4.1 Introduction
Conventional radiotherapy and radiosurgery differ in many ways, but the most significant distinction is the time-course of radiation dose delivery. Conventional radiotherapy is delivered in multiple, relatively small dose units, or fractions, over the course of several weeks. Radiosurgery is delivered in only a few, high-dose units, or sessions, over a few days. Pre-clinical and in vitro studies established the efficacy of single-fraction radiation delivery for cell killing. A large body of clinical evidence now exists to support the effectiveness of radiosurgery for a variety of intracranial conditions. Minimizing radiation-induced normal tissue injury resulting from radiosurgical treatment is an equally important facet of clinical management.
4.2 Radiobiology
Conventionally, fractionated radiotherapy is governed by four fundamental principles of radiobiology: repair, redistribution, repopulation, and reoxygenation.
- ▪
“Repair” refers to the ability of normal cells to recover from the sublethal injury induced by small doses of radiation more readily than tumor cells.
- ▪
“Redistribution” refers to the effect of ionizing radiation on the cell cycle of dividing cells, causing them to temporarily pause in the G2 phase of mitosis, which renders them more susceptible to radiation injury.
- ▪
“Repopulation” refers to the ability of both normal and tumor cells to continue cell cycle division once radiated.
- ▪
“Reoxygenation” refers to the decrease in hypoxic regions within a tumor as a result of radiation-induced cellular changes, rendering the tumor more susceptible to radiation injury.
The relevance of these four principles to the biological effects of radiosurgical treatment is notably less defined. Whether single-session or multisession, the higher doses delivered per session during radiosurgery are more likely to result in lethal injury, rather than sublethal injury, to both normal cells and tumor cells. Therefore, the guiding principle of any radiosurgical treatment is avoidance of dose to adjacent normal tissues (organs at risk) whenever possible.
4.3 Normal structure identification and contouring
Critical to the success of radiosurgical treatment is the ability to clearly identify and delineate a target lesion or area of interest on proper imaging studies. Similarly important is the task of identifying and delineating all adjacent tissues or normal structures that could receive a dose during radiation delivery. This includes all anatomic structures immediately adjacent to or abutting the target area, as well as surrounding structures near the target. The radiation dose decreases exponentially with distance, so the further away any normal tissue is from the target area, the less dose it will receive.
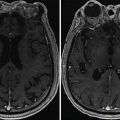
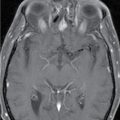
Normal tissues/organs at risk that are generally contoured for skull base radiosurgery cases include both eyes, both optic nerves along their entire pathway, optic chiasm, pituitary gland, brainstem, one or both cochlea, cranial nerves in close proximity to the target, whole brain, and scalp/skin ( Figures 1.4.1 , 1.4.2 ) . Figure 1.4.2 shows a dose-volume histogram, graphically describing the volume of a structure that receives a specific dose. Note that in many skull base cases, the expected anatomic location or appearance of adjacent normal structures may be altered, either by the target lesion itself or by prior surgical interventions. Extra time and attention from both the neurosurgeon and radiation oncologist is necessary in these cases to ensure a successful outcome.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree