Fig. 13.1
AP (a) and lateral (b) radiographs of an elbow in a 76-year-old woman with RA. Note the narrowing of the joint line, the articular surfaces sclerosis, and deformity, with osteophytes and osteopenia
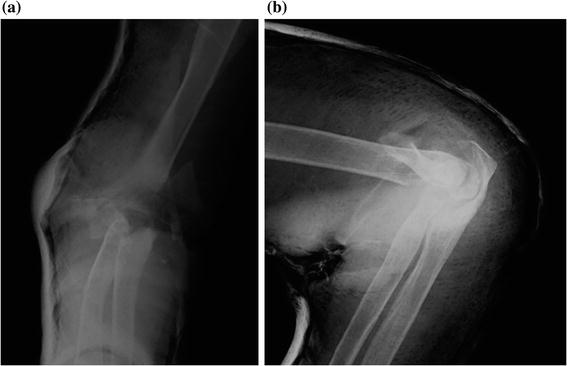
Fig. 13.2
AP (a) and lateral (b) radiographs of a 76-year-old woman with fracture-dislocation of the elbow (after reduction and cast)
Other studies are obtained case by case.
Computed tomography (CT) can be helpful in the evaluation of comminuted fractures or in mapping the extent and location of bony involvement of a tumor. If there is a suspicion of deformity or dysplasia of humerus, ulna, or radius, a 3D reconstruction can also be performed.
Magnetic resonance (MR) imaging in conjunction with physical examination is used to evaluate ligamentous integrity, especially in cases of recurrent instability.
13.2.3 Follow-up Imaging
In the AP view, the humeral component should be centered on the humeral shaft. On the lateral view, a line drawn through the anterior humeral cortex should bisect the area between the anterior flange and the posterior humeral cortex. The ulnar stem should be centered within the medullary shaft. The proximal part of the ulnar component should be even with the tip of the olecranon and should not extend beyond or proximal to the imaginary line drawn parallel to the posterior humeral shaft (Figs. 13.3, 13.4, 13.5).

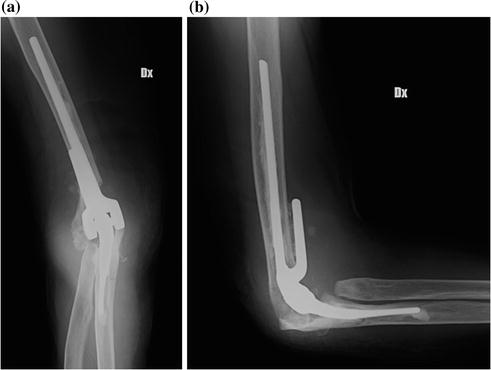


Fig. 13.3
AP (a) and lateral (b) radiographs of a semiconstrained total elbow prosthesis (Tornier Latitude) with concomitant capitellar arthroplasty, in a 76-year-old woman with RA. Note the cementation around the stems and the bone graft under the humeral flange
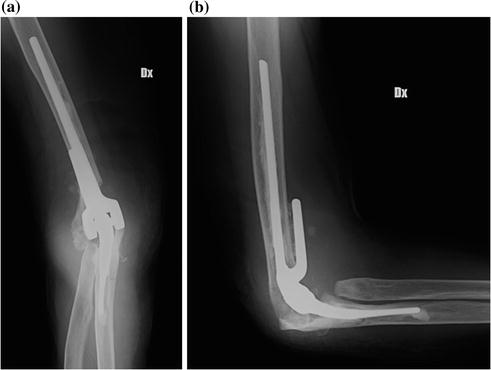
Fig. 13.4
AP (a) and lateral (b) radiographs of a semiconstrained total elbow prosthesis (Zimmer Coonrad-Morrey), in an 80-year-old woman with fracture-dislocation of the elbow. Capitellar resection has also been performed. Note the cementation around the stems and the bone graft under the anterior humeral flange

Fig. 13.5
a and b radiograms showing the aseptic mobilization of the humeral component of the prosthesis shown above (Fig. 13.4), 3 years later, with periprosthetic fracture. Note the significant osteopenia
Although radiography should be the initial imaging modality used to evaluate elbow arthroplasty, CT scan can be used to identify the degree and sites of heterotopic ossification, the severity of radiocapitellar osteoarthritis, and the presence of loose intraarticular bodies and periprosthetic fractures in select cases. MR imaging may be helpful to assess soft tissue infection, ligamentous disruption, and recurrence of neoplasm. The use of CT scan and MR imaging is limited by the presence of artifacts related to the metal composition of the prosthesis.
2.
Radial Head Arthroplasty
There are different implant designs and materials currently available in orthopedic practice for radial head arthroplasty.
Silicone hemiarthroplasty, first introduced by Swanson in 1969 [21], is rarely performed because high rates of loosening, fracture, and silicone synovitis were reported [22, 23]. Most currently used implants are composed of titanium or cobalt chromium metal (e.g., SBI-Myrmex RECON or Tornier CRF II) or, more recently, pyrocarbon (e.g., Tornier MoPyC). They can have a fixed or variable neck–head angle (unipolar or bipolar design) and can be either cemented or not (press-fit)
The unipolar, or monoblock, design consists of a radial head that does not move separately from the radial neck. The stem can either move in the radial neck and act as a spacer or may have a fixed (press-fit or cemented) design that resembles the native anatomy.
The bipolar design allows semiconstrained articulation of the radial head with the fixed metal stem and may telescope or rotate several degrees in all planes. The radial head is symmetric, composed of metal or pyrocarbon, and bridged to the radial neck by a mobile polyethylene-on-chromium bearing at the head–neck junction [24]. Physiologically, the purpose of this design is to reduce stress at the implant–bone interface and increase the contact area of the radiocapitellar joint [25] (37). However, because of this increased motion, there is greater potential for osteolysis, particle disease, and osteoarthritis at the radiocapitellar joint space.
13.2.4 Implantation Technique
The patient is supine on the operating table, and the elbow is flexed and allowed to rest on a small table. The forearm is placed and held in pronation, so that the radial nerve is medialized and the radial shaft is oriented in the axis. With the elbow flexed, an angled incision has to be centered over the tip of the epicondyle. The most popular deep approach is the lateral one, between the extensor carpi radialis brevis and the extensor digitorum communis. The other option, with the same skin incision, is to use a posterolateral approach between the anconeus, posteriorly, and the extensor carpi ulnaris, anteriorly (Kocher): This approach affords a more distal access to the radius. The annular ligament must be incised, if intact; anyway, whether it was torn or incised, it should be repaired whenever possible. Finally, the head osteotomy and the preparation of the medullary canal of the radius must be performed, with the dedicated instruments. The choice of the appropriate head size and neck length are the most critical factors in order to avoid prosthesis overstuffing and excessive ligaments stress that might cause failure of the implant. Orientation of the prosthetic neck is usually determined relative to the bistyloid plane, following the same axis. Once the trial stem has been properly seated, with cementation if necessary, the radial head can be inserted.
13.2.5 Preoperative Imaging
Preoperative assessment requires standard AP and lateral views of the head of the radius. It is important to execute also X-ray of the ipsilateral wrist, if painful, to exclude an Essex-Lopresti Syndrome.
CT scan can be helpful for a better understanding of the pattern of comminuted capitellar fractures, to decide whether to proceed with an osteosynthesis or an arthroplasty.
13.2.6 Follow-up Imaging
On both AP and lateral views, the stem of the radial head implant should be centered within the radial neck, with no tilt, and the articular surface of the radial head should be less than 1–2 mm proximal to the sigmoid notch of the ulna [26]. Transverse movement of the radial head implant, also known as translation, appears as an area of increased lucency at the tip of the stem, with the head more than 1–2 mm beyond the coronoid process on a lateral view and a narrowing of the radial–capitellar joint space.
For a correct evaluation of post-operative radiograms, it may be useful to know what kind of prosthesis has been inserted. In some implants, the stem is smooth and uncemented, and as the radial head self-centers on the capitellum during forearm rotation, it moves in the radial neck, showing a stable lucency (<2 mm) surrounding the stem on radiographs [10]. This lucency must not be confused with a sign of pathological mobilization. Otherwise, if the stem is fixed (press-fit or cemented), it should not move in the intramedullary canal; therefore, a lucency must be considered as a possible complication.
It is also important to consider if the implant is unipolar or bipolar: In the first case, the head should not move separately from the radial neck, and a variation of this angle in the different views or elbow positions may be considered pathologic. On the contrary, in the bipolar design, the head can rotate several degrees in all imaging planes (Figs. 13.6, 13.7, 13.8, 13.9).

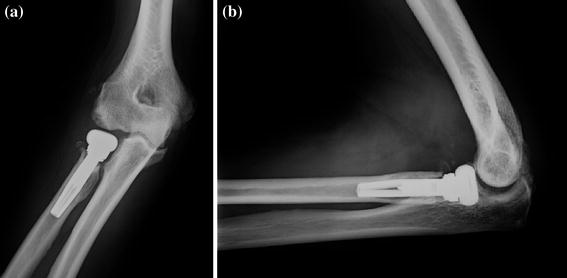
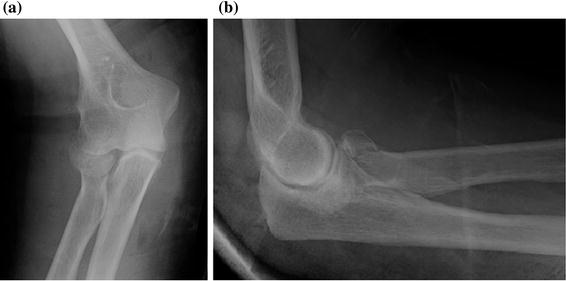
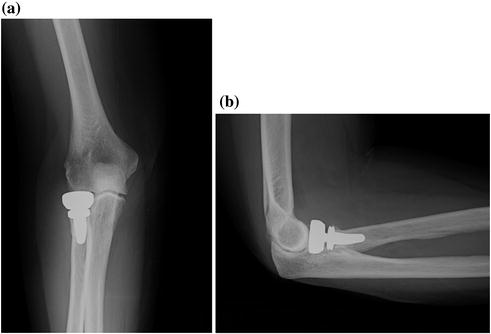

Fig. 13.6
AP (a) and lateral (b) radiographs of a 66-year-old man with fracture-dislocation of the elbow
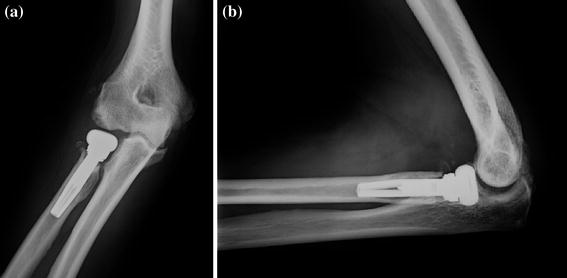
Fig. 13.7
AP (a) and lateral (b) radiographs of a 66-year-old man with a radial head arthroplasty (Tornier MoPyC, cementless, fixed pyrocarbon head)
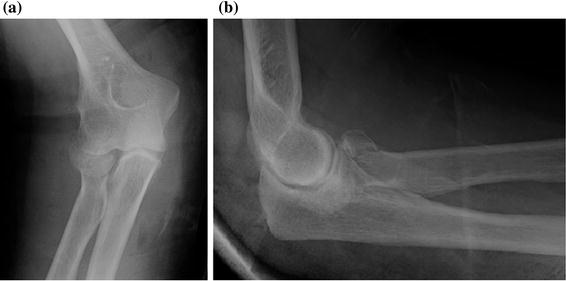
Fig. 13.8
AP (a) and lateral (b) radiographs of a 70-year-old woman with a Mason III fracture of the capitellum
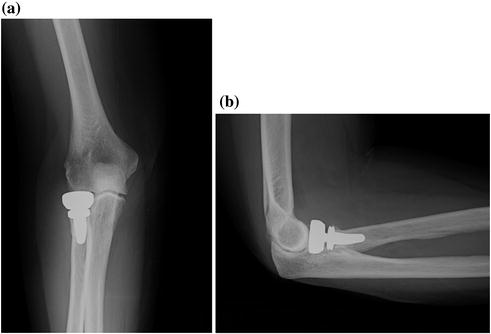
Fig. 13.9
AP (a) and lateral (b) radiographs of a 70-year-old woman with a radial head arthroplasty (SBI-Myrmex RECON, cementless, bipolar metal head). The stem of the implant is centered in the radial neck
13.3 Wrist Arthroplasty
As well as other anatomical sites, the main indications for wrist arthroplasty are pain and disfunction in patients in which medical management has failed to relieve the pain or when the deformity interferes with upper limb function.
Wrist arthroplasty is an alternative for patients with severe wrist arthritis who have specific requirements or desires to preserve motion. However, wrist replacement has its own unique risks and potential complications and is not appropriate for patients with high physical demands.
Advanced osteoarthritis of the wrist or the distal articulation of the lunate with the capitate has traditionally been treated surgically by arthrodesis. In order to maintain movement, it can be performed proximal row carpectomy with capsular interposition arthroplasty as an alternative to arthrodesis with the interposition of a pyrocarbon implant or with a total wrist arthroplasty.
Total wrist fusion is a palliative option that is often not well tolerated and that is not free of complications [27].
Total wrist arthroplasty gives superior functional results, but its use is limited because of the high rate of complications and failures [28, 29]. New models of prosthesis have been recently developed but still lack significant follow-up [30]. Its indication is pain and/or loss of function due to rheumatoid arthritis, SNAC or SLAC wrist, osteoarthritis, post-traumatic arthritis. The contraindications include poor bone quality (which may affect the implants stability), severe neurological or muscular deficiencies (that would compromise implant function), and infections (acute or chronic, local, or systemic). Other contraindications include disease which may compromise the function of the implant.
Recently, new types of wrist prosthesis have been developed. These implants often act as spacers, and they can partially or totally substitute carpal bones. They can be used alone in association with other procedures, such as first row carpectomy. The results of these types of implants are good, and with the proper indications, they represent a good alternative to total and partial wrist arthrodesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree