Fig. 13.1
(a) Axial view of proximal right coronary artery (thin arrows) and left coronary artery (thick arrows) acquired on 1.5 T system using the whole heart, navigator technique. AO Aorta, RV right ventricle, RA right atrium. (b) Coronal view of proximal right and left coronary arteries acquired on 1.5 T system using the whole heart, navigator technique
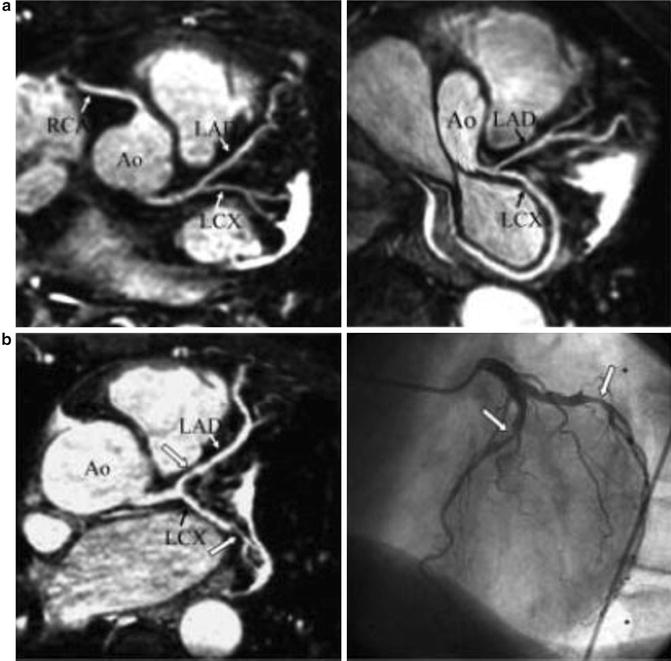
Fig. 13.2
(a) Multiplanar reformatted MRCA images of right and left coronary arteries with excellent visualisation of left anterior descending artery (LAD) and left circumflex artery (LCx) with their side branches. Ao Aorta, RCA right coronary artery (b) MRCA of patient with two-vessel disease (left) in comparison with X-ray coronary angiography (right). Arrows point to region of stenosis (Reprinted from Jahnke C, Paetsch I, Nehrke K, et al. Rapid and complete coronary arterial tree visualization with magnetic resonance imaging: feasibility and diagnostic performance. European Heart Journal 2005; 26:2313–2319. With permission from Oxford University Press)
The first multicentre prospective study comparing MRCA with XCA was conducted by Kim and colleagues in 1999 [28]. They enrolled 109 patients suspected to have CAD and performed MRCA and XCA. The authors used three-dimensional gradient echo sequences during free breathing for 10–15 min and applied the T2-weighted preparation pulse including the frequency selective fat saturation pre pulse. This study demonstrated high sensitivity and specificity for left main coronary disease and three-vessel coronary disease with 87 % accuracy. The specificity for any CAD was low at 42 %. The main limitation of this study was the limited coverage of the coronary system, and the prolonged nature of the examination with a mean scan time of 70 min. Yang and colleagues have reduced the acquisition time to 10 min in their study of 62 patients suspected with CAD. They performed contrast-enhanced whole heart MRCA on the 3 T system in 62 consecutive patients and compared with XCA. The sensitivity, specificity, and accuracy of MRCA for detecting significant stenosis were 94 %, 82 %, and 89 %, respectively [29]. More recently Yoon and colleagues demonstrated the utility of whole heart MRCA in predicting future risk of cardiac events in patients suspected to have CAD. In their study of 207 patients suspected to have CAD with non-contrast-enhanced free breathing whole heart MRCA on the 1.5 T system, the annual cardiac event rate was 0.3 % in the group without significant stenosis and 6.3 % in the patients with >50 % stenosis on MRCA [30].
The whole heart MRCA approach has increased coverage and greatly reduced imaging time although has not greatly improved diagnostic accuracy. The incorporation of SSFP technique into the whole heart coronary magnetic resonance angiography (MRA) facilitated the visualisation of the middle and distal segments of the coronary arteries [31]. SSFP techniques achieve higher signal- and contrast to noise ratio of the coronary artery lumen against the surrounding myocardium. This sequence is used in most centres currently.
MRCA in Subclinical Coronary Atherosclerosis
Even before reduction in the coronary artery luminal diameter, the artery remodels by increasing wall thickness with preservation of luminal diameter (Glagov remodelling) [3]. This positive remodelling of the vessel wall has been demonstrated on intravascular ultrasound and multi-detector computed tomography. Both these modalities have their limitations especially when serial assessment is required. Black blood imaging and improvement in spatial resolution techniques have made it possible to image the coronary artery wall using MR [32]. Fayad et al. were the first to demonstrate the feasibility of black blood fat suppressed magnetic resonance imaging in measuring the coronary wall thickness and visualise the remodelling of the coronary artery wall [12]. Desai and colleagues confirmed reproducibility of this technique and showed that this can be implemented in longitudinal studies of progression and regression of coronary atherosclerosis [33].
The MESA (Multi-Ethnic Study of Atherosclerosis) study assessed the coronary arterial remodelling as a marker of subclinical atherosclerosis using coronary wall MR in asymptomatic population-based cohort [34]. MRCA was performed on 179 subjects using the 3D whole heart navigator, ECG gated, and fat suppressed T2 preparation SSFP sequence in 1.5 T system. They detected positive remodelling in this asymptomatic cohort of men and women. Larger studies are required to assess the therapeutic implications of early detection of coronary atherosclerosis.
MRCA in Plaque Characterisation
Plaque characterisation has been demonstrated using delayed enhancement (DE) CMR imaging using contrast agents (Fig. 13.3). The demonstration of contrast enhancement in coronary atherosclerotic plaques correlated well with increase in severity of plaque calcification as confirmed on multi-slice computed tomography (MSCT) and luminal stenosis seen on coronary angiography, in patients with chronic stable angina [35]. Significant uptake of contrast has been demonstrated in the coronary plaques 6 days post-acute coronary syndrome, which have decreased on 3-month follow-up scans indicating inflammation in the plaque [36].
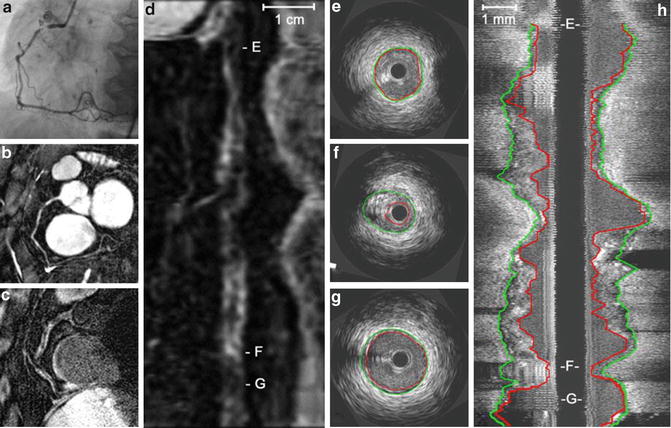
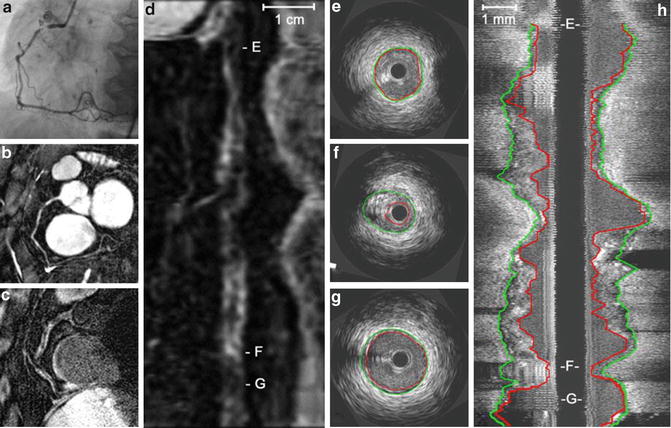
Fig. 13.3
A 61-year-old female patient with stable angina. X-ray angiography (a) and coronary MRA (b) demonstrate high-grade stenosis in the proximal RCA. (c) Corresponding MR vessel wall image demonstrate several areas with vessel wall thickening and high signal intensity. (e) (Distal RCA), (f) (diseased area) and (g) (proximal RCA) are cross-sectional IVUS images and refer to the corresponding areas as shown on stretched multiplanar reformation (MPR) of the vessel wall (d: e, f, g) and the longitudinal IVUS reformat (h: e, f, g). f is the area of maximum stenosis (Reprinted from Gerretsen S. Detection of coronary plaques using MR coronary vessel wall imaging: validation of findings with intravascular ultrasound. European Radiology (2013) 23:115–124. With permission from Springer Science + Business Media)
MRCA in Coronary Revascularisation
The use of intracoronary stents has increased significantly in the last decade. The clinical safety of the stents is well established in the 1.5 T even early after implantation [37–41]. The stents are non-ferromagnetic and are not susceptible to attractive forces or local heating. Though majority of the stents are approved for CMR assessment immediately after implantation their propensity to cause local signal void and susceptibility artefacts results in suboptimal assessment of in-stent disease.
In contrast, coronary artery bypass grafts (CABG) are large calibre vessels with a predictable course and less influenced by cardiac motion. Therefore they would be ideal to image on MRCA. Langerak and colleagues studied 69 patients awaiting elective coronary angiography for assessment of chest pain post-CABG [42]. They underwent MRCA at baseline and stress flow mapping was performed. When compared to conventional angiography they reported a sensitivity and specificity of 96 and 92 %, respectively, for stenosis in the grafts of ≥70 %. The limitation in imaging the coronary bypass grafts is the susceptibility artefact and signal void created by the metallic clips at anastomotic sites.
Indications for MRCA
Despite advances in imaging techniques and higher field strength scanners, there is a paucity of large multicentre clinical trials in MRCA. Recently, Kato et al. in their 7 centres, Japanese MRCA trial imaged 138 patients with 3D navigator corrected SSFP whole heart MRCA sequence [43]. The average image time was under 10 min. Their results were modest with sensitivity of 88 %, specificity of 72 %, positive predictive value (PPV) of 71 %, and negative predictive value (NPV) of 88 %. Similar to earlier studies, they were able to exclude left main coronary disease and three-vessel coronary disease with NPV of 99 %. When compared to recent multicentre CCTA studies, the NPV in the low pre-test probability of CAD group (<20 %) was similar and therefore may be a safe alternative to CCTA in this group of patients [44, 45]. In the relatively high pre-test probability group, MRCA was able to exclude significant disease in left main coronary artery and three-vessel coronary disease.
In a recent meta-analysis comparing CCTA and MRCA for ruling out clinically significant CAD in adults with suspected or known CAD, 89 and 20 studies, respectively, were eligible for analysis. There were 7,516 patients in the CCTA studies and 989 in the MRCA studies. Bivariate analysis of the data yielded a mean sensitivity and specificity of 97.2 and 87.4 for CCTA and 87.1 and 70.3 % for MRCA [46]. In patients who were suspected to have CAD, CCTA is more accurate in detecting and ruling out clinically relevant CAD (Table 13.1).
Table 13.1
Comparison between MRCA and CCTA in the assessment of coronary arteries
MRCA | CCTA |
|---|---|
Advantages | |
• No exposure to ionising radiation | • Higher accuracy in excluding CAD |
• Multi-parametric, functional assessment possible | • More widely available |
• No need for oral or intravenous beta blocker | • Easier to perform |
• No artefacts with severely calcified plaques | • Shorter scanning times |
• Relatively comfortable for patients | |
Disadvantages | |
• Longer scanning time | • Exposure to radiation |
• Restricted availability | • Need for iodinated contrast |
• Contraindicated in patients with pacemaker/intracardiac defibrillators/metallic implants | |
Not ideal for claustrophobic patients | |
Conclusion
Cardiac MR imaging has evolved significantly in the last two decades and has an established role in the assessment of cardiac anatomy, function, myocardial perfusion, and tissue characterisation. The addition of MRCA to CMR would add to its versatility and provide a safe, non-invasive comprehensive cardiac assessment tool. MRCA is still evolving in the assessment of coronary atherosclerosis and its full potential has not been realised yet. Large multicentre comparative studies and outcome studies in the subclinical detection of coronary atherosclerosis are needed to recommend routine use of this safe, non-invasive imaging modality.
References
1.
Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–98.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree