, Valery Kornienko1, Alexander Potapov2 and Igor Pronin3
(1)
Department of Neuroradiology, Burdenko Neurosurgery Intitute, Moscow, Russia
(2)
Department of Neurotrauma, Burdenko Neurosurgery Insitute, Moscow, Russia
(3)
Department of Neuroradiology, Burdenko Neurosurgery Institute, Moscow, Russia
Abstract
There are only a few papers devoted to studying of cerebral blood flow by CT perfusion in severe traumatic brain injury, with first publications appearing recently. However, no data are available on dynamic CT perfusion of the regional cerebral blood flow in hemispheric structures, subcortical formations, and brain stem in comatose patients at different stages of consciousness recovery.
In this work CT perfusion was used to evaluate the regional cerebral blood flow with regard to focal and diffuse morphological changes of the brain in severe trauma. Our studies showed that mosaic and multidirectional alterations of the cerebral blood flow may range from oligemia-ischemia in one vascular region to hyperemia in the other in dynamics of the traumatic brain disease. All patients in the analyzed group revealed regional cerebral blood flow values beyond the normal range in the first and repeated CT perfusion examinations.
Quantitative blood flow parameters in the brain stem have been studied by CT perfusion in comatose patients, with regard to dynamics of the traumatic brain disease and its outcome.
This chapter has been contributed in collaboration with Eugenia Alexandrova and Gleb Danilov.
6.1 Clinical Material
24 patients with TBI caused by a traffic accident (13), blow to the head (7), falls from height (3), and blind penetrating wound (1) were included into the analysis. Patients’ age ranged 6–49 (average 32.5 ± 13), 16 of them were male and 8 female; 21 patients had an admission Glasgow Coma Scale (GCS) score of 4–8 (6.4 ± 1.5) and 3 patients had GCS of 9–11. Dynamic evaluation revealed that 21 patients had length of coma ranging 3–20 days (average 9.8 ± 4 days); 10 patients had a lucid interval after trauma.
On admission CT data analysis revealed cortical-subcortical contusions in 22 cases, signs of diffuse brain injury in 11 cases. All patients showed CT signs of subarachnoid hemorrhage and different degrees of compression or deformation of mesencephalic cisterns, and 10 patients had a lateral midbrain shift. Outcome analysis by GOS showed that only 10 (42 %) patients had favorable outcome (moderate disability or good recovery), 14 (58 %) unfavorable outcome: severe disability (11), vegetative state (1), and death (2).
The first rCBF study was performed within the first 1–3 days following TBI in 12 patients, within 4–8 days in 8 patients, and within 12–14 days in 4 patients. The second rCBF evaluation was performed within 5–14 days after trauma in 14 patients, within 15–34 days in 9 patients, and on the 60th day in one patient. Regional CBF was evaluated four times in one patient – the third and fourth studies were performed in 4 and 6 months following TBI due to development of hydrocephalus. In another patient CT perfusion was carried out three times; the last one in 7 months after trauma and shunting procedure following cranioplasty.
Twenty patients with severe TBI in coma and 4 patients with mild TBI underwent a single CT perfusion study with blood flow evaluations in the brain stem, and 18 patients underwent CT perfusion study in dynamics with ROIs positioning at the region of the midbrain tegmentum and in both cerebral peduncles symmetrically.
Four healthy volunteers without history of a neurological disease or significant head trauma were studied using the same CT perfusion parameters; age range was 21–36 (mean = 30) (Pronin et al. 2007).
6.2 Dynamics of rCBF in Hemispheric Brain Structures
Perfusion CT studies demonstrated average rCBF values exceeding 28.6–69.0 ml/100 g/min in single or multiple vascular regions in 23 patients, with seven of them showing rCBF reduction in one or more vascular regions and its increase in the other regions. A significant correlation was identified between regional cerebral blood flow (rCBF) and cerebral blood volume (rCBV) values (R = 0.8, p < 0.05). For these reasons further analysis was based on rCBF values only.
The lowest rCBF values were obtained in the vascular regions of ACA in the first studies and the following days and weeks after trauma. This tendency toward rCBF reduction in the ACA regions was caused by predominant frontal lobe contusions. Typical rCBF maps are presented in Fig. 6.1. A comparison analysis showed a significant difference (p < 0.05) between average rCBF values in hemorrhagic contusions and in the contralateral hemispheric intact zones.
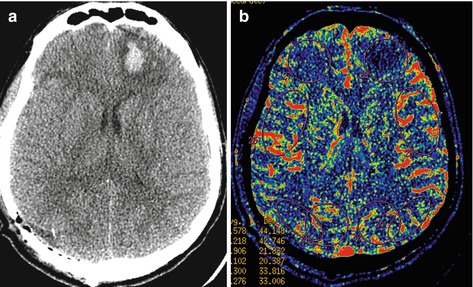
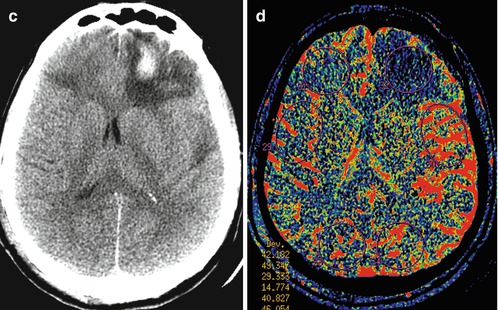
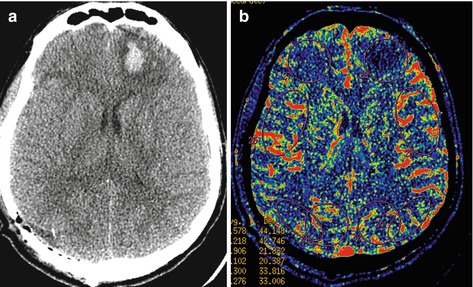
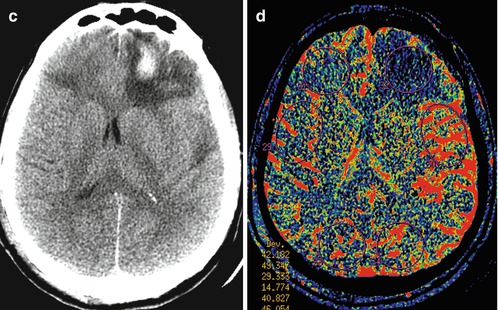
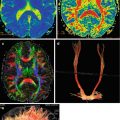
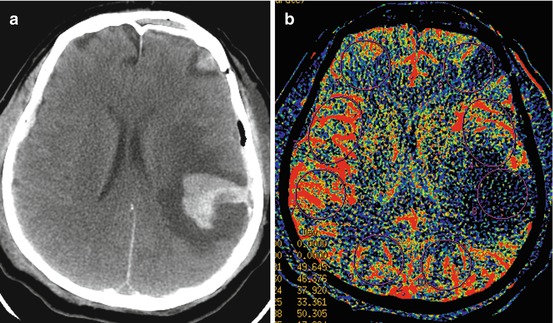
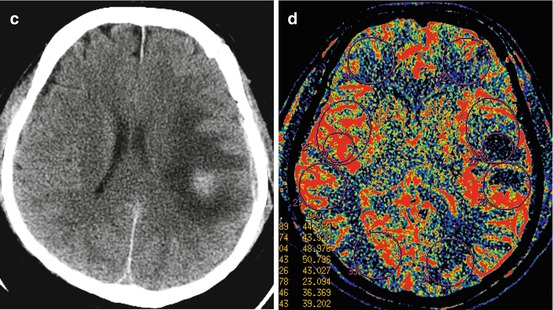
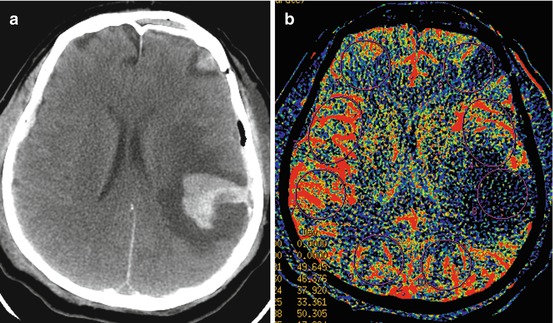
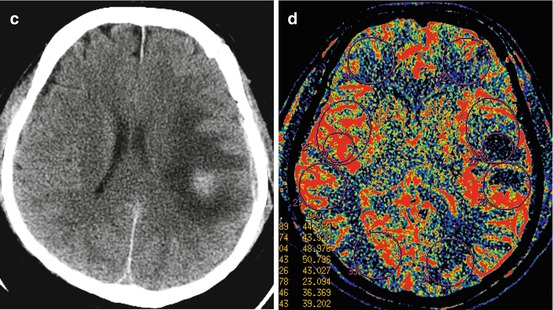
Fig. 6.1
Traumatic brain injury as a result of fall from height. GCS, 7. Outcome, severe disability. Focal contusions of the frontal and temporal lobes. Cerebral perfusion study in 2 (a, b) and 10 (c, d) days after injury and after removal of epidural hematoma in the right parieto-occipital region; rCBF values in the focal contusion area of the left frontal lobe – 8.5 ml/100 g/min
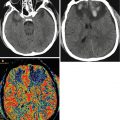
CT scanning in two patients in deep coma at admission (GCS of 4) showed signs of diffuse and focal brain injury followed by hydrocephalus (Figs. 6.2 and 6.3).
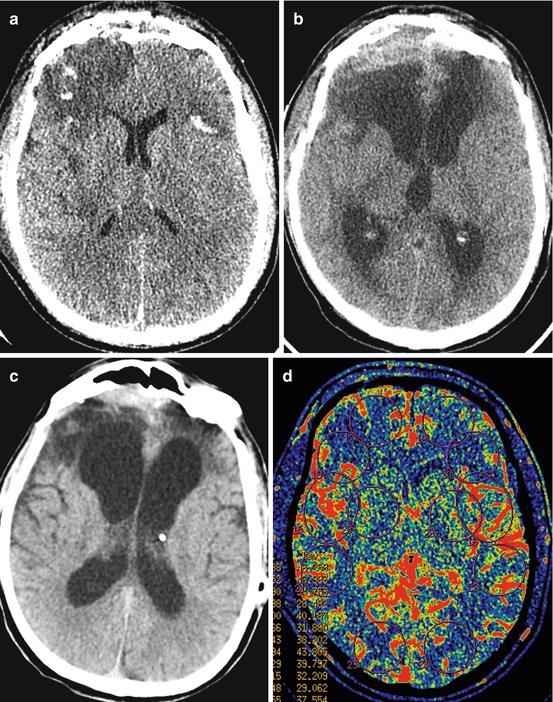
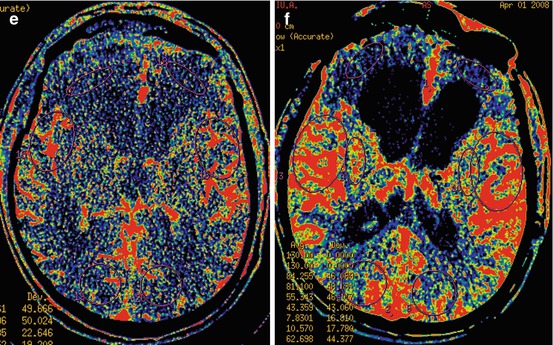
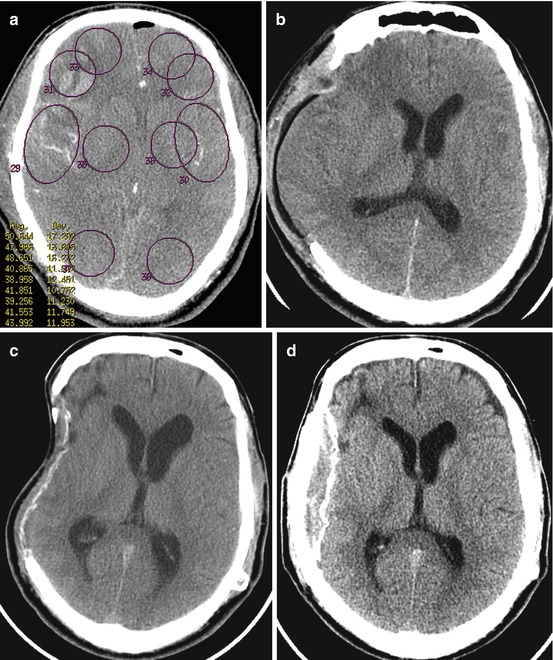
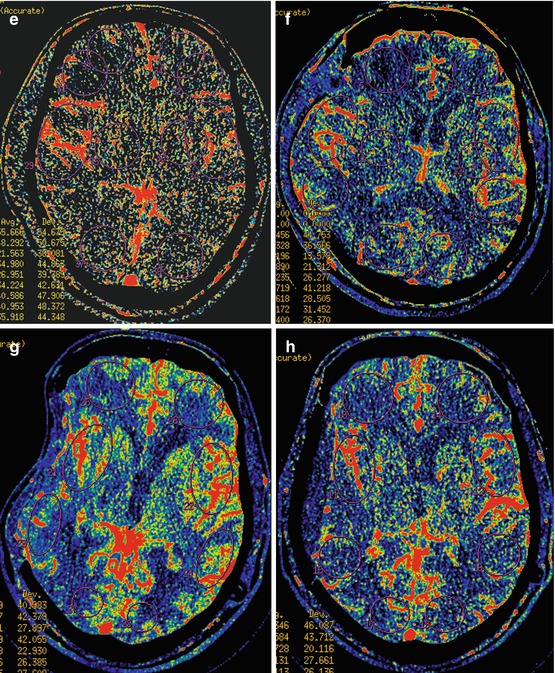
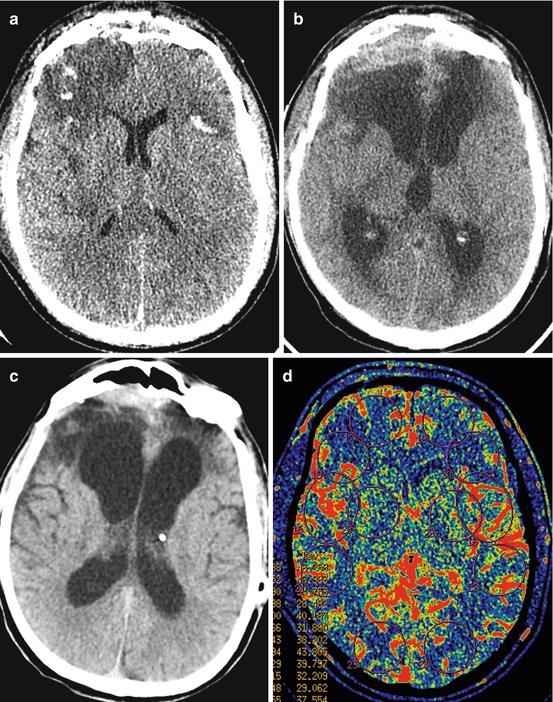
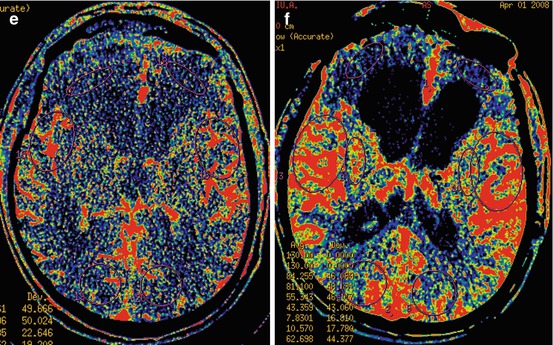
Fig. 6.2
Diffuse axonal injury with focal contusions in the frontal lobe, skull base fractures with a CSF leakage complicated by meningoencephalitis and hydrocephalus. CT and CT perfusion: (a, d) 5 days after injury; GCS, 4; (b, e) 1 month after trauma, vegetative state; (c, f) 6 months after injury, vegetative state (see explanation in the text)
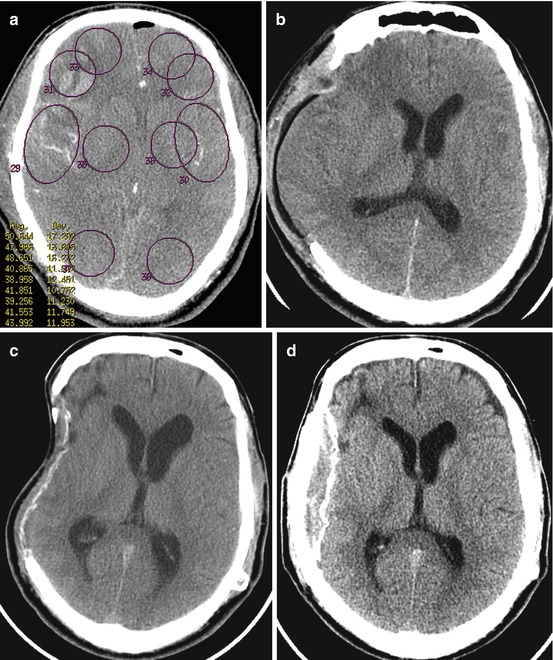
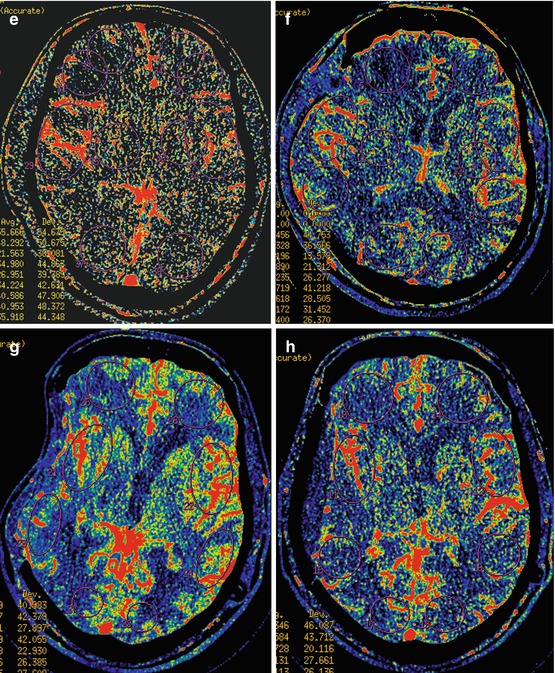
Fig. 6.3
TBI in traffic accident, DAI. GCS, 4. CT and CT perfusion: (a, e) (2 days after trauma), coma, decompressive craniectomy; (b, f) 11 days after trauma, coma, vegetative state; (c, g) 4 months after trauma, minimally conscious state, shunting; (d, h) 7 months, severe disability, cranioplasty (see explanation in the text)
Case Report (Fig. 6.2)
M., 44y.o. Trauma is caused by assault. Diagnosis: diffuse axonal injury combined with hemorrhagic focal contusions in the frontal lobes, epidural hematoma in the left temporal region, linear fractures of the right frontotemporal area, frontal squama spreading into frontal sinus walls, maxillary fracture by type Le Fort II, fractures of lateral and medial walls of both orbits, zygomatic arch on the right, bilateral eye contusion.
On admission: GCS, 4; all brain stem reflexes were decreased, decerebrate rigidity.
Regional CBF values on the 5th day after trauma were 28.5 and 27.0 ml/100 g/min in the left and right ACA regions, correspondingly.
In 2 weeks after TBI, brain stem reflex is activated (blinks, “hippus pupillare,” intact cough reflex, slight horizontal left eye movements).
In 25 days after TBI, osteoplastic craniotomy with plasty of the anterior skull base CSF fistula and removal of chronic subdural hematoma were performed.
In a month after TBI, patient’s state is assessed as vegetative: spontaneous eye opening, oromandibular activity, decreased diffuse muscle tone are preserved. Mostly upper brain stem signs are marked.
In 40 days after TBI, clinical signs of infectious purulent meningitis confirmed by clinical and laboratory data. In 2 months after TBI, meningitis completely regressed; neurological status remains unchanged.
Dynamic CT scans in 2.5 months after TBI revealed increasing hydrocephalus, atrophic changes in frontal lobes. The patient underwent ventriculoperitoneal shunting.
Perfusion CT in a month after TBI revealed rCBF decrease to 14.4 and 10.6 ml/100 g/min, and in 6 months to 7.8 and 10.6 ml/100 g/min in the ACA territories.
In 19 months after TBI in neurological status, akinetic mutism with some emotional reactions, long-term gaze fixation, sitting in bed (for an hour), looking onto the street. Spastic tetraparesis is retained.
The other patient had diffuse and focal brain injury caused by a car accident and was in a deep coma at admission (GCS of 4). On the 2nd day following trauma, rCBF values in the right ACA region were reduced to 17.8 ml/100 g/min (and 28.2 ml/100 g/min – in the left ACA region). On the 4th day patient’s state deteriorated: there were clinical and CT data of brain dislocation. For these reasons, a right-sided decompressive craniectomy was performed which allowed stabilizing patient’s state and minimizing signs of brain shift and herniation. However, the patient remained in a comatose state. Repeated CT perfusion on the 11th day following trauma showed further reduction of rCBF values in both ACA artery regions (7.7 and 15.9 ml/100 g/min, accordingly) (Fig. 6.3). Later on, the comatose state was followed by the vegetative state with development of hydrocephalus which required programmable shunt implantation. The patient’s state slightly improved. He showed signs of partial consciousness recovery with further transformation into minimally conscious state. Control CT studies in 4 and 7 months after trauma demonstrated signs of moderate brain atrophy (mostly in the right hemisphere) with retained rCBF reduction in the right and left ACA regions – 13.4 and 24.4 ml/100 g/min, correspondingly.
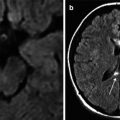
Figure 6.4 shows MRI and perfusion CT data in a patient aged 16, with epidural hematoma and contusion foci in the right temporoparietal region before and after hematoma removal. As is clear from this picture, dynamic examinations visualized the decreased edema and oligemic areas after surgery.
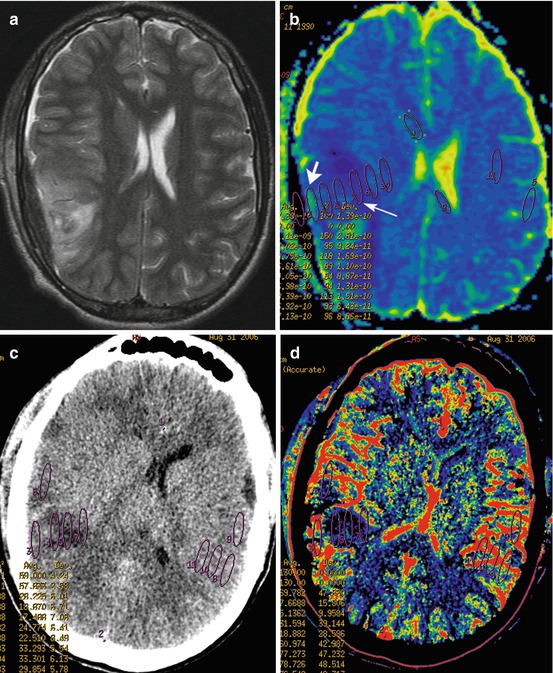
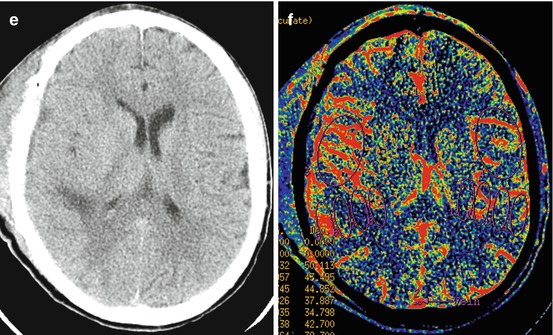
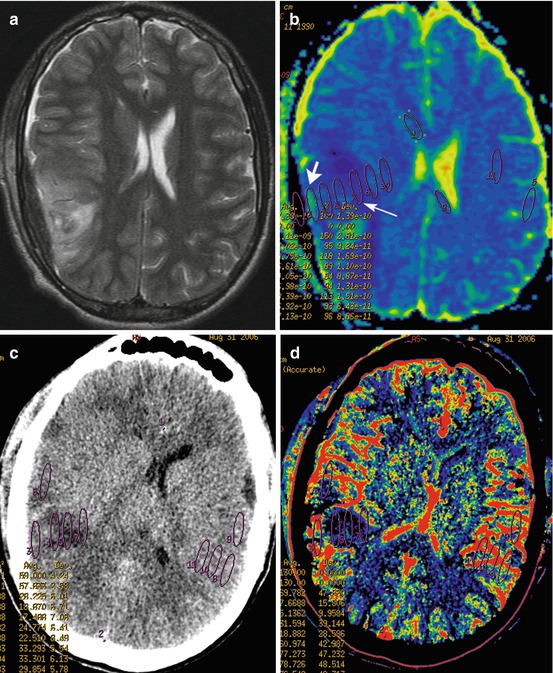
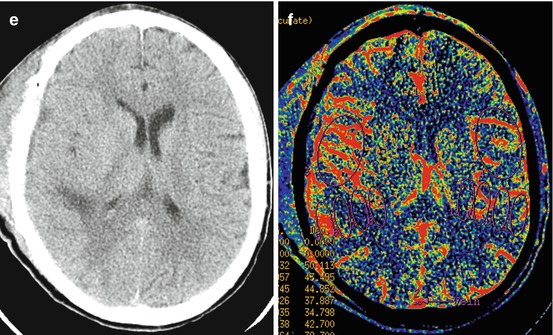
Fig. 6.4
Focal contusion and epidural hematoma in the right temporoparietal region. MRI in 5 days after trauma: T2WI (a); ADC map (b) shows combination of vasogenic (1.1 × 10−3 mm2/c, short white arrow) and cytotoxic (0.4 × 10−3 mm2/c, long white arrow) edema in the perifocal zone of focal contusion. CT and CT perfusion (c, d) in 5 days and 12 days (e, f) after trauma
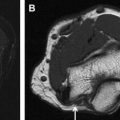
When focal contusions were accompanied by persistent or increasing ischemia, dynamic CT perfusion studies revealed development of cystic-atrophic changes (Fig. 6.5).
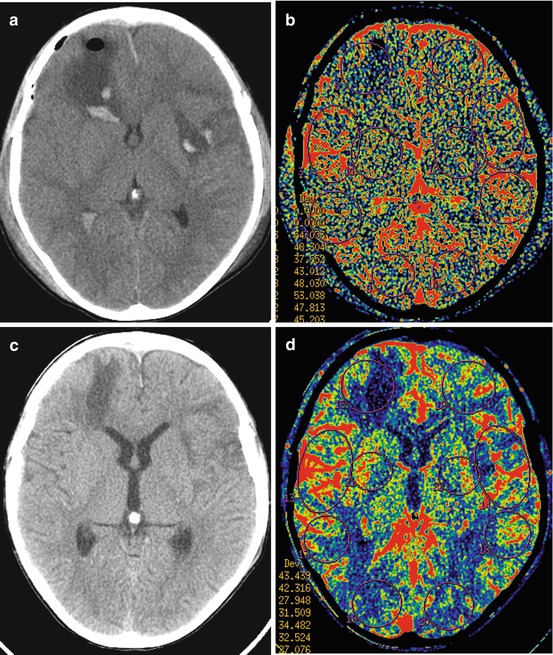
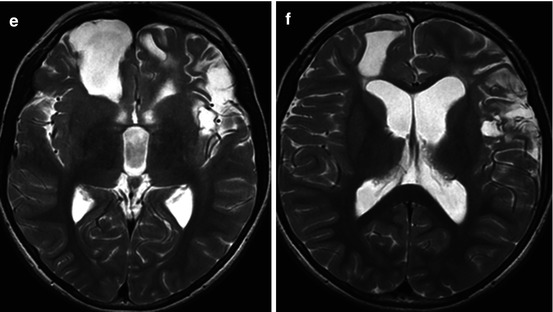
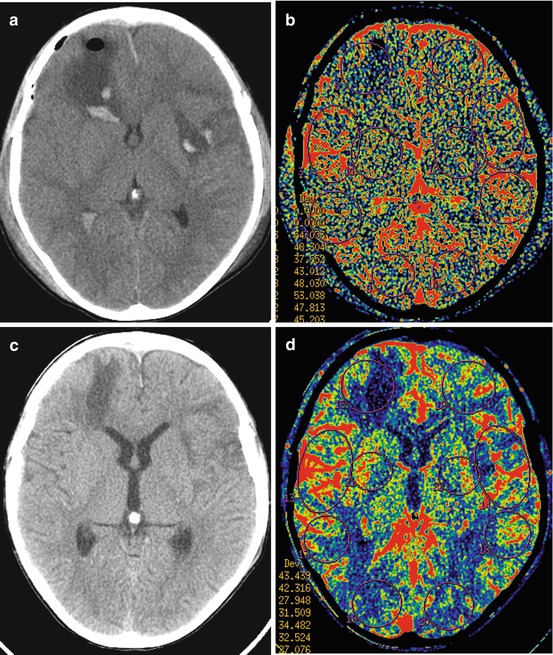
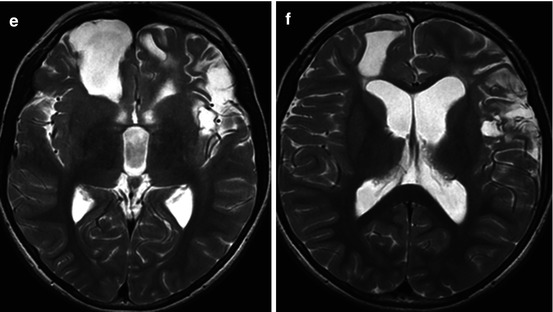
Fig. 6.5
M., 6 y.o. Severe TBI resulting from an object drop on the head. GCS, 8. Coma duration, 8 days. Outcome, moderate disability. CT and CT perfusion (a, b) in 3 days after trauma show hemorrhagic focal contusions in the right frontal and left frontotemporal regions, intraventricular hemorrhage, reduction of rCBF values in the right frontal lobe. CT and CT perfusion (c, d) in 12 days reveal decrease of perifocal edema, further rCBF reduction in the right frontal lobe, appearance of rCBF reduction zones in the left frontotemporal region. MRI study (T2WI, e, f) in 3 years after trauma demonstrates cystic-atrophic areas, which correspond to the reduction of rCBF value areas in CT perfusion studies
Regional CBF increase over 69.0 ml/100 g/min in the MCA vascular region was revealed in 6 patients by initial examination (3–4 days after trauma). Repeated CT perfusion studies (8–13 days after injury) in 3 of them showed preserved rCBF elevation in these vascular regions.
Figure 6.6 shows rCBF dynamics in a patient aged 49 on the 4th and 13th day after injury and subdural hematoma removal in the left frontotemporoparietal region. It visualized rCBF value reduction (below 7.4 ml/100 g/min) in frontal, temporal, and parietal focal contusions in the left hemisphere and rCBF values increase (82.4 ml/100 g/min) in the right MCA region. A repeated CT perfusion study on the 13th day following trauma demonstrated decreased area of hemorrhage and slight regress of perifocal edema and oligemia in the contusion foci. Hyperemia was also decreased in the right MCA region. However, in 6 months following trauma, the patient remained severely disabled with aphasia and right-sided hemiparesis.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree