Congestive splenomegaly
Liver cirrhosis
Portal hypertension
Hepatic vein obstruction
Splenic vein obstruction
Infectious and inflammatory diseases
Infectious mononucleosis
Acquired immunodeficiency syndrome (AIDS)
Viral hepatitis
Typhoid fever
Tuberculosis
Malaria
Sarcoidosis
Hyperplastic splenomegaly
Spherocytosis
Thalassemia
Hemoglobinopathy
Infiltrative diseases
Leukemia
Lymphoma
Myeloproliferative disease
Extramedullary hematopoiesis
Storage disease
Neoplasm
Hemangiomatosis
Lymphangiomatosis
Peliosis
23.1.1 Congestive Splenomegaly
In congestive splenomegaly, an obstruction of portal venous outflow from the spleen leads to an increase in the amount of red pulp. The main cause of congestive splenomegaly is liver cirrhosis. Other causes including hepatic vein obstruction such as membranous obstruction of inferior vena cava (MOIVC) or isolated splenic vein obstruction can cause congestive splenomegaly. Secondary findings can help to differentiate the cause. Splenomegaly with liver surface nodularity suggests the diagnosis of liver cirrhosis. Splenomegaly with multiple subcutaneous venous collaterals may suggest MOIVC. Splenomegaly associated with pancreatic mass is suggestive for isolated splenic vein occlusion.
23.1.2 Hyperplastic Splenomegaly
Hyperplastic splenomegaly results from the normal sequestration of increased amount of the abnormal blood cells which are degenerated in the spleen.
23.1.3 Infectious and Inflammatory Disease
Inflammatory splenomegaly is caused by increased reticuloendothelial cell and lymphoid cell proliferation from an increased antigen clearance and antibody production. Abscess formation in the spleen, due to filtered encapsulated organisms, can cause infectious splenomegaly.
23.1.4 Infiltrative Splenomegaly
Infiltrative lesions such as tumor cells (in the case of leukemia and lymphoma), metabolites (in the case of Gaucher’s disease and amyloidosis), and blood cell producing cells (in the case of extramedullary hematopoiesis) can cause splenomegaly.
23.2 Infection
23.2.1 Malaria
Malaria is a protozoan disease associated with infected Anopheles mosquito. CT findings of splenic involvement of malaria include splenomegaly, decreased splenic enhancement, and lack of mottled striped enhancement during the arterial phase. The complications of malaria include spontaneous splenic rupture and splenic infarction.
23.2.2 Tuberculosis
Splenic involvement is usually in the miliary form. Miliary tuberculosis appears as irregular low-density masses in the spleen. Secondary finding including necrotic lymph nodes, high-density ascites, and nodular peritoneal thickening may be helpful. In the later phase, the splenic lesion turns into calcified granuloma.
23.2.3 Brucellosis
Fever, night sweats, fatigue, anorexia, myalgia, and arthralgia are common symptoms of brucellosis. Hepatosplenomegaly, abscess formation, subcapsular hematoma formation, and splenic rupture are findings of splenic involvement of brucellosis. The respiratory involvement can help suggest the diagnosis.
23.2.4 Salmonella Infection
The spleen is one of the most common sites of Salmonella infections, and the manifestations can range from nonspecific organomegaly to an abscess formation and splenic rupture.
23.2.5 Aspergillosis
Splenic involvement of aspergillosis includes diffuse or multifocal wedge-shaped low-density areas or disseminated low-density nodules in the spleen due to the angioinvasiveness of the organism.
23.3 Miscellaneous
23.3.1 Extramedullary Hematopoiesis
Extramedullary hematopoiesis is a compensation of bone marrow dysfunction to make blood cells. It mainly affects the liver and spleen. The signal intensity of the lesion depends on the time of lesion, i.e., the time of iron component. In the active stage, the lesion shows intermediate signal intensity on T1-weighted image, high signal intensity on T2-weighted image with some enhancement after contrast media injection. In the late stage, the lesion may show low signal intensity on T1- and T2-weighted images without definite enhancement. On dual-echo gradient MR, the lesion shows low signal intensity in the in phase of MR due to the presence of iron.
23.3.2 Gamna-Gandy body
Gamna-Gandy bodies are found in about 10 % of patients with splenomegaly. They consist of fibrous tissue with hemosiderin and probably are associated with small perivascular hemorrhages. They show low signal intensity on T1- and T2-weighted images owing to hemosiderin components.
23.4 Summary
1.
Some splenic diseases show discrete image finding, but mainly the imaging findings of the splenic diseases are overlapped and indistinct.
2.
Ancillary findings and clinical histories are very important to differentiate diffuse splenic diseases.
23.5 Illustrations: Diffuse Spleen Diseases
23.5.1 Congestive Splenomegaly
23.5.1.1 Splenomegaly with Liver Cirrhosis
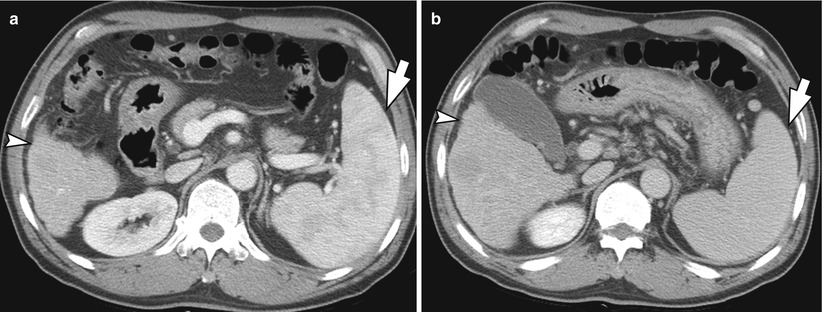
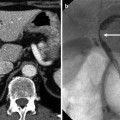
Fig. 23.1
Splenomegaly with liver cirrhosis in a 49-year-old male. (a, b) Contrast-enhanced CT images in portal phase (a) and equilibrium phase (b) show the enlarged spleen (arrow) and surface nodularity of the liver (arrowhead). During portal phase, the spleen still shows so-called zebra-type heterogeneous enhancement. On equilibrium phase image, spleen shows homogeneous enhancement
23.5.1.2 Splenomegaly Associated with Alcoholic Liver Cirrhosis
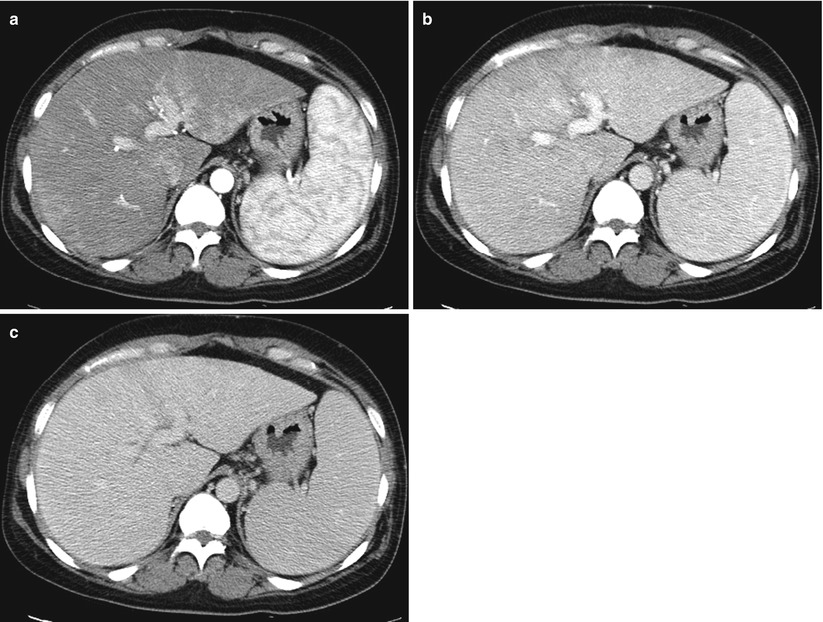
Fig. 23.2
Splenomegaly associated with alcoholic liver cirrhosis in a 57-year-old male. (a) Contrast-enhanced CT image in arterial phase shows inhomogeneous hepatic enhancement with splenomegaly. Note preserved zebra-like splenic enhancement. (b, c) On portal (b) and equilibrium phase (c) transverse CT, the spleen shows more homogenous enhancement. Note the inhomogeneous hepatic enhancement
23.5.1.3 Splenomegaly Associated with Splenic Vein Occlusion
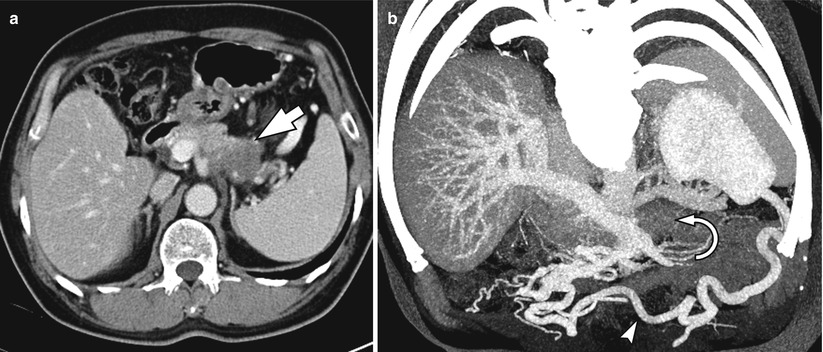
Fig. 23.3
Splenomegaly associated with the splenic vein occlusion in a 50-year-old female. (a




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree