questionable mass in the right upper outer quadrant
1. Is there any abnormality in the right upper outer quadrant?
2. What do you know about tomosynthesis?
3. How is tomosynthesis being used right now?
4. What do you know about primary lymphoma in the breast?
5. What is the appearance of lymphoma on imaging?
Primary breast lymphoma 764
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
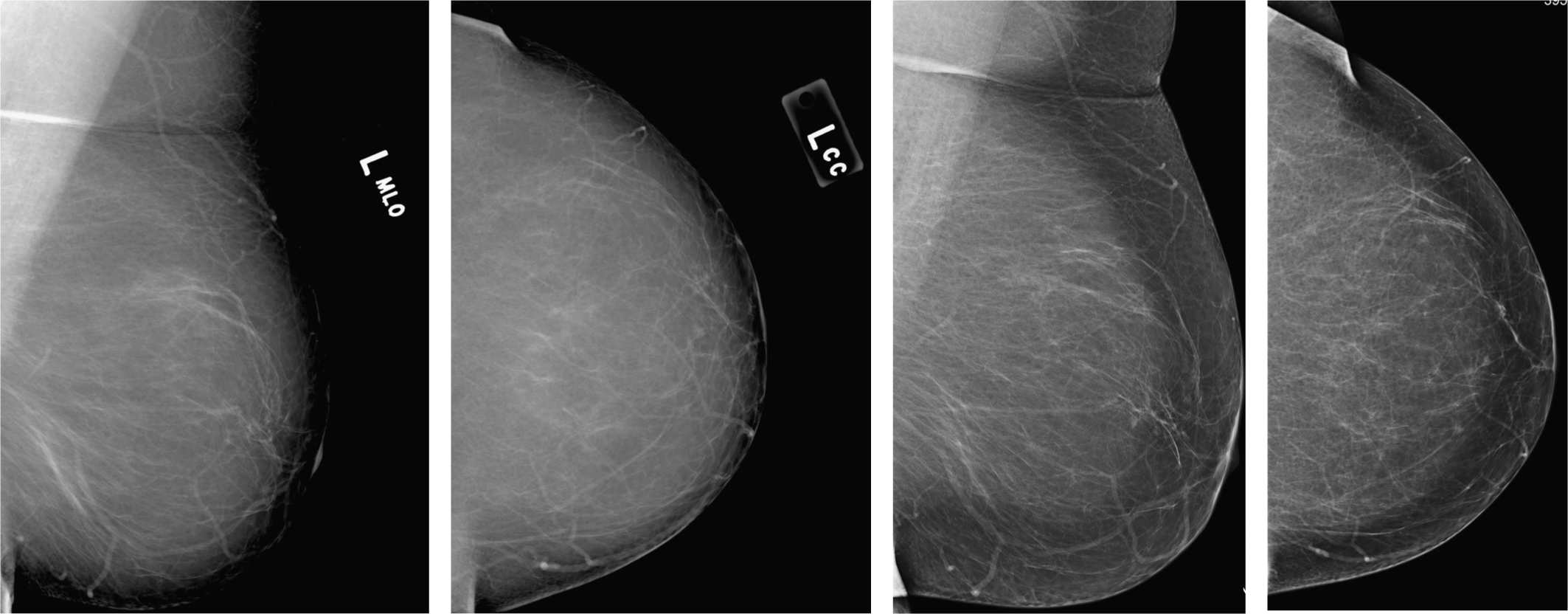
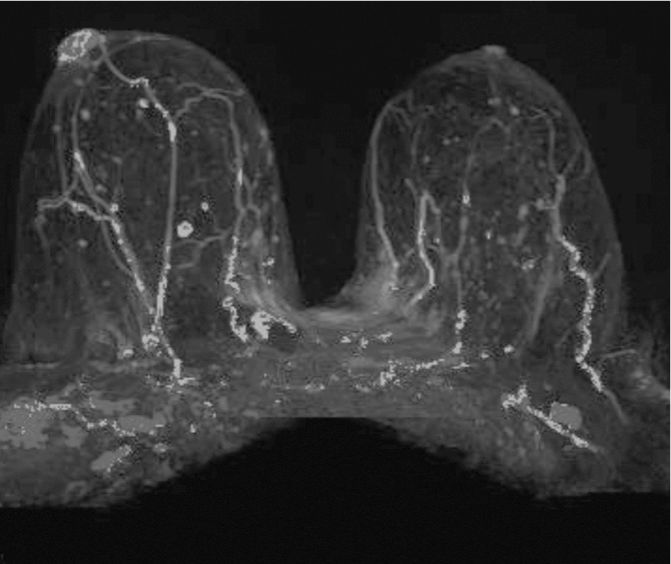
Tomosynthesis, right MLO, single 1-mm slice. Stack of slices replaces spot compression view.
MRI maximum intensity projection (MIP) image after IV contrast demonstrates area of abnormal enhancement corresponding to the ultrasound finding.
Ultrasound of right upper outer quadrant demonstrating mass at 11:00 close to the nipple. No increased flow on duplex.
Ultrasound of retroareolar breast demonstrates the hypoechoic area, irregular in shape, which corresponds to the MRI.
Answers
1. This is a case where old pictures would be extremely important—a theme that cannot be repeated enough in breast imaging; thus: OLD IMAGES ARE THE KEY IN BREAST IMAGING. Yes there is a questionable mass in the right upper outer quadrant.
2. Tomosynthesis is a new mammographic technique that utilizes movement of the tube to create several slices of the breast. It is called 3D mammography and the machine looks the same and the patient does not realize any difference, but the radiologist receives multiple thin cuts in CC and MLO projection, which can be scrolled through on the workstation. The conventional current mammography machines can be referred to as 2D mammography in that context. One company got FDA approval in early 2011.
3. Tomosynthesis (3D mammography) was approved for diagnostic workup in 2011 but not to replace 2D mammography for screening. It is currently being used to replace spot compression views, since it creates multiple slices and has more information than a conventional compression view. It is more problematic in regard to calcifications. It is used in conjunction with 2D mammography as a combo (2D/3D mammography), especially for dense breasts. It is also FDA approved in conjunction with conventional mammography for screening.
4. Lymphomas contribute to about 0.15 of malignant mammary neoplasm. Less than 0.5% of all malignant mammary lymphomas involve the breast primarily. Primary breast lymphoma has an age peak at the 4th to 7th decade. The diagnosis of primary breast lymphoma is limited to patients with no evidence of systemic lymphoma or leukemia.
5. On mammogram, primary breast lymphoma, but lymphoma in general, presents often as mass, most frequently with “irregular” shape and “indistinct” margin. Other presentations include the presence of “focal asymmetry.” Ultrasound demonstrates, in most cases, mass with “irregular” shape. Posterior to the mass, the echo can vary and could include “acoustic enhancement.” Color Doppler imaging shows frequently hypervascularity. MRI demonstrates lobular mass, often hyperintense on T2-weighted images and heterogeneous enhancement with rapid uptake and washout. PET demonstrates vivid uptake of FDG.
Suggested Readings
Hakim CM, Chough DM, Ganott MA, Sumkin JH, Zuley ML, Gur D. Digital breast tomosynthesis in the diagnostic environment: a subjective side-by-side review. AJR Am J Roentgenol. 2010;195(2):W172-W176.
Noroozian M, Hadjiiski L, Rahnama-Moghadam S, et al. Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization. Radiology. 2012;262(1):61-68.
Yang WT, Lane DL, Le-Petross HT, Abruzzo LV, Macapinlac HA. Breast lymphoma: imaging findings of 32 tumors in 27 patients. Radiology. 2007;245(3):692-702.
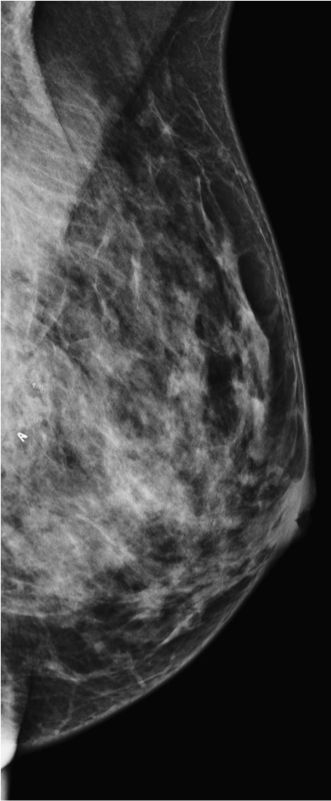
Palpable lump in the left breast
1. What BI-RADS classification should be used here?
2. What is the next imaging test?
3. What type of tumor does a chondrosarcoma arise from?
4. What determines whether a chondrosarcoma is primary breast or arising from another lesion?
5. What is the best way of treating a chondrosarcoma of the breast?
Chondrosarcoma of the breast 600
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
Ultrasound shows two circumscribed complex echogenicity masses. Note the acoustic enhancement behind the lesions. The mass on the left also shows a liquid necrotic center.

Ultrasound shows that although the mass is sharply marginated, the margins have a microlobulated appearance. There are some low echo slit-like areas raising the possibility of a phyllodes tumor.
Answers
1. Although these masses are not calcified and have circumscribed margins, their distribution is not normal. They are also palpable and feel hard, which does not fit with the normal presentation of fibroadenomas or tense simple cysts. A BI-RADS 4 assessment is the most suitable outcome.
2. Further evaluation with ultrasound is likely the best next investigation. You can perform further mammographic views if you think that the margins of the masses have not been demonstrated clearly. MRI is unlikely to give additional information to affect the management of the case.
3. Sarcomatous change has been reported in both phyllodes tumors and metaplastic carcinomas of the breast.
4. The presence of a primary sarcoma means that this is likely a secondary deposit. However, a chondrosarcoma can arise in a phyllodes tumor or a metaplastic carcinoma. Both of these lesions have an epithelial component, and so this should be excluded before calling a lesion a primary breast chondrosarcoma.
5. Treatment is primarily surgical. Chondrosarcoma of the breast is resistant to both chemotherapy and radiation therapy.
Suggested Readings
Patterson JD, Wilson JE, Dim D, Talboy GE. Primary chondrosarcoma of the breast: report of a case and review of the literature [published online ahead of print]. Breast Dis. 2011.
Verfaillie G, Breucq C, Perdaens C, Bourgain C, Lamote J. Chondrosarcoma of the breast. Breast J. 2005;11(2):147-148.
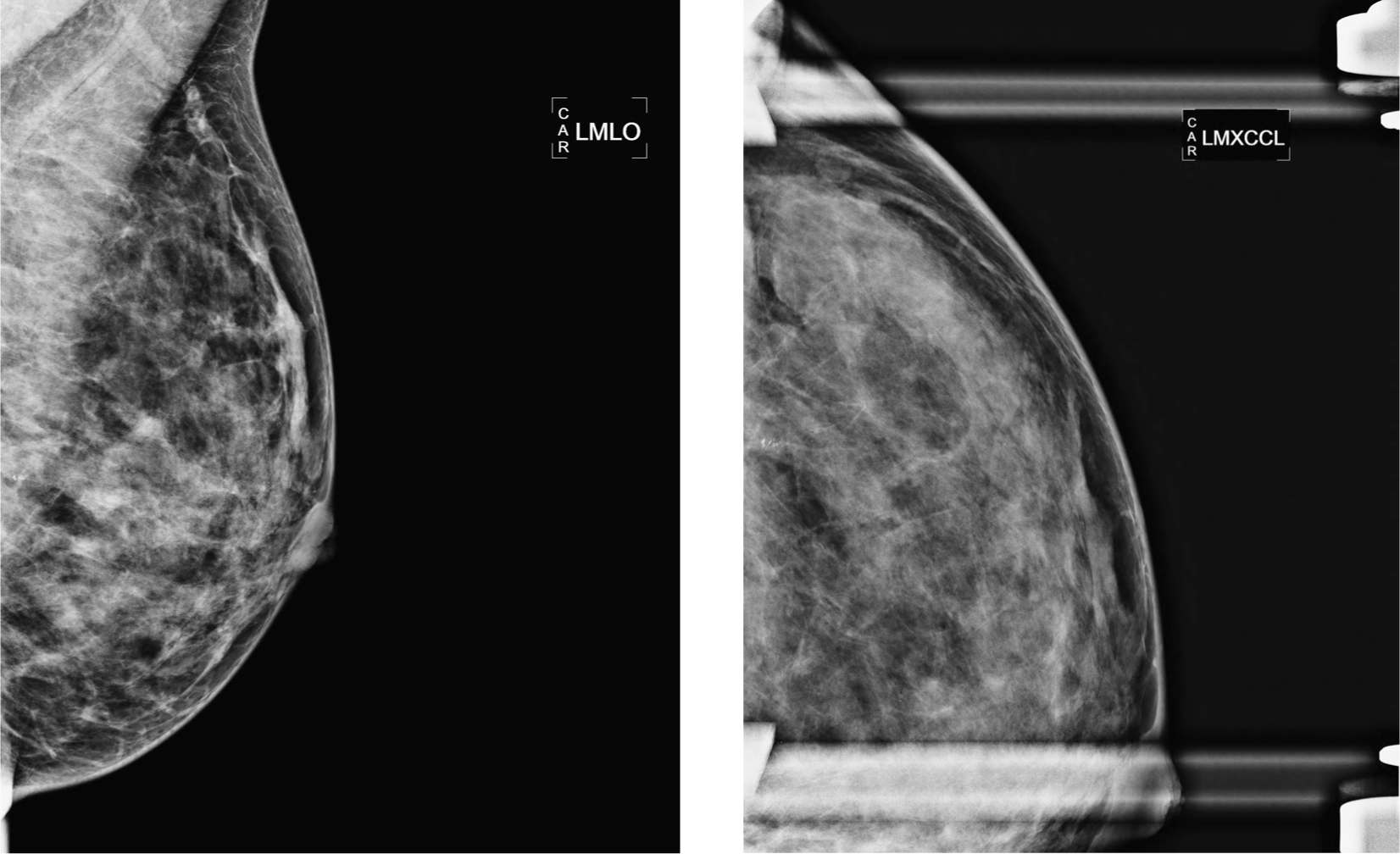
Screening mammogram of left breast in patient with two sisters with breast cancer—priors on left
1. What is the finding on the screening mammogram?
2. Who qualifies for MRI screening?
3. What are the factors being considered for the risk calculator of the National Cancer Institute?
4. What is the average lifetime risk of women up to the age of 90?
5. What other exam would be available if patient does not qualify for MRI?
MRI screening of high-risk patient with incidental finding 393
Case ranking/difficulty: ![]()
![]()
![]() Category: Screening
Category: Screening
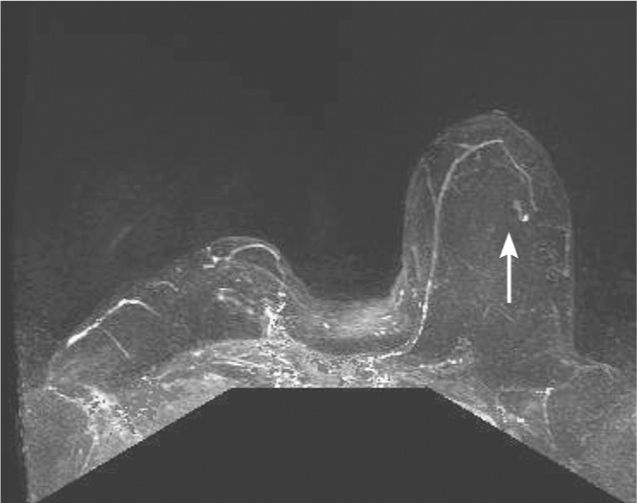
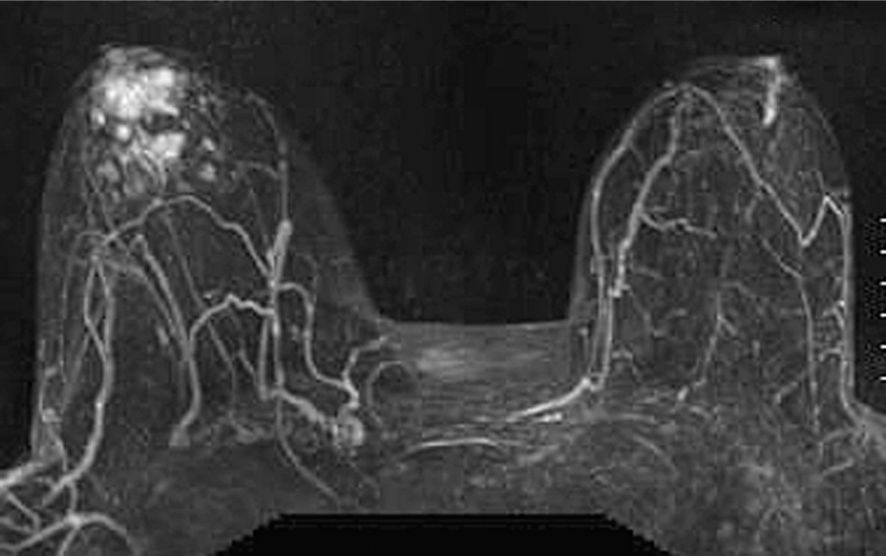
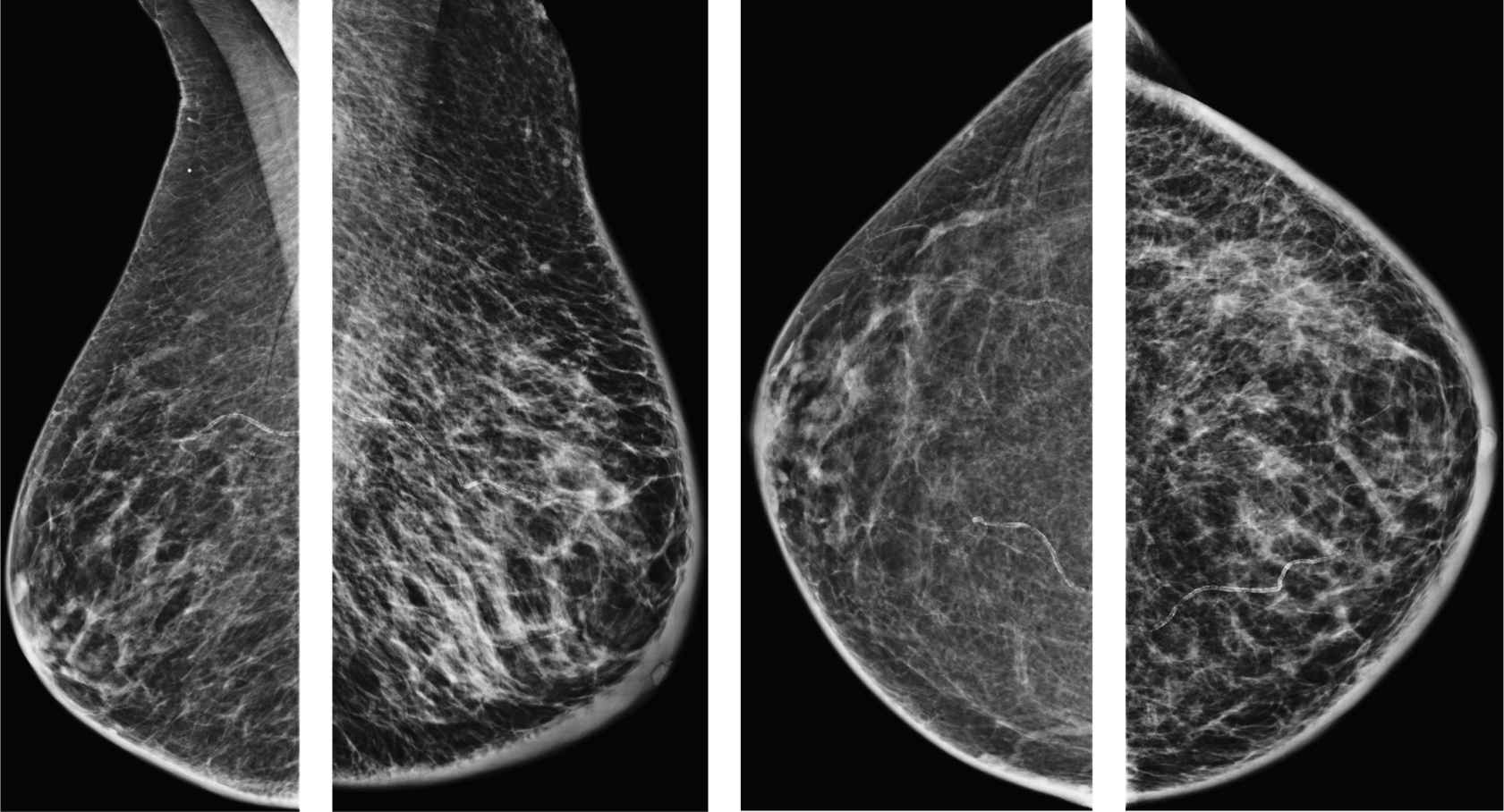
MRI of bilateral breast after IV contrast, maximum intensity projection (MIP) technique.
MRI of T1-weighted sequence after IV contrast demonstrates early enhancement of the small 4-mm mass.
MRI, T1-weighted sequence after IV contrast, sagittal reformation.
MRI of non–fat-suppressed T1-weighted sequence without contrast demonstrating small mass with “irregular” margin.
Answers
1. This is a normal screening mammogram.
2. Patients with a lifetime risk of 20% to 25%, patient needs two first degree relatives with breast cancer, for example, mother and sister.
3. Factors that will put into the calculator are as follows:
i. Personal history of breast cancer
ii. Woman’s age
iii. Woman’s age at the time of first menstrual period.
iv. Woman’s age at the time of her first live birth of a child
v. Number of first-degree relatives with breast cancer
vi. History of breast biopsies
vii. Race/ethnicity
4. Lifetime risk depends on the age and ethnicity; for a 40-year-old white woman, it is about 12.4%, and for a 40-year-old African American, it is around 9.6%.
5. In case of not qualifying for breast MRI—and in particular if the patient has very dense breast tissue—the other exams that would be complementary to mammography and widely available would be breast ultrasound. Breast ultrasound in general is not accepted for screening but is being used by request of the referring physician. Tomosynthesis would also be a helpful adjunct to standard mammography to increase sensitivity.
Suggested Reading
Warner E, Messersmith H, Causer P, Eisen A, Shumak R, Plewes D. Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med. 2008;148(9):671-679.
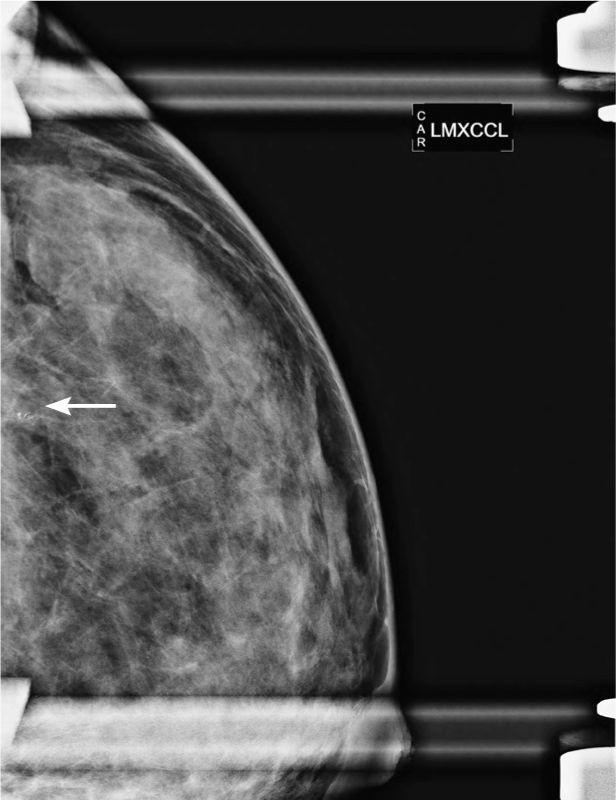
44-year-old woman with new suspicious calcifications in the left breast
1. Would these calcifications require biopsy if they were there 2 years ago?
2. What would be the procedure if these calcifications cannot be biopsied with stereotactic approach?
3. What are two important quality-assuring steps for performing a stereotactic biopsy.
4. If the post-biopsy marker clip is displaced, what might be the consequence?
5. How can clip displacement be avoided?
Where is the clip? 322
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
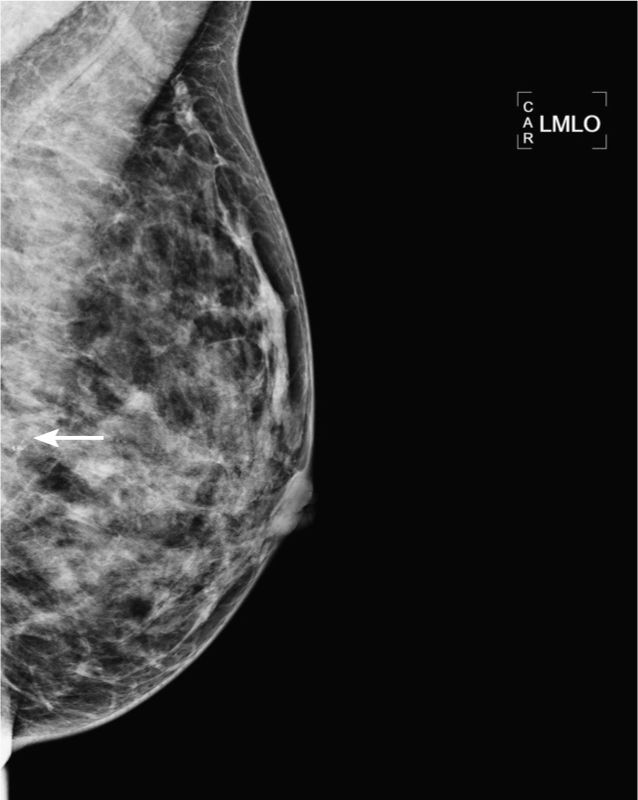
Diagnostic mammogram demonstrates group of suspicious calcifications in the left lateral, central, and posterior breast.
Diagnostic mammogram magnification XCCL view demonstrates group of suspicious calcifications in the left lateral breast.
Mammogram of left breast MLO view after stereotactic biopsy demonstrates clip at the level of the nipple.
Left CC view after stereotactic biopsy after clip placement demonstrates 3-cm clip medial from the residual calcifications.
Answers
1. Calcifications—if they are suspicious based on morphological features—need to be biopsied, even if they are stable over several old mammograms. They could represent ductal carcinoma in situ (DCIS), which can progress slowly over time, in particular if it is low-grade DCIS.
2. If suspicious calcifications are seen on two projections, they can be approached with needle localization and surgical excision can be performed. Calcifications such as in this case are not accessible to stereotactic biopsy due to their location within the breast, for example, since they are located very posteriorly, patient needs to be send for needle localization and surgical excision.
3. It is important to get a specimen radiograph after stereotactic biopsy of suspicious calcifications to prove that a representative sample of the calcifications was obtained. It is not the goal to excise all calcifications. Also important is that the postbiopsy mammogram shows the clip in good position, which means that the clip is in the target zone where the specimen was collected from.
4. In most cases, it is sufficient to document the location of the misplaced clip in relation to the area that was biopsied. There are rare cases where it is helpful to place a second clip. This can be the case if the clip is short in correlation to the target and therefore the needle localization would be less accurate.
5. Clip displacement cannot be completely avoided. It is caused by the release of compression after a stereotactic biopsy.
Suggested Reading
Esserman LE, Cura MA, DaCosta D. Recognizing pitfalls in early and late migration of clip markers after imaging-guided directional vacuum-assisted biopsy. Radiographics. 2004;24(1):147-156.
Palpable lump in the left breast
1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What is the next best imaging test?
4. What are the imaging features of a breast sarcoma?
5. What is the surgical treatment of breast sarcoma?
Angiosarcoma—presenting as a mass 1581
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
Left breast ultrasound with Doppler showing peripheral vessels—no surrounding vessels in subcutaneous tissues.
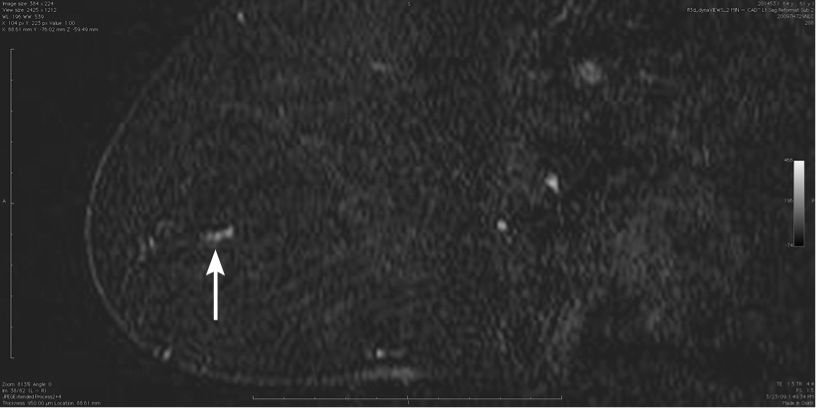
T2 axial MRI, shows homogeneous high signal circumscribed but superficial mass simulating fibroadenoma.

T1 fat sat axial 120 seconds following contrast injection.
Answers
1. BI-RADS 4—as the findings simulate fibroadenoma, there are some confounding features that allow you to recommend a biopsy.
2. Any of the first four answers can present as a circumscribed mass with peripheral vascularity. Interval change may help to differentiate a phyllodes tumor from a fibroadenoma. Metastases are common only when there is a known other cancer primary site setting. A simple cyst with proteinaceous debris should be belottable with gentle pressure on ultrasound. Seeing the internal echoes moving helps to distinguish form a solid mass.
3. The mass on mammography is circumscribed and similar to the nearby axillary lymph nodes. The initial ultrasound image shows that the mass is very superficial, unlike the normal position for a fibroadenoma, but could then be a node. Doppler ultrasound may show this mass to be highly vascular, including the surrounding breast tissue.
4. The characteristic features that make you suspect a sarcoma are the oval shape with indistinct margins, and marked vascularity on ultrasound. It is rare for a mass to be truly round unless it is a high tension simple cyst. Irregular margin to a mass is the suspicious finding arising from an invasive ductal carcinoma.
5. Lumpectomy with wide margins has been tried, but sarcomas when they recur are difficult to treat. The standard care has developed with mastectomy and no axillary procedure, as sarcoma rarely metastasizes to the locoregional lymph nodes. Mastectomy with reconstruction can be an option in sites with oncoplastic surgeons.
Suggested Readings
Babarovi![]() E, Zamolo G, Musta
E, Zamolo G, Musta![]() E, Str
E, Str![]() i
i![]() M. High grade angiosarcoma arising in fibroadenoma. Diagn Pathol. 2011;6(1):125.
M. High grade angiosarcoma arising in fibroadenoma. Diagn Pathol. 2011;6(1):125.
Cao Y, Panos L, Graham RL, Parker TH, Mennel R. Primary cutaneous angiosarcoma of the breast after breast trauma. Proc (Bayl Univ Med Cent). 2012;25(1):70-72.
Hui A, Henderson M, Speakman D, Skandarajah A. Angiosarcoma of the breast: a difficult surgical challenge. Breast. 2012;21(4):584-589.
Patient with discoloration of the right nipple: no discharge
1. What is the abnormality?
2. What are typical features of Paget disease?
3. What is the differential diagnosis?
4. Patient has eczema of nipple but normal mammogram—what is the next step?
5. What is the best technique to assess retroareolar breast on ultrasound?
Solid papillary carcinoma 759
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
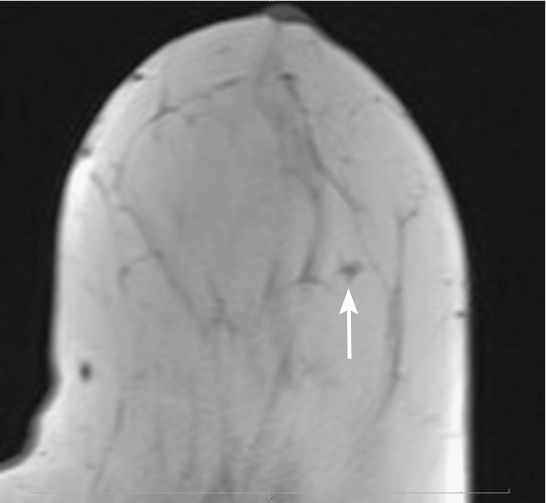
MRI T1-weighted sequence after IV contrast.
MRI T1-weighted sequence after IV contrast with CAD.
Answers
1. Noted is only minimal retraction of the nipple that was stable since prior studies (not submitted)—no other abnormality. Ultrasound does not demonstrate any abnormality neither.
2. Paget disease accounts for 2% to 3% of breast cancer. It is a clinical diagnosis with eczema of the nipple but has characteristic Paget cells within the dermis, which are consistent with adenocarcinoma. Mammograms are in most cases demonstrating findings related to high-grade ductal carcinoma in situ—however, mammograms can be normal as well.
3. Differential diagnosis could include scaring or eczema.
4. In general, ultrasound would be part of the workup to further exclude hidden abnormality in the retroareolar breast—especially in the presence of dense breast tissue. MRI can be helpful to evaluate for additional abnormalities or to further confirm abnormal nipple complex, but it is in general not required at this stage. Punch biopsy performed by breast surgeon is the crucial next step.
5. To assess the anterior retroareolar breast tissue on ultrasound and to avoid the posterior shadowing, it is helpful to compress the lateral aspect by hand and to elongate the tissue anteriorly and to approach the tissue with the transducer from the other lateral contour of the retroareolar breast. Any direct anterior approach at the level of the nipple will require large amount of gel to get rid of any air in between the transducer and the nipple.
Suggested Readings
Burke ET, Braeuning MP, McLelland R, Pisano ED, Cooper LL. Paget disease of the breast: a pictorial essay. Radiographics. 2000;18(6):1459-1464.
Haddad N, Ollivier L, Tardivon A, et al. Usefulness of magnetic resonance imaging in Paget disease of the breast. J Radiol. 2007;88(4):579-584.
Sundaram S, Prathiba D, Rao S, Rajkumar A, Rajendiran S. Solid variant of papillary carcinoma of nipple: an under recognized entity. Indian J Pathol Microbiol. 2011;53(3):537-540.
Status post–cardiac surgery, since then swelling left side of the body
1. What is the pertinent finding on this diagnostic mammogram?
2. What is the next step of workup?
3. What are other important findings to exclude?
4. What could be the diagnosis?
5. What is the most likely diagnosis in the absence of skin alterations and the presence of edema in left leg?
Unilateral edema due to congestive heart failure 1299
Case ranking/difficulty: ![]()
![]()
![]() Category: Diagnostic
Category: Diagnostic
Ultrasound demonstrating interstitial edema.
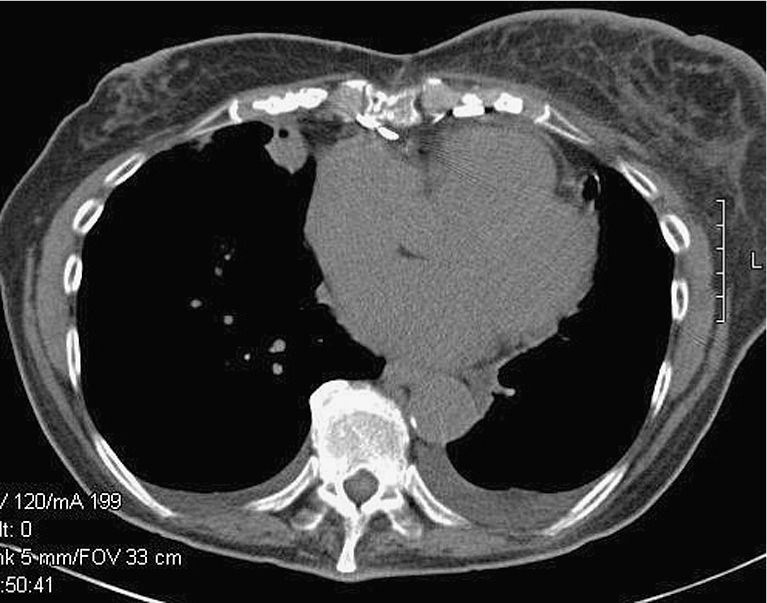
CT chest without contrast demonstrates the unilateral breast edema and pleural eff usion after heart surgery.
Answers
1. Patient demonstrates uniform reticular edema of the left breast, swelling of the left breast, and uniform thickening of the skin.
2. The most important next step is the clinical evaluation. In this case, patient presented with unilateral edema including leg and arm after cardiac surgery. She also noticed the enlargement of the left breast.
3. In this particular case, it is important to exclude any focal abnormal morphology in the breast, such as masses, microcalcifications, and/or lymphadenopathy. This presentation of the left breast can be seen with inflammatory malignancy. However, inflammatory skin changes such as redness and swelling are usually seen in the presence of inflammatory malignancies of the breast.
4. Differential diagnosis could include infection, status postradiation, lymphoma, unilateral cardiac edema, and, most importantly, the presence of inflammatory carcinoma of the breast.
5. This is, given the corresponding chronicity after cardiac surgery and the presence of leg edema, likely due to a rare case of cardiac unilateral edema. If there is remaining clinical concern, punch biopsy can be performed to exclude diagnosis of inflammatory carcinoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree