Fig. 13.1
(a, b) Normal abductor tendons. Intermediate-weighted fast spin-echo images coronal plane in a 25-year-old male (TR/TE 2,590 ms/15 ms, FOV180 × 143 mm, NEX 1; matrix 512 × 256, ETL factor 7, section thickness 3 mm). MR images show a normal insertion of gluteus minimus tendon in (a) (white arrowheads) at the anterior facet of the greater trochanter and a normal insertion of gluteus medius tendon at the lateral facet (b) (white arrowheads). Both tendons show a homogeneous hypointense signal (Gmin gluteus minimus muscle, Gmed gluteus medius muscle)

Fig. 13.2
STIR sequence (turbo-inversion-recovery-magnitude) (TR/TE/TI, 4,890 ms/45 ms/150 ms, FOV 180 × 180 mm, NEX 1, matrix 256 × 179, ETL 9, section thickness 7 mm) of a 48-year-old female patient shows a partial tear of the gluteus minimus tendon attachment with increased signal within the tendon (white arrows) and severe peritendinous fluid adjacent to the partial tear
Gordon et al. [9] suggested that tears of the gluteal tendons are likely to be responsible for calcifications seen radiographically in some patients. In patients with tears of the gluteus medius and/or minimus tendons reactive sclerosis and bone proliferation can be observed particularly at the anterior edge of the sclerotic area [10]. In a study of Steinert et al. [11] including 150 patients, 90 % of patients with trochanteric surface irregularities larger than 2 mm on conventional radiographs have a lesion of the abductor tendons on MR images (positive likelihood ratio of 5.8). 98 % of patients with trochanteric surface irregularities larger than 2 mm on conventional radiographs have peritendinous fluid changes around the gluteus medius and minimus tendon insertions (positive likelihood ratio of 17.5). These findings are of importance to orthopedic surgeons and rheumatologists. In many institutions, a preoperative MR before arthroplasty of the hip is performed when an abductor tendon lesion is suspected clinically. If abductor tendon pathologies are detected on MR images (Figs. 13.3, 13.4, 13.5, and 13.6), the orthopedic surgeon may change the surgical approach. In the presence of an abductor tendon tear, a possible posterior approach is chosen and the abductor tendons are reattached during the implantation of the hip arthroplasty. In case of no tendon pathology, a minimal invasive anterior approach without touching the abductor tendons is performed [12]. Many clinicians, even orthopadic surgeons, seem to underestimate tears of the abductor tendons as a cause of hip pain and treatment option for hip pain. Cormier et al. [13] showed that almost half (45 %) out of 459 French orthopedic surgeons, who were contacted by mail, were not aware of the possibility that tendon tears can occur in the rotator cuff of the hip. Only 13 % (60/459) had performed surgical repair of a gluteal tendon which had been correctly diagnosed preoperatively. However, surgical treatment of gluteal tendon tears has been shown to be very effective [14]. Lequesne and colleagues [14] showed a complete or total remission of symptoms in 90 % after the surgical treatment of abductor tendon tears. Kagan [15] reported seven patients treated with success by gluteus medius tendon repair. Moreover, Miozzari et al. [16] demonstrated that 75 % of all patients with late repair of abductor dehiscence after transgluteal approach for hip arthroplasty were satisfied.


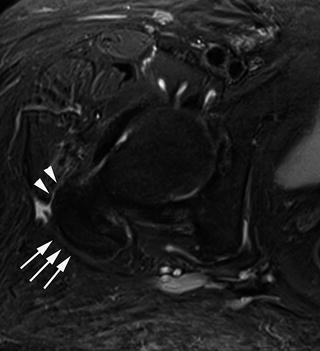
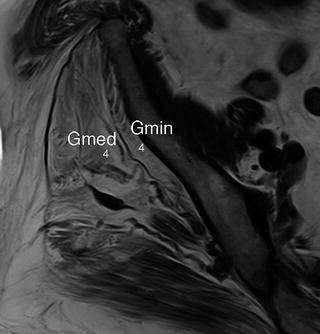

Fig. 13.3
T2-weighted coronal image of an 82-year-old female patient (TR 4,000 ms, TE 70 ms, slice thickness 6 mm) shows a full thickness tear of the gluteus minimus tendon. No tendon attachment (white arrowheads) onto the anterior facet of the greater trochanter is shown

Fig. 13.4
T2-weighted coronal image of an 82-year-old female patient (TR 4,000 ms, TE 70 ms, slice thickness 6 mm) shows a full thickness tear of the gluteus medius tendon. No tendon attachment (white arrowheads) onto the lateral facet of the greater trochanter is shown
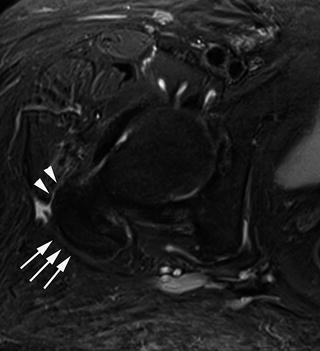
Fig. 13.5
Corresponding transverse STIR image in the same patient as in Figs. 13.3 and 13.4 (TR 4,300 ms, TE 37 ms, TR 150 ms, slice thickness 6 mm). MR image shows a full thickness tear of gluteus minimus and medius tendon. The image demonstrates the missing tendon attachments. Additionally, slight peritendinous fluid is present (white arrows missing gluteus medius tendon attachment and white arrowheads missing gluteus minimus tendon attachment)
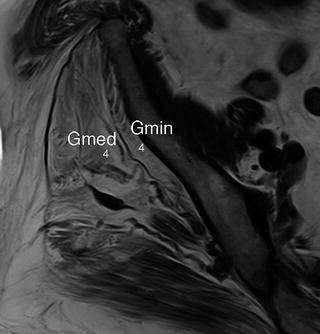
Fig. 13.6
T1-weighted transverse image (TR 500 ms, TE 13 ms, slice thickness 5 mm) illustrates fatty muscle infiltration of gluteus minimus muscle (Gmin) grade 4 according to Goutallier classification and also fatty infiltration of the gluteus medius muscle (grade 4). Gmin M.gluteus minimus, Gmed M.gluteus medius
There are also a relationship between gluteal tendon abnormalities at the insertion onto the greater trochanter and bursitis as previously been reported [17, 18]. Bird et al. [18] described 24 patients with trochanteric pain of which 8 % showed a bursitis comparable to the cases in this present study where increased bursal fluid was seen in 9 % of all patients (14/150). Kingzett-Taylor et al. [5] demonstrated that 14 of 35 patients (40 %) with a tendinopathy or an abductor tendon tear also had increased amounts of bursal fluid. However, this does not necessarily mean that there is a symptomatic bursitis because bursal fluid is a nonspecific reaction to a number of different abnormalities. Blankenbaker et al. [19] commonly found bursal fluid and peritrochanteric edema in asymptomatic hips (88 %).
Iliopsoas Musculotendinous Unit: Iliopsoas Tendinitis
The iliopsoas muscle can be followed inferiorly on transverse images because it proceeds from a medial and anterior location to a lateral and posterior location. MRI can depict the psoas tendon attachment onto the lesser trochanter of the femur, whereas most of the iliacus attaches onto the proximal femoral shaft without a tendon. T1-weighted transverse images will delineate the psoas tendon and intramuscular portions of iliacus tendon separated by a thin cleft of increased signal on T1-weighted images [20, 21]. The increased signal is produced by the fatty fascia from the iliacus tendon.
The normal iliopsoas tendon extends anterior to the anterior superior labrum at the level of the hip joint. The anterior hip images best in transverse and sagittal planes while the patient is lying in a supine position.
Iliopsoas tendinopathy has been reported as groin or trochanteric pain getting worse during active flexion and adduction of the hip. Patients who participate kicking related sports as well as soccer or hockey are involved [22]. Daily activities such as walking or getting up or down from a chair can also produce typical pain [23]. Treatment suggestions are resting, anti-inflammatory medication and stretching [24]. MR shows in patients with a present tendinopathy a thickening of the tendon or an increased intrasubstance signal intensity of the tendon along its course or at the insertion. Additionally peritendinous fluid seen as high signal intensity on T2-weighted images and distension of the iliopsoas bursa can also be seen [21]. Partial tendon tears appear with focal fluid within the tendon or as focal discontinuity of the tendon fibers. The localization of the tear often involves the iliopsoas tendinous attachment close or at the lesser tuberosity attachment. The most severe tendon injury, a complete tear, appears to be more function of age, gender, and possible underlying comorbid nonneoplastic conditions, rather than a consequence of athletic injury [25] (Figs. 13.7 and 13.8).
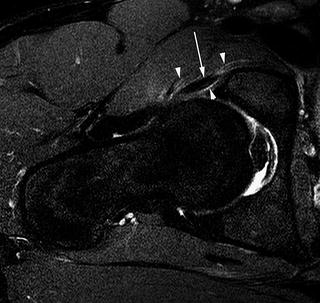
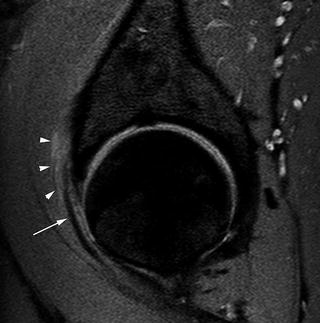
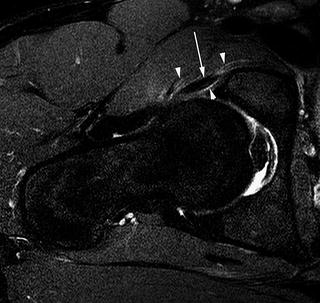
Fig. 13.7
T2-weighted fat-saturated axial TSE sequence of a 22-year-old male patient (TR 3,641 ms/TE 62 ms, slice thickness 3 mm) shows an iliopsoas tendinitis with increased peritendinous signal (white arrowheads) around the iliopsoas tendon (white arrow). The iliopsoas tendon shows an increased signal within the tendon structure
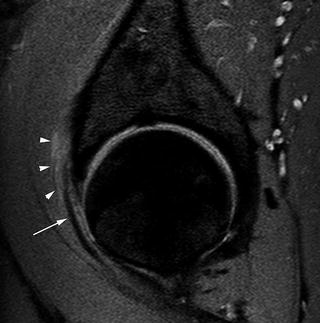
Fig. 13.8
Intermediate-weighted sagital TSE sequence of a 22-year-old male patient (TR 5,777 ms/TE 30 ms, slice thickness 3 mm) shows also the iliopsoas tendinitis with increased peritendinous signal (white arrowheads) around the tendinopathic iliopsoas tendon (white arrow)
Hip Bursae
The hip is surrounded by 15–20 bursae [26]. Most of the cases can be diagnosed clinically and the treatment is conservative; MR imaging is very helpful in detection and localizing of fluid collections around the hip. Characteristic sites for bursae are the iliopsoas bursae and trochanteric bursae.
Trochanteric Bursae and Bursitis
A complex of three bursae has been described over the facets of the greater trochanter. The trochanteric bursa is located between the gluteus medius muscle and the posterior facet of the trochanter. On axial T1-weighted images, the nondistended trochanteric bursa may be seen as a thin band posterior to the trochanter with intermediate signal.
The subgluteus medius bursa lies between the gluteus medius tendon and the lateral facet of the greater trochanter. The subgluteus minimus bursa has its location between the gluteus minimus tendon and the anterior facet of the greater trochanter. There is a relationship between contour or surface irregularities of the greater trochanter and increased bursal fluid in the bursae complex. If surface irregularities are larger than 2 mm appear, 15 % of the patients will show increased bursal fluid [11].
Patients with a bursitis commonly presenting lateral hip pain. Trochanteric bursitis is a well known injury in athletes such as ballet dancers or secondary to blunt trauma occurring during playing football or hockey.
On MR imaging the bursitis is shown as an increased fluid within the bursa as hyperintense signal on T2-weighted images. Often increased peritendinous signal adjacent to the bursa and the abductor tendons are shown (Figs. 13.9 and 13.10).
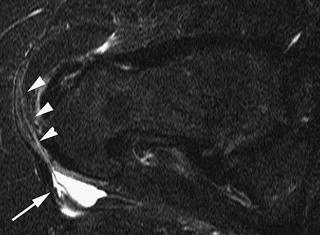
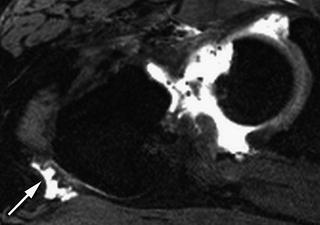
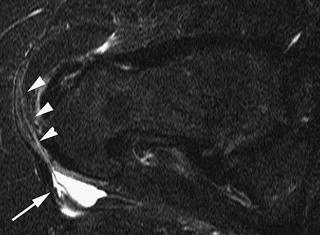
Fig. 13.9
Axial STIR (short tau inversion recovery) image (TR 4,890 ms/TE 245/TI 150 ms, slice thickness 6 mm) demonstrates a bursitis trochanterica (arrow) in a 52-year-old female patient. Also note the peritendinous fluid adjacent to the abductor tendons
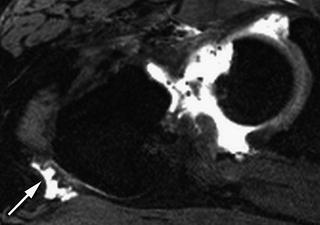
Fig. 13.10
T2-weighted axial 3D sequence at saturated axial TSE sequence of a 47-year-old male patient (TR 11.3 ms/TE 4.9 ms, slice thickness 0.7 mm) demonstrates also a bursitis trochanterica (arrow) in a 47-year-old female patient
Iliopsoas/Iliopectineal Bursa and Bursitis
It is the largest bursa in the body and can extend from the region of the lesser trochanter upward into the iliac fossa. The iliopectineal bursa around the hip joint might communicate with the hip joint in 15 % of the people because there is a hiatus between the pubofemoral and iliofemoral ligaments. That is why in MR-arthrograms contrast agent might extend into the iliopsoas [27].
A bursitis is believed to be caused by irritation of the iliopsoas as moves over the iliopectineal eminence of the femoral head. Patients present anterior hip or groin pain. This pain tends to exacerbate during hip extension and relieved during hip flexion and external rotation.
Associated sports are running, soccer, gymnastics, or resistance training.
On MR imaging the bursitis is displayed as a well-defined cystic mass along the iliopsoas tendon and has a thin wall. After contrast media application, the wall enhances peripherally [28] (Figs. 13.11 and 13.12).
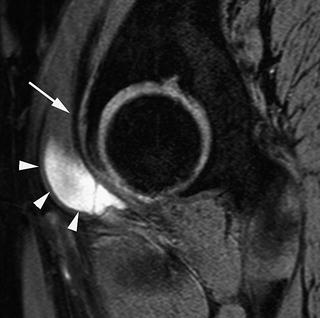




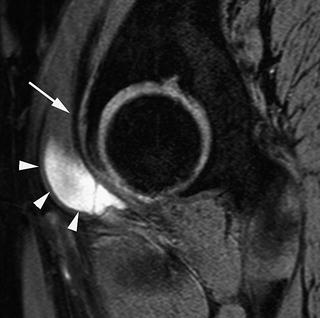
Fig. 13.11
T2-weighted sagittal 3D sequence of a 57-year-old woman (TR 25.2 ms/TE 8.6 ms, slice thickness 1.7 mm) shows an iliopsoas/iliopectinea bursitis as a thin-walled cystic lesion (white arrowheads) directly adjacent to the iliopsoas tendon (white arrow), which shows a normal hypointense signal on T2-weighted image
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree