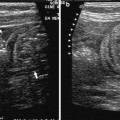
Fig. 1
Neutropenic entercolitis. a Asymmetric hypoechoic non-homogenous tumour-like bowel wall thickening in the ileocecal region are the characteristic sonographic findings in NPC. The stenosis (Stenose) and dilatation of the small bowel (DD) is also indicated. b Asymmetric and non-homogenous wall thickening in the ileocecal region with transmural inflammatory reaction in a patient with NPC. CDI is helpful for characterization. c Asymmetric and inhomogenous and in this case hyperechoic wall thickening of the ileo-cecal valve in a patient with NPC. CDI is helpful for characterization
Intramural air suggests an infection with anaerobic bacteria. Pericolic fluid is a sign of a (possible) perforation. Sonography may demonstrate free abdominal air, which is usually detected on the right side, e.g., perihepatic. In advanced disease with catastrophic prognosis, air bubbles in the portal vein may be demonstrated, resembling late phases after application of contrast enhancing agents. Another feature may be pneumatosis cystoides intestinalis, as seen in premature infants with necrotizing enterocolitis. It is noteworthy that the hydrogen content of the expired air in these patients is massively increased (Dietrich et al. 2006).
A few prospective studies used ultrasound to evaluate patients after chemotherapy. Bowel wall thickness (>4 mm) was seen only in those patients who fulfilled symptom criteria for NPC, and not in those patients with mucositis alone or in those who remained asymptomatic (Gorschluter et al. 2002). Besides the wall thickness, its overall echotexture and appearance of surrounding structures should be considered (Nuernberg et al. 2008; Dietrich et al. 1998b).
Bowel wall thickness has also been shown to be an important prognostic factor. Cartoni et al. (2001) evaluated neutropenic patients with fever and abdominal pain. A bowel wall thickness of >5 mm was considered as diagnostic of NPC. The mean duration of symptoms was significantly longer among patients with (7.9 days) than among patients without (3.8 days) bowel wall thickening and the related mortality was also higher (29.5 versus. 0 %). The degree of bowel wall thickness correlated with the outcome of patients: 60 % of patients with bowel wall thickness >10 mm died from this complication, compared with only 4.2 % of those with mural thickness ≤10 mm (Cartoni et al. 2001). These results are similar to those of our (not yet published) prospective study. Recently, 14 neutropenic patients (absolute neutrophil count <500/mm3) with sonographic features of NPC were evaluated regarding clinical findings, sonographic features, and outcome (8 male, mean age 48 years). Bowel wall thickness was measured at terminal ileum, cecum, sigmoid colon, and small intestine by high resolution sonography with moderate pressure. A thickness <2 mm was considered normal, a thickness >2 and <5 mm was considered as non-specific bowel wall thickening, and a thickness >5 mm was considered abnormal confirming the diagnosis of NPC (Dietrich et al. 2006). The morphology and the five layers of ileum and colon were evaluated assessing a mucosal or transmural pattern of inflammation. Bowel wall vascularity was examined by color Doppler imaging (CDI) and graded as ischemic (no flow pattern), normal, or hypervascular as per standard GvHD criteria (Klein et al. 2001).
In all 14 patients treatment consisted of bowel rest and total parenteral nutrition and multiple antibiotics. G-CSF was given in eight patients to shorten the time of neutropenia. Three patients died due to sepsis with multiorgan failure. High C-reactive protein (P < 0.001) and the sonographically demonstrated bowel wall thickness (P < 0.03) were associated with lethal outcome. The surviving 11 patients recovered from NPC and the reduction of abdominal symptoms was accompanied by progressive reduction of intestinal mural thickening in follow-up ultrasound examinations. Nearly, all patients with NPC (13 of 14) presented a transmural inflammatory pattern of thickened bowel wall. In all patients, the ileocecal region was involved. The thickness of the inflamed bowel wall was at least 10 mm. Hypervascularity on CDI and the detection of small amounts of free fluid in the abdomen were documented in the majority of patients with NPC. Typical sonographic characteristics in NPC are depicted in Fig. 1a.
Other imaging methods include computed tomography (CT) and abdominal X-ray whereas barium enema and enteroclysis are relatively contraindicated as they increase the luminal pressure and the risk of perforation. Although most authors favor CT as the most sensitive diagnostic tool for NPC, sonography has the advantage of being easily performed with repeated examinations (e.g., at the bedside) even in severely ill patients in intensive care or transplantation units. The findings on abdominal X-ray are often nonspecific and may show small bowel ileus, an ill-defined soft tissue density in the region of the cecum, thickened air-filled loops of bowel or signs of pneumatosis intestinalis. Other methods such as scintigraphy are not routinely used in clinical practice.
Several conditions should be taken into account in the differential diagnosis. Appendicitis is very often the main diagnosis. Because of the high perioperative mortality in these patients [most often from 50 to 100 % (Wade et al. 1992)] the operative approach should be avoided. Other acute or chronic inflammatory diseases of the ileocecal area are viral (e.g., CMV colitis) and bacterial ileocecitis, Crohn′s disease, pseudomembranous and ischemic colitis, and colonic pseudo-obstruction (Nuernberg et al. 2008). In post allogeneic stem-cell transplantation patients, one has to think of graft versus host disease (GvHD), although this usually occurs after engraftment (Klein et al. 2001). A neoplastic (leukemic of lymphocytic) infiltration of the ileocecal region must be excluded especially in case of a palpable mass in this area. In pancytopenic patients one also has to think of an acute hemorrhage into the mucosal wall (Dietrich et al. 2006).
Penicillin-induced segmental hemorrhagic colitis shows characteristic sonographic features with asymmetric wall thickening of the colon (typically in the right colon) with loss of intestinal wall layers due to edema and bleeding. Relative hypovascularization can be detected with CDI. The surrounding colon may appear normal. The past medical history is decisive. Intestinal tuberculosis has become increasingly observed since the occurrence of the AIDS pandemic. As with NPC, many regions of the intestine may be involved, although the ileocecal region is affected in up to 90 % of patients. The ultrasound image displays a hyperechoic (sometimes asymmetrically thickened) mucosa with loss of folds and unclear demarcation from (sometimes asymmetrically) thickened submucosa, so that a pseudo-polypoid image prevails. Short stenoses, mesenteric hyperechoic inflammatory signs, development of fistula, and abscesses can also be seen. Other characteristic signs include severe mesenteric lymphadenopathy (sometimes more than 10 hyperechoic round- to oval-shaped lymph nodes are detected) and a distended ileocecal valve, with asymmetrical (sometimes tumorous) thickening, especially affecting the medial cecal wall. Patients with peritoneal tuberculosis may also have ascites and thickening of the peritoneum (Barreiros et al. 2008).
1.5 Management and Prognosis
The conservative approach, total parenteral nutrition, nasogastric suction, broad spectrum antibiotics, and antifungal treatment should be placed at the forefront. As neutropenia represents the “sine qua non” of NPC, time of neutropenia should be shortened, e.g., with granulocyte colony-stimulating factors or granulocyte transfusions (Dietrich et al. 2006; Wade et al. 1992). Antibiotic coverage for C. difficile infection should be added (Davila 2007), but no prospective randomized trials or high-quality retrospective studies on the treatment of NPC have been published so far. As the perioperative mortality in these patients is very high, early surgical intervention is not recommended. On the other hand, the right time for surgery should not be missed. Therefore, a close clinical evaluation of the patient by physicians and surgeons is mandatory. The indications for surgery are the same as in persistent gastrointestinal bleeding, free perforation, and clinical deterioration suggesting uncontrolled sepsis (Wade et al. 1992).
The mortality rate in patients with signs of perforation, sepsis, and multi-organ failure is higher than 50 % (Abbasoglu and Cakmakci 1993). The main prognostic factor is neutrophil recovery and overall time of neutropenia, as neutropenia allows for continuous bacterial invasion of the bowel wall, perpetuating the lesion, with possible necrosis and perforation (Wade et al. 1992).
The sonographically demonstrated thickened bowel wall is associated with poor prognosis and is also a useful tool for monitoring disease progression by showing the decreasing bowel wall thickening in responding patients. In addition, sonography might indicate complications of the disease by detecting free abdominal air or intramural hemorrhage.
2 Acute Graft versus Host Disease
2.1 Introduction
Graft versus host disease (GvHD) is a major complication after allogeneic stem cell transplantation (HCT). It has been classically divided into acute and chronic disease based upon the time of onset. As per definition, classic acute GvHD (aGvHD) occurs within the first 100 days after hematopoietic cell transplantation (HCT). Chronic GvHD (cGvHD) has a later onset. However, new criteria were developed in 2005 (Filipovich et al. 2005; Table 1).
Table 1
Categories of acute and cGvHD according to NIH consensus
Category | Time point of onset of symptoms after HCT or donor lymphocyte infusion (DLI) | Signs of aGvHD | Signs of cGvHD |
|---|---|---|---|
Acute GvHD | |||
Classic aGvHD | ≤ day 100 | Yes | No |
Persisting, relapsed or late onset aGvHD | > day 100 | Yes | No |
Chronic GvHD | |||
Classic cGvHD | No time limit | No | Yes |
Overlap syndrome | No time limit | Yes | Yes |
2.2 Epidemiology and Pathogenesis
Graft versus host disease is a donor T cell-mediated reaction against tissue of the recipient. It occurs predominantly in skin, liver, and gastrointestinal (GI) tract. Frequency and severity of aGvHD are mainly dependent on the grade of HLA match between donor and recipient, the intensity of conditioning, donor type (sibling vs. unrelated), and the stem cell source (bone marrow vs. peripheral blood). After HCT 10–80 % of patients develop aGvHD and 30–75 % of patients suffer from clinically relevant grade II-IV aGvHD of the GI tract (Mielcarek et al. 2003).
The pathogenesis of acute intestinal GvHD has been described by Ferrara et al. (1999) in a three-phase model. The first phase involves damage of host tissues by inflammation from the conditioning prior to transplantation. As a second phase, recipient and donor antigen-presenting cells as well as proinflammatory cytokines led to an activation of donor T cells. In the third phase, called the effector phase, activated donor T-cells confer cytotoxicity against target host cells through Fas–Fas ligand interactions, perforin-granzyme B, and the additional production of cytokines, such as TNF-α (Jacobsohn and Vogelsang 2007).
2.3 Symptoms
The main target organs of aGvHD are skin, liver, and GI tract. A maculopapular rash is the most common and earliest manifestation of aGvHD. The rash is often confluent and can occur simultaneously with hematologic engraftment. Typical areas for skin aGvHD are palm and sole. Hyperbilirubinemia or elevated liver enzymes can be signs of aGvHD with liver involvement (McDonald 2006). Involvement of the GI tract with aGvHD is often severe and difficult to treat. It is characterized by diarrhea, abdominal cramping, nausea, or vomiting. The severity of GI involvement is determined by the volume of diarrhoea, which can occasionally exceed 10 l per day. Diarrhea may be watery or bloody. Additionally, severe ileus may develop (Cox and McDonald 1990). The severity of aGvHD is determined by assessing the degree of skin, liver, and GI tract involvement. This is subsequently combined with the results on performance scales to produce an overall grade (Przepiorka et al. 1995; Table 2).
Clinical staging of aGvHD according to Organ Involvement | |||||
|---|---|---|---|---|---|
Organ stage | Skin | Liver | GI-tract | ||
1 | Maculopapular rash < 25 % of body surface | Serum bilirubin 2–3 mg/dl | Diarrhoea 500–1000 ml/day or nausea | ||
2 | Maculopapular rash 25–50 % of body surface | Serum bilirubin 3–6 mg/dl | Diarrhoea 1000–1500 ml/day | ||
3 | Maculopapular rash > 50 % of body surface | Serum bilirubin 6–15 mg/dl | Diarrhoea 1500–2000 ml/day | ||
4 | Generalized erythroderma with bullous formation and desquamation | Serum bilirubin > 15 mg/dl | Diarrhoea > 2000 ml/day Severe abdominal pain with or without ileus | ||
Overall grading of aGvHD | |||||
Stage per organ | ECOG | ||||
Overall grade | Skin | Liver | GI-Tract | Performance | |
I | 1–2 | 0 | 0 | 0 | |
II | 1–3 or | 1 or | 1 or | 1 | |
III | – | 2–3 or | 2–3 or | 2–3 | |
IV | 4 or | 4 or | 4 or | 3–4 | |
2.4 Diagnosis
The diagnosis of aGvHD can be made clinically in the patient presenting with a classic rash, abdominal cramps with diarrhoea, and a rising serum bilirubin concentration, within the first 100 days following transplantation. After allogeneic HCT the key symptoms of intestinal aGvHD such as diarrhea, nausea, or vomiting are frequent and nonspecific. Differential diagnoses include side effects of pre-transplant conditioning, neutropenic colitis, C. difficile colitis, side effects of immunosuppressants (e.g., MTX or mycofenolate mofetil), or antibiotics and viral infections (Norovirus, Rotavirus, Adenovirus, Herpes Simplex Virus, Varicella Zoster Virus and Cytomegalovirus).
A clinical impression of intestinal aGvHD has to be corroborated by endoscopy (esophago-gastroduodenoscopy and ileocoloscopy) with biopsies. Endoscopic features of aGvHD described as ‘Freiburg Criteria’ are spotted erythema, aphthous lesions, confluent defects, ulcerations, and complete denudation of the mucosa (Kreisel et al. 2012). For the diagnosis of intestinal aGvHD histologic confirmation is mandatory and since viral infections often occur simultaneously with aGvHD, biopsies have to be investigated by immune staining and by virological methods, respectively.
2.5 High Resolution Sonography
The first article on sonographic findings in intestinal aGvHD was published in 2000 (Haber et al. 2000) and identified the key finding of bowel wall thickening, particularly in the ileocoecal region.
Thereafter, high resolution ultrasound and CDI were demonstrated to be helpful for diagnosis and differential diagnosis of aGvHD identifying several songraphic features of gastrointestinal aGvHD, which are summarized in Table 3 (Gorg et al. 2005; Klein et al. 2001; Dietrich 2010




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree