Neck infections are fairly common in the emergency setting, affecting a broad spectrum of the patient population. Care should be taken not only to distinguish these conditions from other noninfectious origin such as malignancy but also to guide acute clinical management. A familiarity with neck anatomy, the imaging modalities used for investigation of such conditions, as well as common findings on imaging are critical to the care of affected patients. Cross-sectional imaging is a mainstay in this setting. This article presents the most common neck infections, and details some of their most prominent findings on cross-sectional imaging.
Emergency neck infections are diverse in both their presentation and their affected patient population; with pathology ranging from a transient enlargement of a child’s cervical lymph node to a rapidly spreading necrotizing fasciitis in an adult diabetic. Despite the widespread availability of antibiotics and early surgical intervention, deep neck infections still present significant morbidity and mortality in clinical centers. Complex neck anatomy can frequently obscure or delay diagnoses, so timely and appropriate radiological interpretation are critical to patient care. This article reviews common neck infections that may be encountered in the emergency room and details some of their most salient findings on imaging.
Infections of the lymph node
The development of the lymphatic system begins in early fetal life and continues through early neonatal growth. The lymphatic system comprises a combination of lymphocytes and surrounding cellular structures that include epithelial and stromal elements. Lymph nodes are a secondary lymphoid structure where primary immune responses are initiated. Like other secondary lymphoid organs of the body, lymph nodes have specialized architecture that promotes controlled interactions of immune cells to facilitate an appropriate immune response to infectious agents. The ultimate anatomy of the head and neck lymphatic system consists of an elegant meshwork of lymphatic drainage. This network can be simplified broadly into 3 groups: the ring of Waldeyer—a circle of adenoidal, tonsillar, and lymphoid tissue; a more superficial ring consisting of the facial groups, parotids, preauricular, postauricular, and occipital nodes; and finally the nodes of the neck, which include the submaxillary, submental, and superficial and deep cervical chains.
Pathologically, an infective agent within the head and neck will spread into the surrounding tissues and be partially inactivated by the host’s immune response. A portion of the infective antigenic focus will be passively drained into the afferent lymphatic channels of the lymph node causing a cascade of events including the activation of T and B lymphocytes, the formation of multiple germinal centers with active cell proliferation, and ultimately enlargement of the lymph node. A variety of infectious and noninfectious processes may cause enlargement of the cervical lymph nodes. The stimulated node is often referred to as “reactive.” Ongoing and untreated infection may eventually result in necrosis of the node leading to suppurative adenitis.
Cervical Adenitis
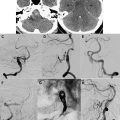
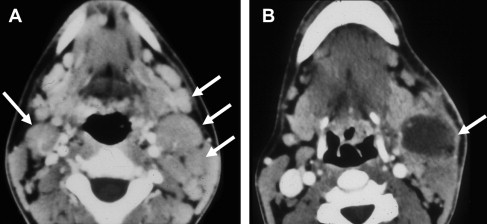
The term cervical adenitis denotes an inflammation of the lymph nodes of the neck due to an infectious process ( Fig. 1 A). Suppurative adenitis indicates an infected node that has undergone liquefaction necrosis ( Fig. 1 B). The likelihood of developing cervical adenitis, especially suppurative forms, decreases with age, although the incidence of suppurative adenitis is increasing in older patients. The pediatric population, not surprisingly, comprises a large proportion of infectious head and neck emergency room presentations.
The most common cause of cervical lymph node enlargement in children is viral infections of the upper respiratory tract. The true incidence of viral infections is unknown because the majority of such infections are benign, and do not require any form of biopsy or incision and drainage. Noteworthy virions include adenovirus, rhinovirus, enterovirus, and herpes simplex virus. Epstein-Barr virus, the causative agent in infectious mononucleosis, is characterized by generalized lymphadenopathy, weakness, fever, and malaise. Infection with cytomegalovirus and Varicella zoster is also a well-documented cause of generalized lymph node enlargement. Another noteworthy viral infection is the acquired immunodeficiency syndrome (AIDS), caused by human T-cell lymphotrophic virus type III (HTLV-III), a potentially devastating disease of childhood. Nearly 90% of human immunodeficiency virus–infected children acquire their infection vertically, during gestation or, more commonly, during labor and delivery. Patients affected by congenital transmission usually develop symptoms during the first year of life. Symptoms include localized or generalized lymphadenopathy, thrush, parotid swelling, interstitial pneumonitis, hepatosplenomegaly, and diarrhea. Affected patients also have an increased risk of bacterial superinfection including meningitis and sepsis.
Bacterial infections are the most common cause of suppurative cervical adenitis, with Staphylococcus aureus and Group A streptococcus being the most common etiologic agents. Infected patients typically present with fever and upper respiratory tract infections. Early in the course of infection, discrete nodes are palpated. With uncontrolled infection, the firm nodes are replaced by a palpable fluctuant mass (suppurative adenitis), which may require drainage. Other noteworthy bacteria that may cause suppurative cervical lymph nodes include Streptococcus pyogenes , Group B streptococcus, and Pseudomonas aeruginosa .
Computed tomography (CT) is the preferred modality to evaluate patients suspected of having cervical lymphadenitis. CT has the advantage of a shorter acquisition time relative to magnetic resonance (MR) imaging, which in children may necessitate sedation to reduce motion artifact. Early involvement by infection is characterized by homogeneous enlargement, loss of the fatty hilum, and increased enhancement of the involved lymph node on CT (see Fig. 1 A). Reticulation of the adjacent fat surrounding a suppurative lymph node or the presence of a circumferential rim of soft tissue may be helpful in differentiating an inflammatory origin as the cause of the abnormal node as opposed to metastases.
Cat-Scratch Disease
Cat-scratch disease (CSD) is a very common cause of enlarged cervical lymph nodes in the pediatric age group, and has been reported to be the most common cause of chronic unilateral regional lymphadenitis in children in the United States. The disorder is caused by the bacteria Bartonella henselae and usually presents within 3 to 10 days following contact. A prior history of a cat scratch, lick, bite, or other exposure is present in more than 90% of cases. These patients present clinically with tender, enlarged cervical lymph nodes, fever, and malaise. Approximately 10% of patients develop overlying erythema and fluctuant lymph nodes that require drainage. Diagnosis is confirmed by a positive cat-scratch antigen or demonstration of the bacillus on a Warthin-Starry stain of infected material.
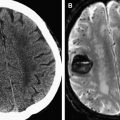
The typical findings on CT are a unilateral clumped group of enlarged lymph nodes clustered in the primary echelon drainage of the site of contact. Central areas of decreased attenuation within the lymph nodes are rare ( Fig. 2 ). There may be some subtle reticulation of the fat surrounding the lymph nodes; however, gross findings of extracapsular extension is rare. On MR imaging, the signal characteristics are nonspecific and can be seen in a variety of disorders. The nodes typically enhance with contrast and contain high T2 signal.