EYE: ACUTE AND CHRONIC INFECTIONS
KEY POINTS
- The imaging findings in eye infections are most often nonspecific.
- Imaging can identify findings that aid in the differential diagnosis or causative pathology in a minority of patients.
- Imaging can help differentiate tumor and infection but sometimes complicates that process and leads to the mistaken belief that a tumor is present.
- Imaging can identify complications such as effusions and detachments that can lead to improved outcomes if treated promptly.
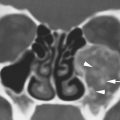
The eye has several coats and internal ocular spaces that can become involved with either acute or chronic infectious disease (Figs. 49.1–49.7). These infections can then cause episcleritis, scleritis, and uveitis. The term endophthalmitis can be applied when the infection affects at least one coat of the eye and an adjacent ocular cavity. Endophthalmitis, however, is generally accepted as a term that is consistent with a very serious infection of the eye seen postoperatively or one that is seeded by a systemic infection (Fig. 49.1). Panophthalmitis is a yet more serious ocular infection, where infection not only involves the internal contents of the eye but also spreads and involves all layers of the eye, with necrosis of the sclera, possible globe rupture, and orbit involvement (Fig. 49.5).
Infections may be local or related to systemic disease. For instance, ocular tuberculosis (TB) will usually be present as part of disease elsewhere but can occur as the only site of infection. This trend is true of any number of viral, bacterial, fungal, or parasitic infections.
Infections can be complicated by hyaloid, choroidal, and retinal detachments discussed in Chapter 45 (Figs. 49.3 and 49.4).
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The anatomy of the eye is discussed in detail in Chapter 44. A working understanding of the coats and spaces of the eye and surrounding preseptal and postseptal soft tissues is useful in analyzing eye infections. The anatomy related to the choroid, retinal, and hyaloid membrane of the eye and various detachments and fluid collections related to these structures that could result from infections are discussed in Chapter 45.
The main vascular tissue in the eye is the uveal tract and outside the eye the conjunctiva. It is important to understand that these anatomic structures essentially envelop the eye inside and out with a slow-flow, highly vascular membrane. It should not be surprising that infection that is transmitted by the blood supply, or that the vascular response to infection, is often initially and predominantly expressed in these structures (Fig. 49.1).
IMAGING APPROACH
Techniques and Relevant Aspects
The eye is studied with ultrasound (US), computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. These infectious conditions may be seen coincidentally on images of the brain and face done for other purposes and, therefore, on images with much lower resolving power than those that might be focused on the eye.
Dedicated studies of the eye/orbit must be done with the highest possible resolution given other constraints on the anatomy that needs to be evaluated. Sometimes, a separate protocol for the eye and orbit is required if both the brain and eye/orbit must be studied definitively. CT and MR protocols are presented in Appendices A and B.
Pros and Cons
CT and magnetic resonance imaging (MRI) are generally not indicated in episcleritis and scleritis, but those conditions may be seen if these studies are done to distinguish these superficial inflammatory conditions from more deep-seated or threatening infections. The signs of uveal tract inflammation seen on CT and MRI are nonspecific findings. These patients are usually not imaged for evaluation of uveitis, but that inflammation may provide clues about the nature of related sinonasal or intracranial abnormalities.
CT and/or MRI may be used to evaluate chronic inflammatory conditions of the eye that mimic other diseases and in which the funduscopic examination may not be definitive. Perhaps toxocara as a cause of leukocoria (Chapter 45) is the best example of that circumstance.
US may not be possible in a painful, infected eye; however, it may be useful and sometimes definitive in a nonpainful chronically infected eye, such as in the diagnosis of ocular cysticercosis. US might be especially helpful to identify detachments and related fluid collections or effusions that can be repaired and drained, thus contributing to a better outcome.

FIGURE 49.1. A–C: Magnetic resonance and computed tomography (CT) images of a patient with HIV and cytomegalovirus infections. In (A), the contrast-enhanced T1-weighted image shows abnormal enhancement of the ciliary body and iris as a manifestation of uveal tract infection (arrow) compared to normal ciliary bodies on the opposite side (arrowhead). In (B), the T2-weighted image shows thickening in the region of the ciliary body (arrow). There is also evidence of fluid or inflammation in the conjunctival sac (white arrowhead). In (C), contrast-enhanced CT on the same patient shows the thickening of the anterior uveal tract on the right (arrows) compared to the left side (arrowhead). D: A patient with ocular syphilis manifesting as uveal tract enhancement (arrows) and thickening compared to the normal side (arrowhead).

FIGURE 49.2. Contrast-enhanced T1-weighted fat-suppressed image showing a focal enhancing mass along the retina (arrow) and further abnormal enhancement and thickening of the choroid (arrowhead). This is due to catscratch disease. This was initially mistaken for an ocular tumor.
SPECIFIC DISEASE/CONDITION
Viral, Bacterial, Fungal, and Other Nonparasitic Infections
Viral, pyogenic bacterial, granulomatous bacterial (including TB, syphilis, brucellosis, and others), and fungal infections are all possible etiologies. Parasitic infections are discussed in a separate section, but they can present an acute phase and in general mimic any other source of infection. The infection can be local or systemic.
Self-limited viral infections are likely the most common (Fig. 49.1). Relatively common infections such as catscratch and Lyme diseases as well as those less common such as TB, syphilis, and fungal infections (Figs. 49.1D and 49.2) can produce retinochoroiditis that can mimic an intraocular mass in its presentation.
When eye findings are seen on imaging examinations of the face and neck, a sinonasal source or intracranial clues to diagnosis may be visible (Fig. 49.3C). Infection may also be secondary to penetrating trauma with a retained orbit or ocular foreign body or seen as a surgical complication (Fig. 49.4).
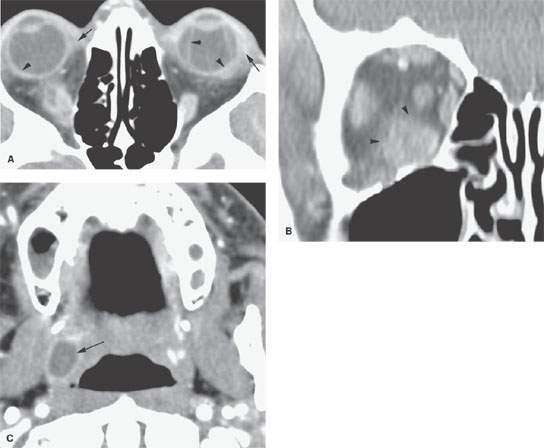
FIGURE 49.3. Patient with orbital and eye involvement due to fungemia. A: There is thickening around the eye on both sides (arrows) that can be reasonably referred to as a periscleritis. There is abnormal enhancement of the sclera and likely choroid bilaterally with a choroidal detachment on the left side (arrowheads). B: Involvement of the inferior rectus muscle and surrounding intraconal soft tissues likely due to hematogenous spread to the muscle. C: Further evidence that this is due to systemic disease manifesting as a proven fungal tonsillar abscess (arrow).
Prevalence and Epidemiology
These tend to be sporadic infections occurring in both the pediatric and adult populations. Immune suppression can predispose to some infections (Figs. 49.1 and 49.3). Recent surgery (Fig. 49.4), penetrating injury, risky behavior (Fig. 49.5), or sinonasal infection that spreads to the orbit considerably raises the risk. Populations geographically at risk for certain exposures, such as to local parasite populations or Lyme disease, will raise the odds of those ocular infections.
Clinical Presentation
These infections typically present with a red and swollen eye and a good deal of pain.
Pathophysiology and Patterns of Disease
The pathophysiology of inflammatory conditions and their appearance on imaging studies is discussed in general in Chapter 13.
Episcleritis is inflammation of the tissue between the conjunctiva and sclera, and scleritis is an infection of the sclera itself; they may coexist (Figs. 49.1B and 49.5). Bacterial, viral, granulomatous, fungal, and parasitic infections are possible etiologies.
Scleritis and episcleritis are manifest by thickening and enhancement of the scleral margin and edema of surrounding fat. In posterior scleritis, fluid may be visible in the Tenon space, and there may be associated choroidal detachment best seen on contrast-enhanced T1-weighted fat-suppressed and T2-weighted fat-suppressed images (Figs. 49.3–49.5). Other detachments are possible as well. Scleral perforation is rare (Fig. 49.5); staphylomas may form at areas of scleral weakening.
Some infections produce primarily a chorioretinitis.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
Scleritis and episcleritis are manifest by thickening and enhancement of the scleral margin and edema of surrounding fat usually easily seen on contrast-enhanced CT and best seen on contrast-enhanced T1-weighted fat-suppressed and T2-weighted fat-suppressed images (Figs. 49.3–49.5). In posterior scleritis, fluid may be visible in the Tenon space, and there may be associated choroidal detachment (Chapter 45) (Figs. 49.3 and 49.4). Scleral perforation is rare; staphylomas (Chapter 46) may form at areas of scleral weakening.
The thickening and enhancement of the choroid, ciliary body, and/or iris seen on contrast-enhanced CT and best on contrast-enhanced T1-weighted MR images are nonspecific findings (Fig. 49.1). These patients are usually not imaged for evaluation of their uveitis. When focal, such changes can be mistaken for tumor (Fig. 49.2).

FIGURE 49.4. Endophthalmitis secondary to trauma or surgery. A, B: A patient with bacterial endophthalmitis due to recent eye surgery. Contrast-enhanced computed tomography studies were performed. In (A), there is evidence of inflammation in the periscleral soft tissues including the lacrimal gland (arrows). There is a retinal detachment and abnormal enhancement of the detached membrane as well as the sclera. In (B), the periscleral inflammation (arrows) and detachment are perhaps somewhat more obvious. C, D: A patient with lymphoma presented with diminished vision and a red eyelid. In (C), the T2-weighted image shows thickening of the uveal tract (white arrowheads) also involving the Tenon space (black arrowhead). Image distortion is present anteromedial to the globe (arrow). In (D), the contrast-enhanced T1-weighted fat-suppressed sagittal image with a susceptibility artifact suggestive of a foreign body is clearly seen (arrow). Enhancement correlates with uveitis and tenonitis (arrowheads). During surgery, a metal fragment was found and removed, after which the vision improved. Biopsy showed no evidence of lymphoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree