Hemangiomas are vascular tumors that enlarge through proliferation of endothelial cells. They are the most common tumors of infancy, appearing in as many as 10% to 12% of children under 1 year of age, with double this incidence in preterm infants weighing less than 1000 g. Female-to-male predominance is about 4:1. Most hemangiomas appear in the first 6 weeks of life. Hemangiomas can be seen in the skin in 4% to 10% of Caucasian newborns, and less frequently in non-Caucasians. The head and neck regions are involved most frequently, followed by the trunk and the extremities. Despite their benign nature, hemangiomas can cause significant morbidity if not recognized and treated properly. Endovascular treatment is an important component of the interdisciplinary management of hemangiomas.
Hemangiomas are vascular tumors that enlarge through proliferation of endothelial cells. They are the most common tumors of infancy, appearing in as many as 10% to 12% of children under 1 year of age, with double this incidence in preterm infants weighing less than 1000 g . In the children of mothers who have undergone chorionic-villus sampling, the incidence of hemangiomas has been reported to be 10 times higher . Female-to-male predominance is about 4:1.
Most hemangiomas appear in the first 6 weeks of life. Hemangiomas can be seen in the skin in 4% to 10% of Caucasian newborns, and less frequently in non-Caucasians . The head and neck regions are involved most frequently (60% of cases), followed by the trunk (25% of cases) and the extremities (15% of cases). Hemangiomas occur as an isolated lesion in 80% of cases, whereas they are multifocal in 20%. Involvement of the liver, gastrointestinal tract, or lungs is common in patients who have multiple cutaneous lesions. Central nervous system involvement is rare, usually associated with the disseminated form, and often lethal.
Despite their benign nature, hemangiomas can cause significant morbidity if not recognized and treated properly. The management of hemangiomas has emerged as interdisciplinary, with endovascular treatment an important component.
Clinical presentation and natural history
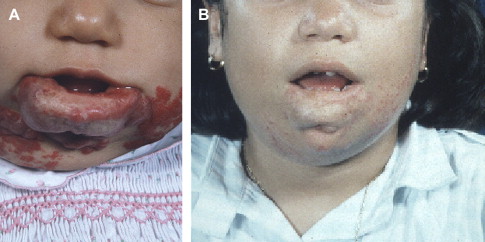
At birth, hemangiomas appear as small, pale, or erythematous macules, red spots, ecchymotic-like patches, or telangiectasias. After birth, the lesion is noted to grow and, if superficial, appears more as a bright red, slightly raised, noncompressible plaque lesion ( Fig. 1 ). Less superficial lesions involving the deep dermis or subcutaneous tissue may have minimal, blush-like discoloration, or no skin involvement at all ( Fig. 2 ). Deeper hemangiomas present several months later and are noted only when they produce contour asymmetry. Hemangiomas are characterized by a rapid growth, or proliferative, phase, which may last up to 18 months, at which point growth reaches a plateau. Nearly all hemangiomas go through a spontaneous involuting phase. Areas of ulceration or necrosis, with patchy healing, are not infrequent. By 5 years of age, 50% of hemangiomas will have achieved complete involution, and 70% by 7 years of age, with the remaining children showing continued improvement until ages 10 to 12 ( Fig. 3 ) . In approximately one half of children, the skin at that time will appear normal.


Diagnosis
Superficial hemangiomas are easy to diagnose on physical examination because of their characteristic red, raised, strawberry-like appearance. The lesions are soft on palpation and warm to touch, and may be pulsatile, with an audible bruit during the proliferative phase. Deeper lesions with intact overlying skin may be more difficult to diagnose. The skin color may appear blue because of the presence of dilated draining veins beneath the skin. Other characteristic physical features include a pale halo around the lesion, and superficial telangiectasias. The history of rapid postnatal growth followed by stabilization and involution is helpful in making the diagnosis. Usually, the first sign of the involuting phase is marked by a change from the bright reddish, purplish, or crimson color of the cutaneous component to a grayish, patchy, less intense vascular soft tissue, with decreased or absent pulsations. Involuting lesions have a soft, fatty consistency.
Hemangiomas without skin involvement can be differentiated clinically from malformations because of their rapid proliferation, which is faster than the normal growth of the patient. In infants with large lesions, swelling can be seen, particularly if the hemangioma has large draining veins. An increase in size during crying episodes is more characteristic of a venous malformation. However, in some scalp locations associated with a bone defect or located over a bony suture, pulsatility and a transient increase in size during crying episodes may be noted as well .
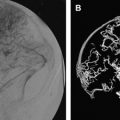
Although most hemangiomas can be diagnosed clinically, deep lesions require imaging to rule out soft-tissue malignancies and vascular malformations. The hallmark of hemangiomas on imaging is the combination of a homogeneous, solid, parenchymal mass with evidence of increased vascularity, and less frequent high-flow vascular supply and drainage. Ultrasound scanning with Doppler imaging demonstrates the solid parenchymal component with dilated vessels inside and around the lesion. Doppler assessment of the vessels indicates high flow with decreased arterial resistance and increased venous velocity, consistent with microshunting. With involution, the vessels become smaller, and the Doppler flow more normal. CT shows hemangiomas to be similar, or lower in density than surrounding muscle, with uniformly dense contrast enhancement and demonstration of feeding and draining vessels around and below the lesion. During and after involution, subcutaneous lesions appear to have increasing amounts of intralesional fat and smaller vessels, with no associated bone hypertrophy. MR imaging demonstrates a lobulated, parenchymal mass with dilated feeding arteries and draining veins within and around the lesion ( Fig. 4 ). Hemangiomas are iso- or hypointense on T1-weighted sequences, and moderately hyperintense on T2-weighted sequences. They enhance uniformly in the proliferating phase. Gradient sequences confirm the high-flow vessels within and around the solid mass. Analysis of associated deep and intracranial lesions, if suspected, makes MR imaging particularly helpful under these circumstances. MR angiography is of no particular value at present.
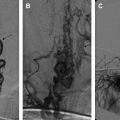
Angiography is not needed for diagnosis. When performed at the time of planned endovascular embolization, it demonstrates dilated feeding arteries, organized gland-like arterial angioarchitecture with a dense parenchymal blush, and drainage into dilated adjacent veins ( Fig. 5 ). Venous filling may be very rapid, indicating arteriovenous shunting. It is sometimes difficult to distinguish hemangiomas from hypervascular soft-tissue tumors, which tend to have less well defined margins and irregular vessels, with signs of encasement and neovascularity.
Diagnosis
Superficial hemangiomas are easy to diagnose on physical examination because of their characteristic red, raised, strawberry-like appearance. The lesions are soft on palpation and warm to touch, and may be pulsatile, with an audible bruit during the proliferative phase. Deeper lesions with intact overlying skin may be more difficult to diagnose. The skin color may appear blue because of the presence of dilated draining veins beneath the skin. Other characteristic physical features include a pale halo around the lesion, and superficial telangiectasias. The history of rapid postnatal growth followed by stabilization and involution is helpful in making the diagnosis. Usually, the first sign of the involuting phase is marked by a change from the bright reddish, purplish, or crimson color of the cutaneous component to a grayish, patchy, less intense vascular soft tissue, with decreased or absent pulsations. Involuting lesions have a soft, fatty consistency.
Hemangiomas without skin involvement can be differentiated clinically from malformations because of their rapid proliferation, which is faster than the normal growth of the patient. In infants with large lesions, swelling can be seen, particularly if the hemangioma has large draining veins. An increase in size during crying episodes is more characteristic of a venous malformation. However, in some scalp locations associated with a bone defect or located over a bony suture, pulsatility and a transient increase in size during crying episodes may be noted as well .
Although most hemangiomas can be diagnosed clinically, deep lesions require imaging to rule out soft-tissue malignancies and vascular malformations. The hallmark of hemangiomas on imaging is the combination of a homogeneous, solid, parenchymal mass with evidence of increased vascularity, and less frequent high-flow vascular supply and drainage. Ultrasound scanning with Doppler imaging demonstrates the solid parenchymal component with dilated vessels inside and around the lesion. Doppler assessment of the vessels indicates high flow with decreased arterial resistance and increased venous velocity, consistent with microshunting. With involution, the vessels become smaller, and the Doppler flow more normal. CT shows hemangiomas to be similar, or lower in density than surrounding muscle, with uniformly dense contrast enhancement and demonstration of feeding and draining vessels around and below the lesion. During and after involution, subcutaneous lesions appear to have increasing amounts of intralesional fat and smaller vessels, with no associated bone hypertrophy. MR imaging demonstrates a lobulated, parenchymal mass with dilated feeding arteries and draining veins within and around the lesion ( Fig. 4 ). Hemangiomas are iso- or hypointense on T1-weighted sequences, and moderately hyperintense on T2-weighted sequences. They enhance uniformly in the proliferating phase. Gradient sequences confirm the high-flow vessels within and around the solid mass. Analysis of associated deep and intracranial lesions, if suspected, makes MR imaging particularly helpful under these circumstances. MR angiography is of no particular value at present.
Angiography is not needed for diagnosis. When performed at the time of planned endovascular embolization, it demonstrates dilated feeding arteries, organized gland-like arterial angioarchitecture with a dense parenchymal blush, and drainage into dilated adjacent veins ( Fig. 5 ). Venous filling may be very rapid, indicating arteriovenous shunting. It is sometimes difficult to distinguish hemangiomas from hypervascular soft-tissue tumors, which tend to have less well defined margins and irregular vessels, with signs of encasement and neovascularity.