and Alfredo Blandino1
(1)
Department of Radiological Sciences, University of Messina, Messina, Italy
Several extraintestinal complications have been associated to IBD. In particular, it has been noted that up to 36 % of patients with CD have at least one extraintestinal manifestation and 25 % have more than one extraintestinal complication. Moreover, the development of one extraintestinal complication appears to increase the risk of developing others [1].
This chapter discusses the usefulness of MREg/MREc even in detecting extraintestinal complications, which may sometimes be the initial presenting symptoms or, most commonly, be hidden by the major intestinal symptoms.
Abdominopelvic extraintestinal complications of CD, which can involve the hepatobiliary and pancreatic system, genitourinary system, musculoskeletal and cutaneous systems, as well as the peritoneum, are well depicted on MR of the small bowel [2]. It is therefore mandatory for the gastrointestinal radiologist who performs the examination to have a basic knowledge of which are the main extraintestinal complications and of their relative imaging characteristics.
Different factors may be responsible for extraintestinal organ involvement, and this can make difficult the differentiation between true extraintestinal manifestations (i.e., primary systemic affections directly caused by IBD) and secondary extraintestinal complications of the disease, caused, for example, by malnutrition, chronic inflammation, or side effects of therapy. Furthermore, even if some of these complications may not correlate with disease activity (e.g., primary sclerosing cholangitis and ankylosing spondylitis), generally, they tend to follow the clinical course of disease and may have a high impact on the patient’s life quality, morbidity, and also mortality [2, 3].
5.1 Hepatobiliary Complications
The hepatobiliary manifestations of IBD include primary sclerosing cholangitis, gallstone disease, liver abscess, and portal vein thrombosis.
Even if rare, the involvement of the biliary tract can also be caused by the presence of inflammatory disease in the duodenum or by inflammation of the lesser omentum, which can lead to obstruction of the common bile duct, to ampullary stenosis (Figs. 5.1 and 5.2), or to duodeno-biliary fistulas (Fig. 5.3).
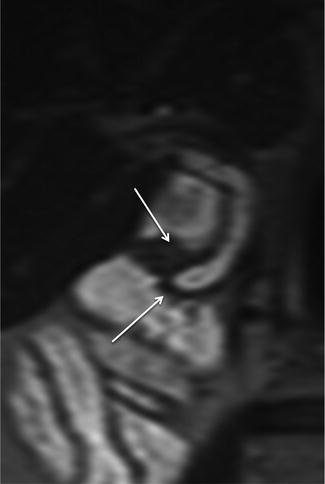
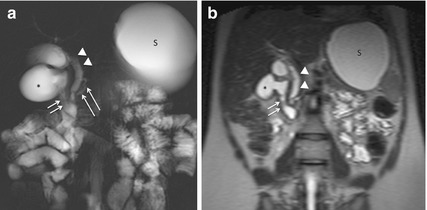
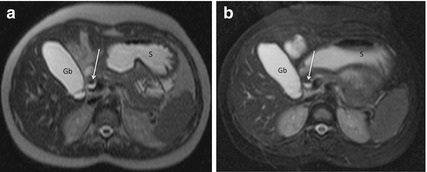
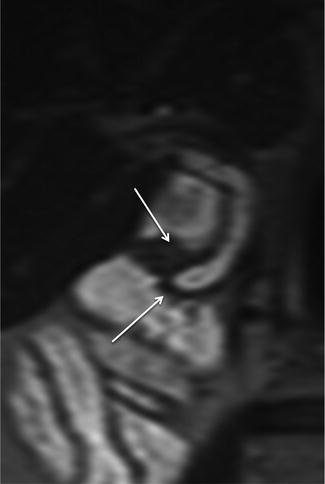
Fig. 5.1
Ampullary stenosis. Magnified coronal HASTE image shows wall thickening in the ampullary area (arrows) with a mild upstream dilatation of the common bile duct
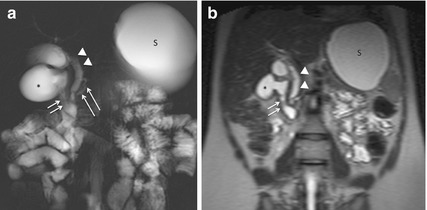
Fig. 5.2
Ampullary stenosis. Coronal MR-fluoroscopy image (a) and coronal HASTE image (b) show the narrowing of duodenal lumen (short arrows in a), due to a concentric thickening of the duodenal wall in proximity of the ampullary area (short arrows in b). The consequent dilatation of the proximal duodenal bulb (asterisk) and of the stomach (S) can also be seen. The common bile duct (arrowheads) and pancreatic duct (long arrows in a) are visibly dilated
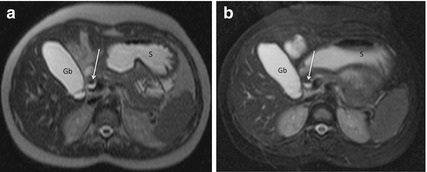
Fig. 5.3
Duodeno-biliary fistula. Axial HASTE image (a) and axial HASTE fat-saturated image (b), obtained along the same anatomical plane. Both MR images show the presence of an air-fluid level in the common bile duct (arrow), due to an enterobiliary fistula. S stomach, Gb gallbladder
5.1.1 Primary Sclerosing Cholangitis
One of the most serious complications of CD is primary sclerosing cholangitis (PSC), a disorder of both intrahepatic and extrahepatic bile ducts [4]. It has an unclear etiology and has a chronic and progressive course, and it manifests itself as inflammation and fibrosis of the medium and large intra- and extrahepatic bile ducts.
At least 5–10 % of PSC patients have CD. However, PSC may occur in 2–4 % of patients with CD, usually in those with colonic involvement and more likely in men than women [5]. Its clinical course bears no relationship to underlying bowel disease; in fact, PSC may develop years either before or after the development of intestinal symptoms [3].
The MREg/MREc protocols, i.e. the MR fluoroscopy, well depict the typical findings of PSC, including multifocal strictures and irregularity of both intra- and extrahepatic bile ducts, leading to the classic “beads on a string” appearance (Fig. 5.4) [3, 6, 7].
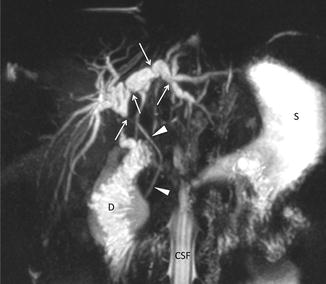
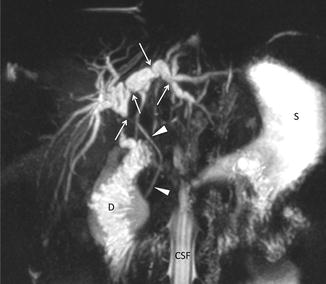
Fig. 5.4
Sclerosing cholangitis. Coronal MIP reformatted image, obtained from multislices HASTE fat-saturated sequence. Both the dilatations and strictures of intra- and extrahepatic bile ducts (arrows) are well seen. Arrowheads: common bile duct; S stomach, D duodenum, CSF cerebrospinal fluid
It is the greatest risk factor for developing cholangiocarcinoma (they both present similar imaging characteristics), from which should be differentiated.
5.1.2 Gallstone Disease
Cholelithiasis is common in patients with CD. The reported prevalence of gallstone disease (GD), defined as current gallstones or previous cholecystectomy for gallstones, in patients with CD, ranges from 13 to 34 % [7–18].
In these patients, age, the site of CD at diagnosis, the number and sites of previous resections, as well as fasting and total parenteral nutrition are all independently associated with cholelithiasis, the pathogenesis of which is multifactorial.
The most important predisposing factor may be considered to be due to the malabsorption of bile acids from the inflamed terminal ileum, which leads to hepatic excretion of bile highly saturated with cholesterol; a further contributory role in the formation of gallstones could be played by a reduced and impaired fatty-meal-induced gallbladder motility, evidenced in most of patients with ileal and ileocolonic disease [18, 19]. Another possibility may be a decreased release and/or hypersecretion of hormones stimulating (e.g., cholecystokinin) or inhibiting (e.g., somatostatin) gallbladder motility [20].
The CD duration is another important risk factor for GD, as well as previous surgery and number of resections are, with particular regard to those involving the ileocecal region, more frequently associated with cholelithiasis and which can be explained with a reduction of transit time in the small intestine and a modification of the ileal microclimate.
The presence of cholelithiasis can be well detected at MR of the small bowel on both HASTE sequences and MR fluorography images (Fig. 5.5).
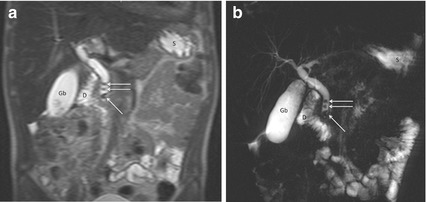
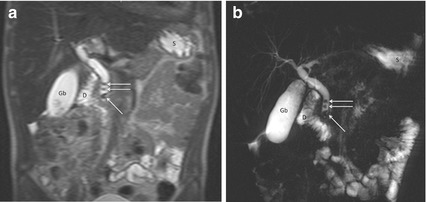
Fig. 5.5
Cholelithiasis. Coronal HASTE image (a) and coronal MR-fluoroscopy image (b) show the presence of small filling defects within the common bile duct, compatible with gallstones (arrows). The cholesterol composition of the CBD gallstones was demonstrated after removal by means of retrograde endoscopic cholangiopancreatography. Gb gallbladder, S stomach, D duodenum
5.1.3 Liver Abscess
Most of the liver abscesses usually occur in patients who have a long-standing history of inflammatory bowel disease, even if a few reports of CD presenting de novo with hepatic abscess have been reported [21, 22]. Long-term steroid treatment, malnutrition, immunological abnormalities, and surgical interventions are additional predisposing factors that may lead to this occurrence.
The pathogenesis of liver abscess has been linked to the interruption of normal mucosal integrity by the intestinal ulcerations. In fact, the invasion of portal venous system by microorganisms facilitates these pathogens to reach the liver.
Clinical manifestations of liver abscesses are variable, and common symptoms are fever, anorexia, weight loss, and abdominal pain that may often be misdiagnosed, as their clinical presentation can resemble an exacerbation of CD.
MR findings characteristic of pyogenic abscesses are high signal intensity on T2-weighted images and low signal intensity on T1-weighted images. Pyogenic abscesses usually possess markedly thick walls and internal septations, which enhance moderately to intensely on early-phase images and demonstrate persistent enhancement on late-phase images (Fig. 5.6).
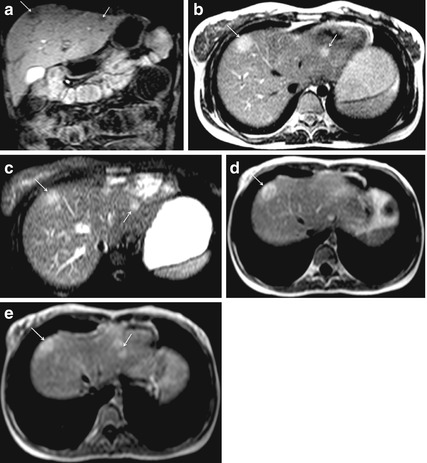
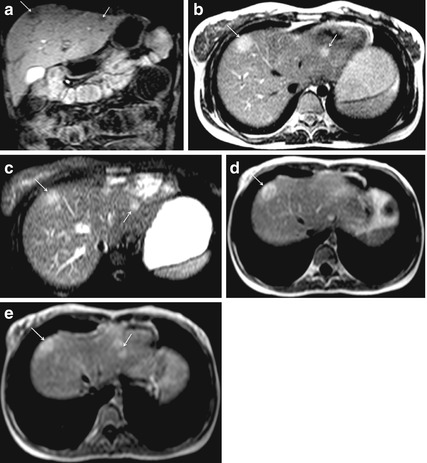
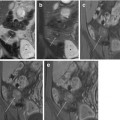
Fig. 5.6
Pyogenic liver abscesses in a febrile patient with Crohn’s disease. Coronal GE T1-weighted fat-saturated image (a). Axial HASTE image (b) and axial HASTE fat-saturated image (c). Axial GE T1-weighted fat-saturated images, obtained after i.v. administration of gadolinium (d, e). MR shows two peripheral hepatic abscesses (arrows) hypointense on T1-weighted image (a) and hyperintense on T2-weighted sequences (b, c) characterized by marked peripheral enhancement on T1-weighted images obtained after contrast medium administration (d, e). The follow-up MR examination, performed after antibiotic therapy, demonstrated the complete resolution
5.1.4 Portal Vein Thrombosis
A rare complication in the nonsurgical clinical setting is represented by portal vein thrombosis.
Generally, patients with IBD are three times more likely to experience thromboembolic events, compared with the general population, with incidence reported to be between 1 and 41 % [7].
The exact cause of the prothrombotic state is still unknown, even if it is likely multifactorial. Risk factors include active inflammation, immobility, surgery, and central venous catheters as well as IBD itself.
During MRE, the signs of abdominal thromboembolic complication can and should be recognized (Fig. 5.7) [3].
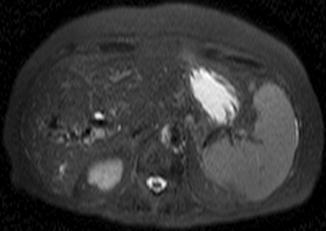
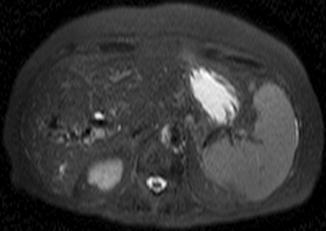
Fig. 5.7
Portal vein thrombosis. Axial HASTE fat-saturated image depicts right portal vein thrombosis with signs of periportal cavernomatosis. Because the patient had contraindications to contrast medium administration (allergy and nephropathy), diagnosis of thrombosis of the portal vein was confirmed by means of ultrasonography
5.2 Pancreatic Complications
Although infrequent, acute pancreatitis and less often chronic pancreatitis may occur in patients affected by IBD as a result of the disease itself or secondary to the medications used during the treatment [23–28]. Many drugs in IBD treatment have the potential to induce acute pancreatitis; in particular, sulfasalazine, 5-aminosalicylic acid, azathioprine, 6-mercaptopurine, and rarely corticosteroids are well known to cause acute pancreatitis as a result of a possible idiosyncratic mechanism. Drug-induced pancreatitis typically occurs within the first weeks after drug therapy begins; the course is usually mild and resolves quickly after discontinuing the drug (Fig. 5.8) [25].


Fig. 5.8
A patient with CD in treatment with sulfasalazine and with a mild edematous form of head pancreatitis. Axial HASTE image shows mild enlargement of the pancreatic head (arrows) without any peripancreatic fluid collection
The IBD-pancreas association is further reflected in many reports of exocrine as well as endocrine pancreatic insufficiency.
The regional inflammatory complications due to duodenal and papillary involvement or biliary complications should also be considered when evaluating the pancreas at MRE.
For what concerns the pathogenesis of chronic pancreatitis, it still remains unclear. It has been considered to be caused by circulating inflammatory mediators rather than directly involved pancreatic tissue. Anyhow, autoantibodies against pancreatic tissue may also play a role in the development of exocrine insufficiency [29–32].
5.3 Genitourinary Complications
The topic of urogenital complications in inflammatory bowel disease is fairly narrow in its spectrum, and it is the expression of the metabolic interrelationships between the two organ systems. The most frequent conditions that fall under this list include ureteral obstruction, nephrolithiasis, fistulous disease involving the genitourinary tract, intrinsic renal disease associated with CD, and some considerations in those who have had surgical procedures that may alter the normal pelvic anatomy.
5.3.1 Ureteral Obstruction
Ureteral involvement is caused predominantly by transmural inflammation of the bowel, which can affect the retroperitoneum and results in ureter and bladder inflammation, fibrosis, or fistula formation [2]. The right ureter is involved most commonly because of the high incidence of CD in the ileocecal region.
Urinary symptoms are often minimal because of the more evident intestinal symptoms, giving evidence of the important role of imaging for early diagnosis.
Heavily T2-weighted sequences, performed in MREg/MREc protocols, help to determine the degree and the location of ureteral obstruction, a valuable method to noninvasively assess the urinary tract of patients affected by CD. Moreover, T1-weighted sequences, performed after intravenous injection of contrast medium, can also provide information about the renal excretory function (Fig. 5.9).
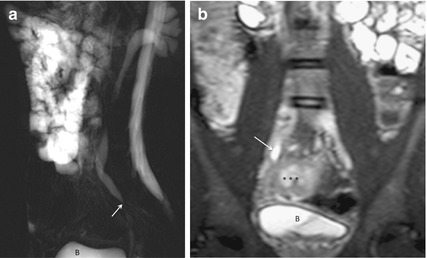
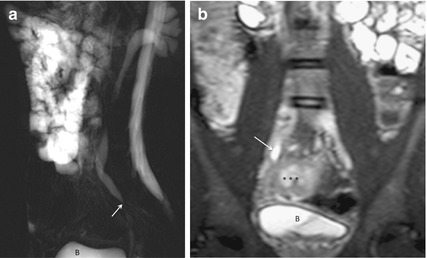
Fig. 5.9
Right ureterohydronephrosis due to pelvic ureter stenosis. Sagittal MR-fluoroscopy image (a) shows tapering of the pelvic ureter with mild degree of upstream dilation of ureteral and renal cavities (arrow). Coronal HASTE image (b) confirms the tapering of the ureter, which is caused by the diseased intestinal segment and the associated perivisceral inflammation (asterisks). B bladder
5.3.2 Nephrolithiasis
Kidney stones are a common manifestation of CD, occurring up to 19 % of patients with IBD, and should always be a part of the differential diagnosis when the patient presents with localized pain. Patients with severe intestinal involvement and a long disease course or who previously underwent extensive ileal resection or ileostomy formation are the ones with higher risk [32–35].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree