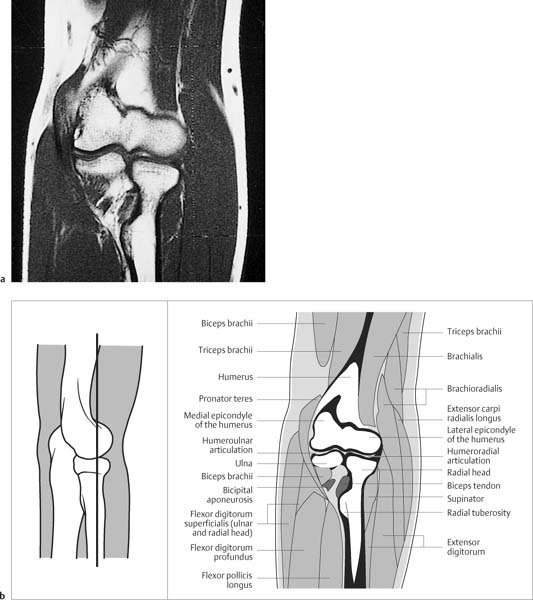
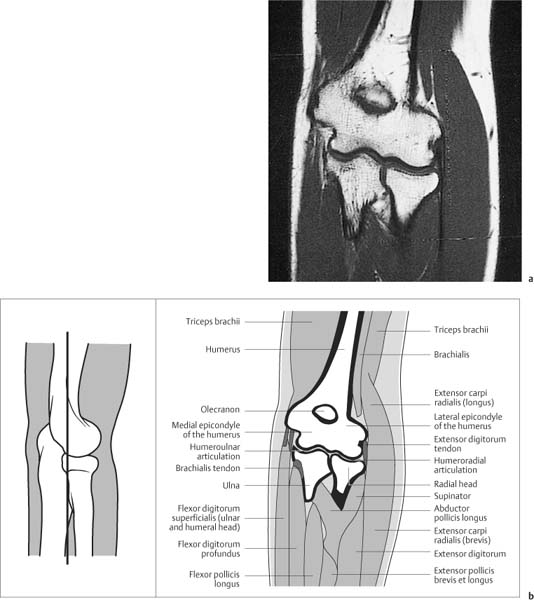
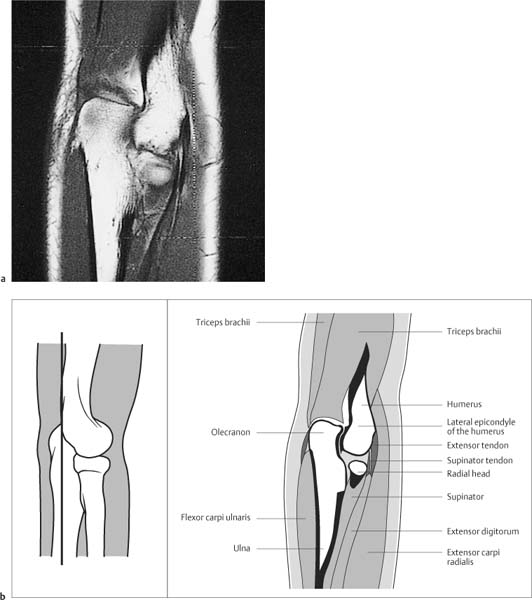
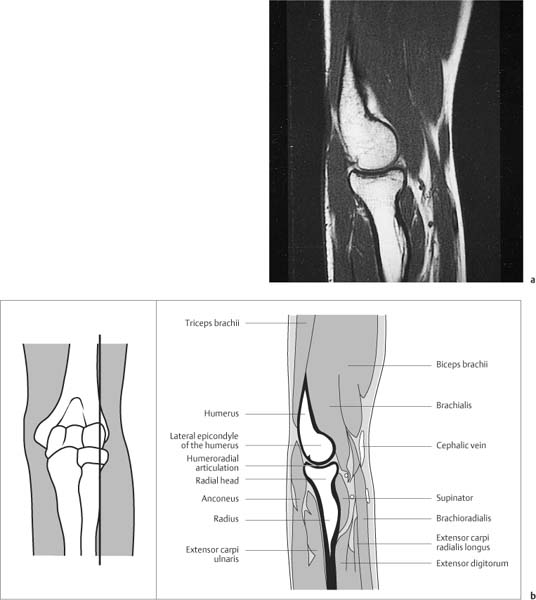
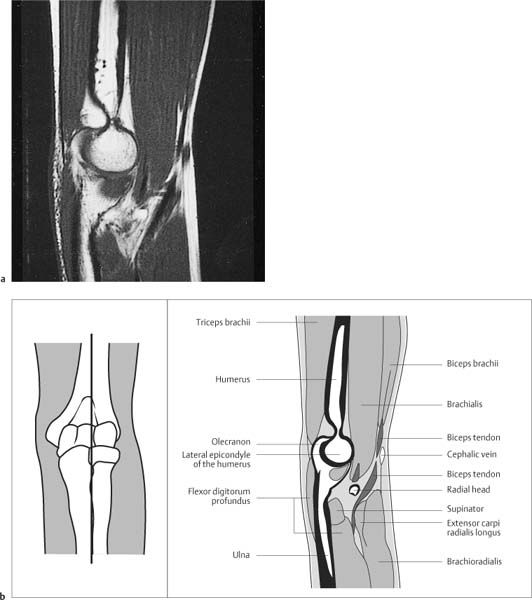
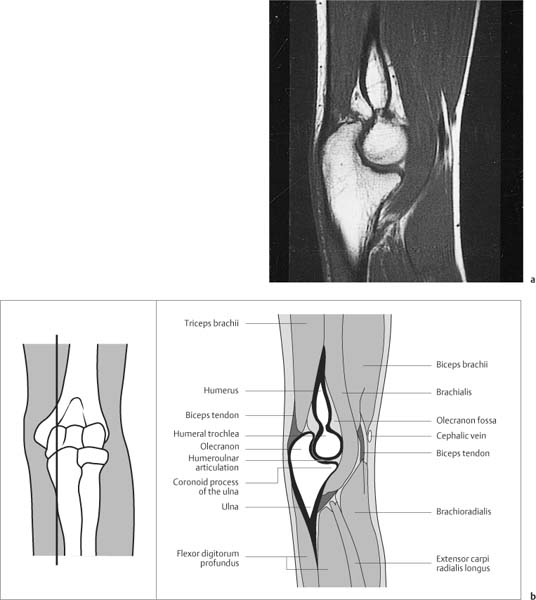
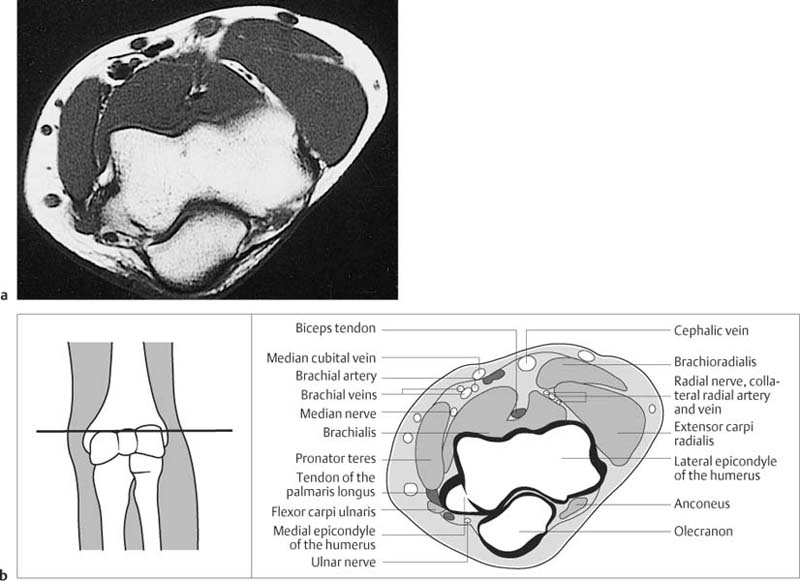
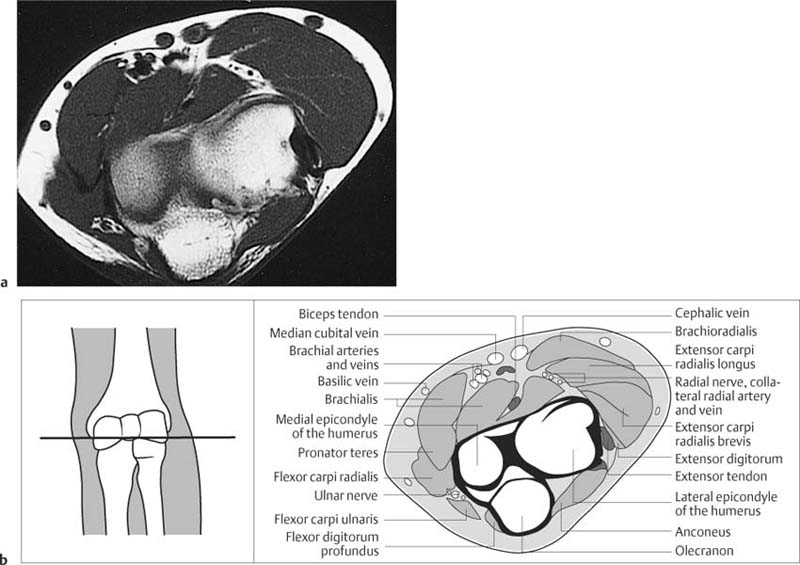
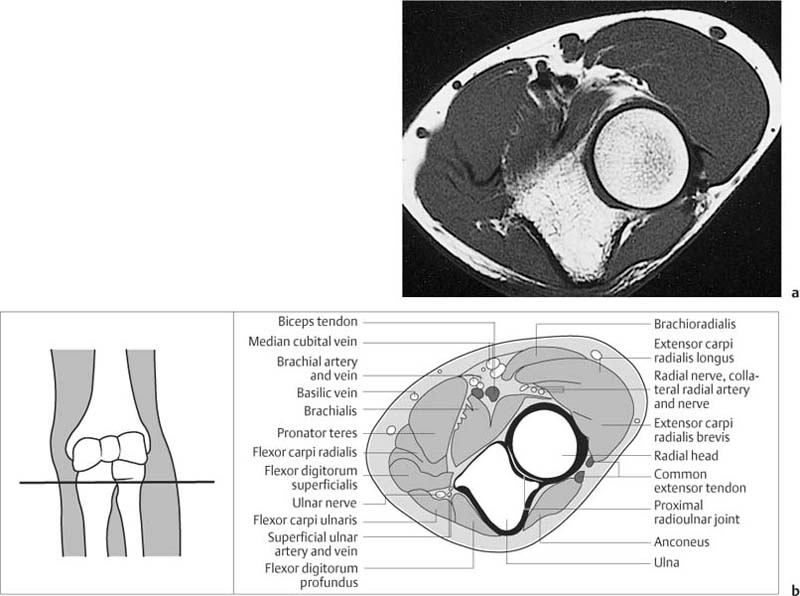
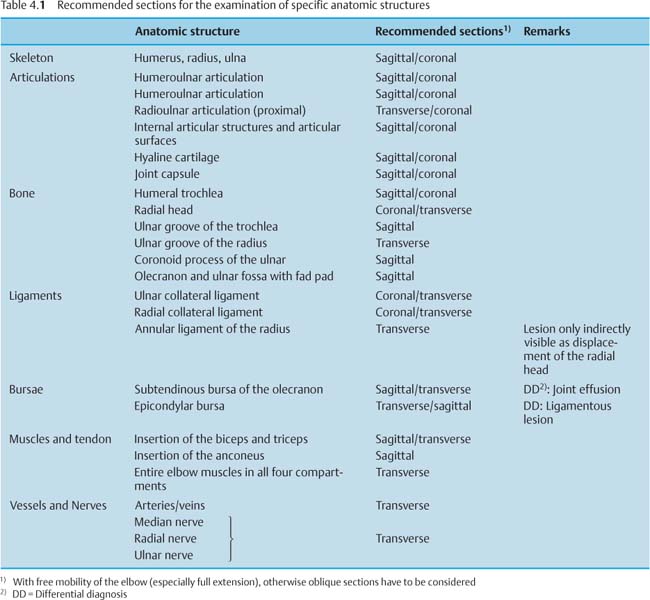
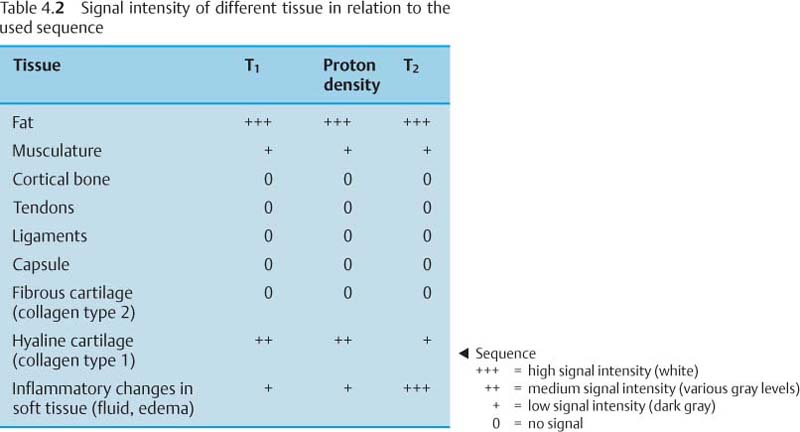
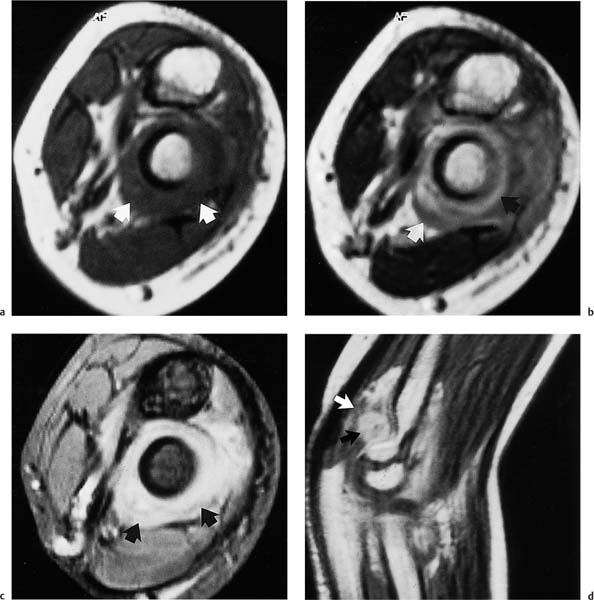
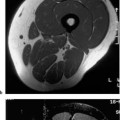
4 Elbow The proliferation of recreational sport and the popularity of sport disciplines involving batting and throwing have increased the number of patients with acute and chronic functional disorders of the elbow. The different mechanical forces acting on the complicated anatomic structure can induce a variety of symptoms. The elbow consists of three separate joint compartments with different planes of movements and is surrounded by muscles, tendons and ligaments. It is often difficult to examine the complicated osseous and soft tissue anatomy with conventional radiography. The advantages of MRI will be shown in comparison to other methods available for imaging the elbow. The increasing role of MRI in diagnostic imaging of the elbow is also reflected in the current literature (10, 11, 12, 13, 14, 23, 24). MRI was rarely applied to the elbow when it was introduced for the evaluation of joints in 1983 and, for a long time, experience in diagnosing pathologic processes in the elbow region was sparse (3, 8, 9, 21). Since then, however, MRI has become an established modality for investigating complaints related to the elbow. Suitable surface coils are now available. With appropriate positioning of the elbow, which can be placed at the side of the body or over the head (if the shoulder is freely movable), sections along the various articulating planes with good contrast visualization of the soft tissues can be obtained. The patient’s position is determined by the available equipment. It should be kept in mind that the patient is more comfortable supine than prone and that the prone position is subject to frequent motion artifacts. In the body coil, the arm has to be elevated above the head, which can be achieved only with an essentially unrestricted range of motion at both shoulder and elbow. It is more comfortable to place the arm along the body with the lower arm in pronation and the palm of the hand resting on the thigh, particularly for longer examinations. Cushions for shoulder and head and a pad underneath the relevant limb improve the patient’s compliance and lower the rate of motion artifacts. The overhead position allows the elbow to be positioned nearer to the isocenter of the magnetic field. This results in more homogeneous fat suppression when chemical fat presaturation sequences are used. The elbow can be positioned with the arm overhead if the patient is placed in an oblique position. However this may lead to further discomfort and increase the likelihood of motion artifact. One study suggests that motion artifacts occur in around 25% of cases when the patient is turned into the oblique position and/or the elbow is placed above the head (2). Whenever the overhead position is used the hand should be immobilized. The design of the MRI gantry limits certain positions, in particular for obese patients. In the majority of cases, it will be most suitable to position the patient supine with the elbow in pronation along the body (4). To encompass the entire elbow, a small off-center field of view (FOV) with a surface coil must be available. When imaging the common flexor and extensor origins for insertional tendinopathy (epicondylitis), the use of coronal images with 20 degrees of elbow flexion has been advocated (5 a). This allows better visualization of the common tendons on coronal sequences. An alternative is a 20 degree posterior oblique coronal plane with the elbow in full extension. This may prove useful when small coils, such as the wrist coil, which prevent the acquisition of images in flexion, are used or when restricted movement of the elbow prevents flexion images being obtained. Alternatively, the elbow can be examined with partial flexion in an extremity coil such as a knee coil. With the elbow in a splint or kept in flexion, a shoulder coil can be used. Applying a pair of surface coils is another measure to offer more comfort to the patient during the examination. Since examinations of the elbow can last up to one hour, anything that might irritate the patient should be avoided. Claustrophobic patients should be adequately premedicated. The patient should be free from any pain (4), should not be thirsty, and should have emptied the bladder prior to the examination. For the examination of the elbow, additional surface coils have been found advantageous. They improve signal-to-noise ratio and spatial resolution. They come in various forms and can be both flat and circular, with a diameter of 8 or 16 cm, or rectangular. Flexible coils are also available. Surface coils are placed over the region to be examined and image the underlying volume close to the surface. A circular surface coil, for instance, encompasses the region it covers and has a regional sensitivity corresponding to its radius. In the majority of cases, the examination begins with a coronal survey view. SE sequence, large field of view (320 – 400 mm) and 256 × 128 image matrix are used to obtain 1 cm thick sections. The imaging time is about ½ minute. Numerous disorders of the elbow can be detected on transverse T1-weighted and T2-weighted images. The transverse sections are generally obtained with T2-weighted sequences because of their excellent soft tissue contrast. The selection of the initial sections is guided by the size of the suspected lesion and the region to be imaged. Using a field of view of 160 mm × 240 mm and a 256 × 256 or 256 × 192 image matrix, the transverse T2-weighted images take about 9 minutes. Fast T2-weighted sequences, such as FSE or TSE sequences, reduce the examination times to 5 minutes. These sequences should be followed by a T1 sequence in the transverse, coronal, or sagittal plane, depending on the clinical symptoms, the anatomic structures to be imaged and the finding on the preceding transverse images. The field of view and the matrix size remain the same as used for the T2-weighted sequences. The imaging time is about 2 – 5 minutes. STIR sequences are best for disclosing small lesions, especially in the bone marrow. STIR sequences take about 25% less time than T2-weighted sequences, although a T2 sequence with fat saturation does provide an alternative to the STIR sequence. Though STIR sequences have a relatively poor signal-to-noise ratio owing to the suppression of the fat signal, pathologic structures frequently are better recognized due to the additive T1 weighting and T2 weighting (7), with an achieved contrast ratio of lesion to fat of 18: 1 and of lesion to musculature of 12: 1. GRE sequences with reduced flip angle and short repetition times (RT) are especially suitable for investigating joint lesions in the different articulating planes. Static GRASS sequences are suitable for examinations of the vascular system (2). It should be emphasized that the protocol of sequences and planes used is usually dictated by the clinical problem to be solved, and the anatomy to be demonstrated (see Table 4.1). The STIR sequences and the chemical shift technique have already been mentioned. The GRE sequences have the capability of three-dimensional display. Cinematic examinations of the elbow with fast GRE sequences are under investigation and have not yet been introduced clinically. Dynamic sequences with IV contrast medium can be helpful for evaluating the activity of inflammatory or tumorous processes. The elbow comprises three parts: • humeroulnar articulation, • humeroradial articulation, • radioulnar articulation. All three articulations communicate with each other and are surrounded by one capsule. They are stabilized by the radial and ulnar collateral ligaments. Moreover, the radial head is encircled by the annular ligament and held against the ulna. Both the coronoid process and the ulnar collateral ligament are crucial for the stability of the elbow. Flexion is achieved by the brachialis, biceps and brachioradialis, and extension by the triceps and anconeus. Pronation is accomplished by the pronator quadratus and pronator teres, and supination by the supinator and biceps muscle. The muscles acting on the elbow can be divided into four groups: • the anterior group: the biceps and brachialis, • the lateral group: the supinator, brachioradialis, and carpal extensors, • the medial group: the pronator teres, carpal flexors, and palmaris longus, • the posterior group: the triceps and anconeus. The brachial artery is the major artery. It is anterior to the brachialis and medial to the biceps, and branches immediately below the elbow into ulnar and brachial arteries. The major nerves traversing the elbow region are: • the median nerve, which is anterior to the brachialis, • the radial nerve, which passes the elbow between brachialis and brachioradialis, • the ulnar nerve, which passes behind the medial epicondyle. The extensors arise from the lateral epicondyle and the flexors from the medial epicondyle. This is of particular relevance for the insertional tendinopathies (tennis and golfer’s elbow). The groove for the ulnar nerve on the medioposterior surface of the humerus accounts for the frequently encountered entrapment syndrome of the ulnar nerve. Furthermore, the bicipital aponeurosis is important, extending from the tendon of the biceps brachii medially and distally and crossing the brachial artery and median nerve. In the cubital fossa, which is demarcated laterally by the brachioradialis and medially by the pronator teres, the biceps tendon is lateral, the brachial artery next to it, and the median nerve medial. The radial artery generally is a direct continuation of the brachial artery and the ulnar artery arises from the main artery at an right angle. The lateral cephalic vein and the medial basilic vein are the superficial veins of the elbow. The median nerve perforates the pronator teres and the ulnar artery passes under the ulnar head of the pronator teres. With the elbow extended, the medial epicondyle, lateral epicondyle, and olecranon are on the same horizontal line, and with the elbow flexed, they form the corners of an equilateral triangle. The humeroulnar joint is a hinge joint, with the trochlear notch containing a smooth ridge, which glides in a groove of the humeral trochlea. The extended elbow forms a physiologic cubitus valgus with an angle of 85 degrees. The articulating surfaces of the radial head and capitellum (radiohumeral articulation) as well as the surfaces of the proximal radiohumeral joint are only partially congruent. The annular ligament of the radius encircles the radial head and arises anteriorly and posteriorly at the radial notch of the ulnar. It measures about 10 mm in width and changes its form with the rotation of the radial head. The articulating surfaces are covered by hyaline cartilage. The joint capsule is thin anteriorly and ventrally, and receives deep fibers from the brachialis anteriorly and from the anconeus posteriorly. Laterally, the joint capsule is reinforced by the collateral ligaments, which passively hold the joint together. The internal joint capsule forms synovial folds over extrasynovial fat in the olecranon, radial, and coronoid fossae. A meniscus-like fold of firm consistency projects into humeroradial articulation. Bursae occur at the olecranon, both humeral epicondyles and radial head. Additional bursae can be observed under the extensor carpi radialis brevis as well as under the anconeus. Several normal anatomical variants exist that may lead to potential pitfalls in the interpretation of the elbow examination. These are discussed at the end of the chapter. The sections of the elbow are obtained in the coronal (Figs. 4.1–4.3), sagittal (Figs. 4.4–4.6), and transverse (Figs. 4.7–4.9) planes. Since the elbow is a hinge joint, optimal positioning of the transverse and coronal sections requires full extension of the joint. In the sagittal plane, the anatomic structures are also well identified with the joint in flexion. This plane is therefore always indicated whenever full extension of the joint is impossible. The recommended sections are listed in Table 4.1. When imaging the common extensor and flexor origins for epicondylitis, a 20-degree posterior oblique coronal plane may also prove useful. Signal intensities. The different signal intensities of the various tissues are listed in Table 4.2. A SE sequence with relative T1 weighting yields the best contrast for soft tissues, articular cartilage, and bone marrow. Fat produces an intense signal and appears white on the images. Musculature has a less intense signal and is dark gray. Cortical bone, fibrous cartilage, capsule ligamentous structures, and tendons are of low signal intensity and appear as black areas. The bone marrow contains a large amount of fat, which appears white on MRI, but ‘bands’ of low signal intensity, which correspond to epiphyseal cartilage (growth plates) or its remnants, can be observed. On the T2-weighted images, fat and fluid exhibit a high signal intensity. Joint capsule. It is generally not visualized unless it is thickened or effusion is present secondary to synovitis. Normally, it is difficult to separate the capsule from the brachialis anteriorly and from the triceps tendon posteriorly. Fat pads between the synovial lining and fibrous layer of the capsule are seen posteriorly in the olecranon fossa and anteriorly in the coronoid fossa of the humerus. These fossae render the trochlea waist-like on the sagittal section. Bursae. These must be distinguished from cysts or other pathologic conditions. The superficial bursa at the olecranon is intratendinous or subtendinous underneath the subcutaneous tissue. The subtendinous bursae are best seen on transverse and sagittal sections and can be mistaken for a joint effusion if filled with fluid, but with no fluid seen anterior to the joint, a bursitis is more likely. The subcutaneous bursal involvement at the medial and lateral epicondyles must be distinguished from ligamentous lesions. Normally, these bursae are not identified unless they are altered by inflammation. If they are inflamed, they are well seen on the T2-weighted images. Arteries. These are hard to separate from the accompanying veins. Nerves. The delineation of the nerves depends on the lipomatous content of the surrounding tissues. Median nerve and radial nerve are best identified on the proximal transverse sections. The ulnar nerve is well seen on transverse sections immediately dorsal to the medial epicondyle. Radial annular ligament. This is of special importance clinically. MRI barely delineates its lesions directly, but can reveal any positional change of the radial head as an indirect sign of a ligamentous lesion (15). Figs. 4.1–4.9 Sectional anatomy of the elbow: 4. 1a, b–4. 3a, b Coronal plane 4. 4a, b–4. 6a, b Sagittal plane 4. 7a, b–4. 9a, b Transverse plane a T1-weighted SE images b Annotated schematic drawings showing the level of each section Figs. 4. 2a,b Figs. 4. 3a, b Figs. 4. 4a, b Figs. 4. 5a, b Figs. 4. 6a, b Figs. 4. 7a, b Figs. 4. 8a, b Figs. 4. 9a, b The synovial membrane reacts to cartilaginous degeneration and lesions with inflammatory changes. Hypervascular membranous protrusions grow toward the site of the articular lesion and become arranged like folds or plicae through fibrous transformations. If these changes are extensive and cover a large area, they are referred to as pannus. Pannus formation has a predilection for the olecranon and the coronoid process, but a plica can arise wherever synovial lining changes to cartilaginous coating. Plicae can become trapped at the superior recess of the joint capsule as well as between the capitellum of the humerus and radial head. The latter condition can be mistaken for a tennis elbow because of similar clinical presentation. MRI can resolve this problem. Figs. 4. 10 a–d Juvenile rheumatoid arthritis. a T2
Introduction
Examination Technique
 Patient Positioning
Patient Positioning
 Coils
Coils
 Sequences and Parameters
Sequences and Parameters
 Special Examination Techniques
Special Examination Techniques
Anatomy
 General Anatomy
General Anatomy
 Specific MRI Anatomy
Specific MRI Anatomy
Synovitis, Plicae, and Pannus Formation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree