Distal Tibia Fractures
Fractures of the distal tibia are among the most difficult injuries facing the orthopaedic traumatologist. Although both extra-articular and intra-articular patterns occur with varying severity, the common concern in all of these injuries is the associated soft tissue injury. The cause of these injuries is frequently violent, and associated injuries occur commonly. Multiple approaches have been suggested, but there is no consensus regarding the optimal treatment for these injuries and no long-term outcome measures that define the results of either the injury or the treatment.
Most articular fractures of the distal tibial weight-bearing surface are the result of motor vehicle accidents, motorcycle accidents, falls from heights, and industrial injuries. Ankle fractures are usually the result of indirect mechanisms, whereas the majority of pilon fractures are the result of an axial loading mechanism in which the talus is forced cranially and into the distal tibia, thus producing the “explosion” fracture of the articular surface. The position of the foot at the time of impact combined with the direction of the applied force will determine the resultant fracture pattern and articular impaction.
The associated soft tissue injury that occurs is frequently more important than the fracture pattern. These injuries are frequently open, especially on the medial side where the distal tibia is in a subcutaneous location. Swelling occurs rapidly and may be exacerbated by the shortening that occurs. The initial and ultimate treatment decisions should be based more on these associated soft tissue concerns than on the osseous injury. Physical examination of the injured lower extremity should include a careful assessment of the local swelling, perfusion, and neurologic deficits. Fracture blisters, local skin necrosis, and impaired distal perfusion are commonly observed. Early limb realignment to relieve skin pressure from the osseous deformity should be performed. In addition, gross or micromotion at the fracture site should be minimized to allow the soft tissue swelling to resolve.
The initial radiographic evaluation consists of standard ankle and tibial radiographs. Computed tomography (CT) scans should be delayed until limb length has been restored. The value of CT scans in assisting with preoperative planning and fracture understanding has been well demonstrated.1 Similarly, contralateral ankle radiographs are frequently helpful in understanding the unique morphological variations in the distal tibial anatomy and assist with pre-operative planning.
Classification
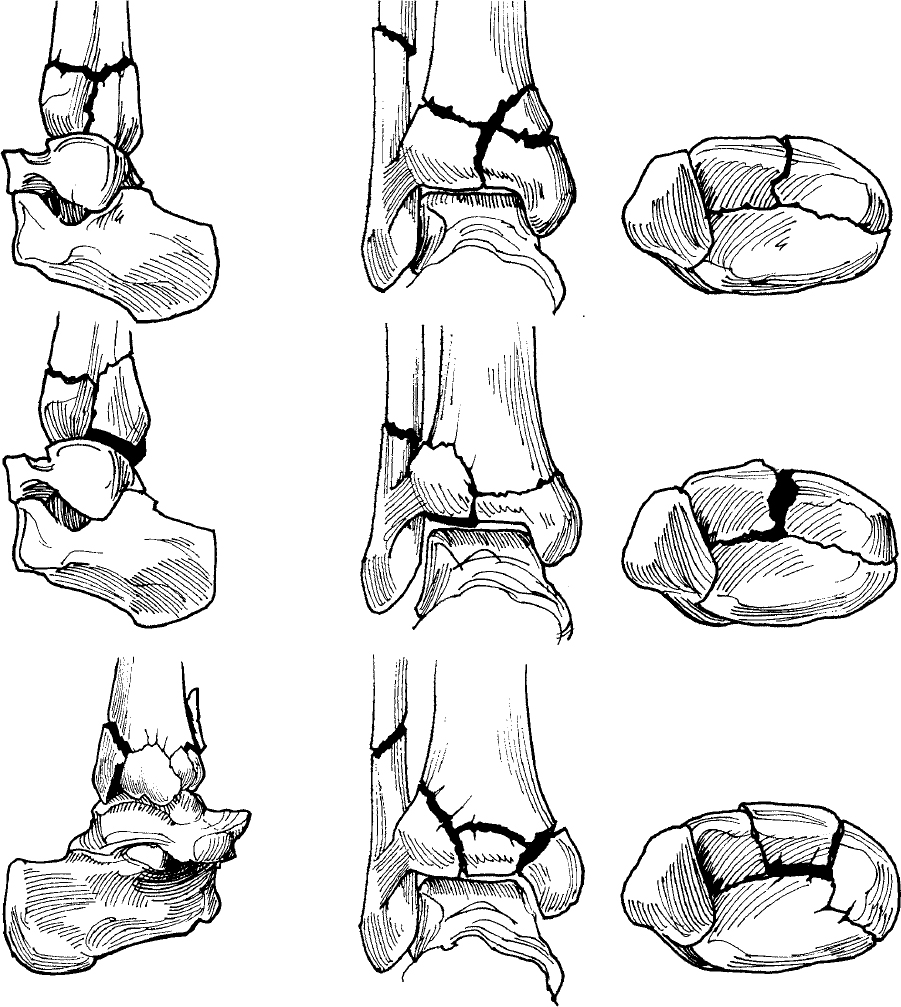
The classification of Rüedi and Allgöwer′s group2 is moderately useful and is divided into three types: type I fractures are nondisplaced, type II fractures are characterized by articular displacement, and type III fractures have associated articular comminution and impaction (Fig. 34.1). The Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification incorporates all fractures of the distal tibia, including extra-articular injuries of the distal tibial metaphysis (Fig. 34.2).3 This classification system is much more detailed, describes comminution at multiple levels, and differentiates between partial and complete articular injuries. Similar to other periarticular fractures described by the AO/OTA classification system, a type A fracture is extra-articular, a type B fracture has partial articular involvement, and a type C fracture has complete (or severe) involvement of the articular surface. However, the reproducibility and usefulness of this classification system have been questioned. Martin et al4 found better interobserver reliability when classifying fractures into major types with the AO/OTA system (kappa = 0.60) than with that of Rüedi and Allgöwer (kappa = 0.46). Agreement at the group level with the AO system remained poor (kappa = 0.38). Similar trends were noted when evaluating intraobserver reliability. Swiontkowski et al5 demonstrated that only moderate agreement (kappa = 0.41 to 0.60) existed with the AO/OTA system, and that determination of the fracture type alone (type A, B, or C) was probably adequate for clinical research. However, for the purposes of describing these injuries and formulating a surgical plan, the fracture group (e.g., C1, C2, or C3) can be helpful.

Nonoperative Treatment
Nonoperative treatment of distal tibial fractures is recommended only for truly nondisplaced fractures or fractures in patients that have an absolute contraindication for surgical management. Such injuries can be effectively managed with closed reduction and cast immobilization followed by progressive weight bearing and ankle range of motion as radiographic healing progresses. The indications for nonoperative management of displaced, articular tibial pilon fractures are extremely limited. Casting is ineffective in reducing any displaced articular segments, and distraction across a shortened ankle joint is not feasible with this treatment method. For example, in displaced partial articular injuries (type 43B) of the distal tibia, nonoperative management is ineffective in reducing the displaced fragment in the majority of these injuries. The articular impaction that is frequently associated with these injuries does not respond to ligamentotaxis and will therefore not be reduced with closed methods. Similarly, in displaced complete articular fractures (type 43C), closed methods are ineffective in accurately reducing the articular segments. In the case of an intact fibula associated with a complete articular distal tibial fracture, varus angulation commonly occurs, and closed methods must counteract this tendency. In similar complete articular distal tibial fractures with an associated fibular fracture, shortening is expected with associated widening of the joint.
Bedridden patients, paraplegics, and patients with significant medical comorbidities precluding prolonged anesthesia are all candidates for nonoperative treatment. Casting of pilon fractures has the distinct disadvantage of inhib iting the necessary and ongoing soft tissue evaluations required in management. Other closed methods such as calcaneal traction may allow serial soft tissue evaluations and provide some joint distraction and ligamentotaxis, but patient compliance and prolonged bed rest are required. Alternatively, an ankle joint spanning external fixator (described later) may be used to provide some stability to the fracture.
Significant joint stiffness is expected after the closed treatment of pilon fractures because healing in an acceptable position requires prolonged joint immobilization. Weight bearing and ankle range-of-motion exercises should be delayed until there is radiographic evidence of healing, frequently requiring at least 12 weeks. Thereafter, progressive weight bearing and mobilization can proceed based on the patient′s comfort in applicable cases.
Surgical Treatment
Video 34.1 ORIF Using a Periarticular Plate
Video 34.2 Locked Plating of a Pilon Fracture
Indications
The indications for surgical treatment are based on the combination of fracture location, fracture pattern, and the associated soft tissue injury. The presence of open wounds, a failure to obtain or maintain adequate alignment, and other extremity injuries are among the indications for operative fixation. Displaced or unstable extra-articular distal metaphyseal fractures can be effectively treated with several surgical techniques, including external fixation, open reduction and plate fixation, percutaneous reduction and minimally invasive plate fixation, medullary nailing, or combinations thereof. The condition of the surrounding soft tissues should help direct the choice of treatment, each of which has specific advantages.
Articular incongruity and talar subluxation are poorly tolerated at the tibiotalar joint. Although there are no strict guidelines for determining how much articular step-off or gap can be tolerated, a visible incongruity at the tibial plafond that is demonstrated on plain radiographs should be considered an indication for operative reduction and fixation in properly selected patients. Nondisplaced fractures may similarly require operative fixation if early motion of the ankle is desired.
General Approach to Open Reduction and Internal Fixation
After evaluating the patient, the fracture characteristics, and the integrity of the soft tissue envelope, operative fixation of a pilon fracture can proceed. The overall treatment approach typically consists of a staged protocol with primary restoration of tibial length followed by a delayed reconstruction of the articular surface.6,7 The basic principles outlined by Rüedi and Allgöwer8 over 35 years ago continue to direct our treatment of these injuries. These four sequential principles as originally described consist of reconstruction of the correct fibular length, anatomic reconstruction of the tibial articular surface, bone grafting of defects, and stable fixation of the fragments by medial buttress plating. Although some flexibility in treatment is important in these injuries, these tenets remain a good starting point during the formulation of an operative strategy. A combination of newer surgical techniques emphasizing meticulous soft tissue handling, limited approaches, and low-profile periarticular implants have enabled avoiding the common soft tissue problems that followed medial plating historically.
Surgical Anatomy
The relevant surgical anatomy for the fixation of tibial pilon fractures includes osseous, ligamentous, muscular, and neurovascular structures. Because of the complexity of these injuries, multiple surgical approaches are frequently required. Therefore, a thorough understanding of each approach and the associated anatomic structures is necessary to properly care for these injuries. The most frequent approaches used include the anterolateral, anterior, anteromedial, posteromedial, and posterolateral. Direct medial approaches to the distal tibia, because of the subcutaneous nature of the bone in that location, are associated with an unacceptably high rate of soft tissue complications and should be avoided; they are not discussed in this chapter.
An understanding of the basic muscular and tendinous anatomy about the distal tibia and ankle joint is necessary to enable uncomplicated approaches and dissections in safe planes. The anterior tibial compartment contains, from medial to lateral, the tibialis anterior, the extensor hallucis longus (EHL), the extensor digitorum communis (EDC), and the peroneus tertius. These muscles are all innervated by branches from the peroneal nerve proximally in the leg, enabling distal approaches that are medial, lateral, and between these muscles. The deep peroneal nerve and the anterior tibial vessels are located between the EHL and EDC distally, requiring direct identification and protection in the direct anterior approach. The superficial peroneal nerve is purely sensory and travels from posterior to anterior, crossing the anterolateral surgical incision (Fig. 34.3). The peroneal muscles (longus and brevis) occupy the lateral compartment of the leg, have a distal muscle belly posteriorly, and are firmly attached at the distal fibula by the peroneal sheath. The deep posterior compartment muscles are largely tendinous at the level of the ankle joint and include the posterior tibial, the flexor digitorum communis, and the flexor hallucis longus (FHL). The FHL has a very distal muscle belly, and its identification is especially useful in the posterolateral approach to the distal tibia. The gastrocnemius and soleus muscles have a common tendinous insertion at the level of the ankle joint, and their tendon sheath requires protection in any posterior approaches. The tibial nerve and the associated vascular supply posteriorly require protection and identification during posteromedial surgical exposures (Fig. 34.4).


An understanding of the ligamentous attachments at the ankle joint is particularly useful when considering displacement patterns and planes of safe surgical dissection. Frequently, the important ligaments of the ankle remain largely intact after a pilon fracture, producing the commonly observed major fracture segments consisting of the posterolateral (Volkmann′s) fragment, the anterolateral (Chaput) fragment, and the medial fragment. As the complexity increases, the number of fragments and the associated comminution increase. However, these three major fragments are observed as a component of most C-type tibial pilon fractures. These fragments typically retain connections with portions of the deltoid (medial fragment or malleolar segment), anterior tibiofibular (Chaput segment), and posterior tibiofibular ligaments (Volkmann′s segment). Any surgical approach chosen should respect any remaining ligamentous attachments to these structures.
The relevant osseous anatomy of the tibial pilon includes the distal tibia, the distal fibula, and the talus. The fibula extends distally relative to the tibia, and is firmly attached by the anterior and posterior tibiofibular ligaments. This anatomy becomes most relevant when considering a treatment strategy for accurately reducing the tibial articular surface. Any change in either the length or the rotation of the distal fibula will be reflected in the anterolateral and posterolateral segments of the distal tibia. Similarly, because of the intimate articulation between the tibia and fibula at the distal tibiofibular joint, angular deformity of the distal fibula in any plane will have implications on the tibial reduction. The distal tibial articular surface is centrally concave with associated posterior and anterior extensions.
The posterior tibial articular surface extends more distally, making a posterior arthrotomy for joint inspection impractical. Although the anterior tibia extends over the dome of the talus, the entire articular surface of the tibia can be viewed from any of the anteriorly based approaches. The relevant anatomy of the talus includes an understanding of the nonarticular portions because these can be used for placement of Schanz pins that are useful in distraction across the ankle joint. Laterally, there is significantly more room available at the talar neck than on the medial side.
The combination of fracture pattern, associated soft tissue condition, open wounds, patient comorbidities, and surgeon comfort determines the surgical approach(es) to be used. Open wounds may or may not be extended as a component of the surgical approach. Frequently, the soft tissues are the most traumatized over the distal tibia, and avoidance of incisions in this region may prove prudent. One of the most important factors in choosing the appropriate surgical approach for a given injury is the location of the fracture lines and the associated comminution.9,10 The most frequently used approaches for articular injuries are the anterolateral and the anteromedial.
Surgical Approaches and Techniques
Urgent Management Including Open Fracture Treatment
Video 34.3 Ankle-Spanning External Fixator
The initial surgical management of tibial pilon fractures requires planning for subsequent procedures based on the injury pattern, associated open wounds, and soft tissue swelling. If open reduction is anticipated, reestablishment of the length of the tibia and fibula is necessary. This assists with resolution of soft tissue swelling, and it also ensures that the definitive open reduction will not require an acute intraoperative limb lengthening.
Fibular fixation (if fractured) is a necessary component of the initial surgical management for three reasons. First, an accurate reestablishment of the proper fibular length and rotation indirectly reduces the tibia due to the strong ligamentous attachments, as already noted. Second, this provides a stable lateral column that a medially based external fixator can be tensioned against to correct any persistent shortening and angulation of the tibia. Third, and most importantly, an accurate fibular reduction maximally reduces the posterolateral tibial articular segment through the posterior tibiofibular ligaments, facilitating later open reduction. The surgical approach for fixation of the fibula should be in a posterolateral location, posterior to the palpable back border of the fibula. This location enables the use of this same incision if a posterolateral approach to the tibia is later chosen, and increases the soft tissue bridge if an anterolateral exposure is required for tibial fixation. Additionally, a posterolateral incision is not located directly over the subcutaneous fibula, helping to minimize wound complications in this location.
Fibular fixation is dependent on the location and the mode of failure. Transverse fractures at the ankle joint line are the result of tension forces on the fibula. Conversely, comminuted or wedge fractures proximal to the ankle joint line are typical of valgus overload compressive fractures. The majority of fibular fractures can be treated with a direct open reduction. In some highly comminuted fibular fracture patterns that are not amenable to direct reduction techniques, indirect reduction of the fibula is accomplished. In these instances, no attempt is made to reduce every small cortical fragment, but simply to correct length, rotation, and angulation of the distal fibula. The importance of an accurate reduction of the fibula cannot be overemphasized. Indirect techniques to regain length may be necessary, especially in high-energy pilon fractures with significant shortening and soft tissue swelling. Useful techniques in difficult or comminuted cases include preliminary application of a medial (tibia to calcaneus) external fixator or femoral distractor to regain length, distal fibular plate fixation with application of a proximal push screw to regain length, and application of a small distractor directly to the fibula (Fig. 34.5). Precontoured plates may be helpful in a minority of extremely difficult cases because the distal rotation of the fibula can make straight plate applications difficult.

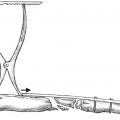
A variety of configurations for ankle-spanning temporary external fixation have been described and work effectively. Some important principles include placement of all pins remote from any anticipated surgical incisions, avoidance of pin placements into the talus if any anterior exposure is planned, and pin placement into subcutaneous locations to minimize pin-site irritation and drainage. Additionally, the external fixator should maintain the foot out of plantar flexion in a neutral position (Fig. 34.5). One successful strategy involves construction of a medial triangular external fixator that relies on an intact or plated fibula, against which tension can be applied. The anticipated pin locations are at the medial tuberosity of the calcaneus, transversely in the midfoot into the cuneiforms, and at the anteromedial face of the tibia (two pins) proximal to any subsequent plate applications. After placement of the proximal 5-mm bicortical tibial pin (perpendicular to the anteromedial face of the tibia) and the 5-mm calcaneal tuberosity pin (parallel to the distal tibial coronal plane articular surface), length and coronal alignment can be obtained. Often, even when the fibula is “out to length,” the medial column is still short. This can be corrected via the following:
Manual traction, distracting between the proximal tibial and distal calcaneal pin
Use of the articulating distractor-compressor clamp, which can aid in gaining length in a controlled manner (Fig. 34.6)

During provisional external fixation, the sagittal plane translational and angulatory deformities of the lower leg can also be improved with strategically placed bumps (beneath either the foot or the leg). A 4-mm pin placed transversely across the midfoot from medial to lateral in the cuneiforms is attached to the proximal tibial pin and maintains the foot in a neutral position. Finally, an additional pin is placed into the anteromedial face of the tibia to prevent rotation around the proximal pin. The talus should be accurately reduced and centered in line with the central axis of the tibia (Fig. 34.7).

An alternative external fixation scheme involves the use of a centrally threaded 5-mm pin at the calcaneus. Excellent control of the alignment of the foot in all planes can be obtained by attaching rods to both sides of the foot using a long pin placed through the calcaneal tuberosity. This frame configuration is especially useful in patients who are treated late (and require bilateral distraction to regain length) and in those injuries where the fibula cannot be fixed at the initial operative procedure. Stabilization of either or both the midfoot and the forefoot is still required to maintain the foot in neutral dorsiflexion.
Open fractures require careful preoperative planning about the placement of incisions for the surgical extension of open wounds to enable an adequate debridement. Most commonly, associated open wounds are located medially. If the open wound is small, an anticipated surgical approach, even if completely remote from the open wound, can be used for the initial irrigation and debridement. If the open wound is large, proximal and distal extensions over the anteromedial face of the distal tibia should be avoided whenever possible. Consistent with the traditional principles of open fracture management, completely devitalized cortical (diaphyseal) fragments require removal. However, every effort should be made to retain all articular segments, irrespective of the soft tissue attachments. If a defect exists after debridement, consideration should be given to placement of antibiotic beads until the time of definitive fixation.
There are situations in which primary definitive fixation of an open pilon fracture may be performed (Fig. 34.8). In these cases, clamp application, fracture reduction, articular lag screw fixation, and plate application are all accomplished through the open wound without additional soft tissue stripping. However, the prerequisites of such an approach include the following:

A complete understanding of the injury, the fracture pattern, and the associated articular involvement
Confidence that a thorough debridement of the open injury has been done in a timely manner
An understanding of the techniques through which the surgeon can reduce and internally fix portions of the injury with “minimally invasive” methods
A well-rested and appropriate surgical team
If any of these prerequisites for this approach are not met, then a staged protocol consisting of primary fibular plating and external fixation across the ankle joint combined with further debridement and wound closure at a secondary procedure is indicated.
Preoperative Planning
The formulation of a cogent preoperative surgical plan begins with the evaluation of the injury films. Several factors contribute to increasing complexity in these injuries and include proximal fracture extensions, multiple articular fragments, impacted segments, bone loss, and osteopenia. The injury radiographs should be evaluated to determine the primary deformity pattern because this in turn determines the final fixation construct and hence the surgical approach(es) necessary. For example, if the original injury film demonstrates significant varus angulation of the distal tibia, a medial buttressing implant is likely indicated to counteract the inherent tendency for this injury to fail back into varus. Review of the fibular fracture characteristics, combined with the coronal plane angulation of the tibia, provides visual clues regarding the areas of compression and tension failure. Occasionally, the injury radiographs demonstrate a purely axial failure of the tibia with or without fibular failure. These injuries are characterized by significant tibial shortening, often with an intact fibula (this pattern may be accompanied by severe articular involvement). The more commonly observed fracture combinations are varus angulation of the tibia combined with tension failure of the fibula, and valgus angulation of the tibia combined with compressive failure of the fibula. Consideration of tension versus compression failure has implications from a biomechanical standpoint when fixation is considered. Buttress plating is frequently required on the compression failure side, especially if bone contact after reduction is compromised due to cortical impaction. Conversely, large implants are rarely needed to support cortical bone that has failed in tension if the compression failure side has been supported.
Computed tomography is essential for the evaluation of the injuries. However, if a staged protocol for fixation is planned (immediate fibular stabilization and ankle spanning external fixation followed by definitive internal fixation as the soft tissue swelling permits), these scans should be delayed until after spanning external fixation has been applied to regain limb length. An exception to this is the situation where the surgeon wishes to internally fix the “simple” articular injury through the traumatic open wound as already noted. CT scans obtained with the extremity in its initial shortened position are frequently of low value due to significant displacement of the fracture fragments and talar shortening. If scans are inadvertently obtained prior to reestablishment of tibial length, they frequently need to be repeated because the overall position of the fragments changes significantly. The axial images are the most useful and provide identification of the major articular fragments, cephalad articular impaction, and regions of comminution and fragmentation. The sagittal and coronal reformations provide additional data, especially for identifying impacted segments that are rotated relative to the axial images.
After identification of all the fracture fragments on the CT scan, the findings can be correlated with the findings of the plain radiographs obtained after length has been reestablished. The surgical incisions and implants can then be planned based on the data obtained from the CT scan(s) and the injury radiographs. This should include consideration of the primary failure mode and the translational and angular deformities of the distal tibia (e.g., varus or valgus; anterior translation of the talus relative to the tibial plafond). Locking plates are of minimal use in most distal tibial pilon fractures. However, in cases of severe metaphyseal impact, metaphyseal bone loss, or osteopenia, there may be a role for these implants. Regardless of whether locked plates are used, compression of the articular surface with lag screws (either independently or through a plate) should be performed. For the vast majority of articular fractures unlocked plates combined with screws provide adequate support. A variety of instruments are helpful for reduction and fixation of pilon fractures (see text box).
Tourniquet Use
The use of a tourniquet in articular fractures of the distal tibia is not optional and is preferred in most circumstances. Limb exsanguination and tourniquet application assist with visualization within a bloodless field. Following the articular reduction, use of the tourniquet can be discontinued. Typically, a low pressure (200 mmHg) is used to minimize tissue ischemia.
Anterolateral Approach for Reduction of Tibial Pilon Fractures
The anterolateral approach (Fig. 34.9) is useful in the majority of complete articular (type 43C) pilon fractures, anterior and anterolateral partial articular (type 43B) pilon fractures, and some extra-articular distal tibial fractures that can be stabilized with a plate slid beneath the anterior compartment (Fig. 34.10). The anterolateral approach has the advantage of excellent visualization of the articular surface to the medial shoulder of the ankle while avoiding dissection of the anteromedial tibial face. Impaction at the medial shoulder is difficult to reduce with this exposure. Proximal extension of the incision is limited as well. The approach facilitates accurate articular reduction combined with submuscular and subcutaneous plate applications spanning the metaphyseal comminution.


Equipment Used for Open Reduction and Internal Fixation of Pilon Fractures
Medium femoral distractor (used to distract between the talus and midshaft of the tibia to enable visualization of the distal tibial articular surface)
Dental picks
Large pointed reduction clamps
Medium pointed reduction clamps
Small pointed reduction clamps
Kirschner wires (K-wires) of varying sizes
2.5-mm terminally threaded pins as joysticks
Small-fragment screws (2.7 and 3.5 mm; with long lengths, e.g., 60 to 80 mm)
Mini-fragment screws (2.0 and 2.4 mm; with long lengths, e.g., 40 mm)
Headlight to visualize the articular surface
Multiple plates consistent with the screws and preoperatively planned bone tamps
Allograft bone chips (as necessary) versus a bone graft substitute
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree