EYE: INTRAOCULAR NEOPLASTIC MASSES AND VASCULAR MALFORMATIONS
KEY POINTS
- The imaging findings in intraocular masses are often nonspecific.
- Imaging can identify findings that aid in the differential diagnosis or causative pathology in most patients.
- Imaging may help differentiate benign and malignant neoplasms but sometimes complicates that process and leads to the mistaken belief that a malignant tumor is present.
- Imaging can identify complications such as effusions and detachments that can lead to improved outcomes if treated promptly.
Intraocular neoplastic masses may be inconsequential and discovered incidentally on physical examination or imaging studies. Vascular malformations, even though they are developmental, are considered in this chapter because they may mimic true neoplasms both in their appearance, presentations, and propensity to cause associated detachments. Benign neoplasms need to be differentiated from malignancies, which is something that is sometimes not possible based on imaging. Both benign and malignant tumors, as well as vascular malformations, can cause a detachment.
The most common primary malignancy of the eye in adults is primary malignant melanoma and in children is retinoblastoma. Overall, the most frequent intraocular cancers are metastases from malignancies elsewhere in the body. Metastases and manifestations of systemic malignancies such as lymphoma and leukemia most typically involve the uveal tract because of its being a blood pool.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The anatomy of the eye is discussed in detail in Chapter 44. A working understanding of the gross internal anatomy of the eye is fundamental in analyzing intraocular masses. This must include a clear understanding of the anatomy related to the choroid, retina, and hyaloid membrane of the eye. The various detachments and fluid collections related to these structures that could result from masses are discussed in Chapter 45.
IMAGING APPROACH
Techniques and Relevant Aspects
The eye is studied with ultrasound (US), computed tomography (CT), and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Intraocular masses may be seen coincidentally on images of the brain and face done for other purposes and, therefore, on images with much lower resolving power than those that might be focused on the eye.
Dedicated studies of the eye/orbit must be done with the highest possible resolution given other constraints on the anatomy that needs to be evaluated. Sometimes, a separate protocol for the eye and orbit is required if both the brain and eye/orbit must be studied definitively with CT and/or magnetic resonance imaging (MRI). Specific CT and MRI protocols are presented in Appendices A and B.
Pros and Cons
CT and MR may be the source of an incidental observation of an intraocular mass or used to evaluate masses suspected to be present in a very broad range of circumstances from childhood leukocoria (Chapter 45) to a search for metastatic disease. MR and CT may identify related regional sinonasal or intracranial abnormalities that are known to be associated with certain ocular masses or somehow share in the disease process.
US is often the primary and only study used to evaluate an intraocular mass. US might be especially helpful to identify detachments and related fluid collections or effusions that can be repaired and drained promptly, perhaps contributing to a better outcome.
SPECIFIC DISEASE/CONDITION
Benign Neoplasms, Vascular Malformations, and Other Benign Masses
Etiology
Ocular hamartomas are collections of astrocytic cells in the retina that are usually encountered as part of neurocutaneous syndromes, especially neurofibromatosis and tuberous sclerosis (Fig. 52.1). They tend to be small, en plaque lesions that cannot be detected by imaging until they are >3 mm in width.
Cavernous hemangiomas of the choroid are usually seen as isolated self-limited lesions in patients 10 to 20 years of age (Fig. 52.2A). They can cause retinal detachments and simulate the presentation of uveal melanoma.1 They may occur as part of the eye findings in patients with Sturge-Weber syndrome.
Retinal hemangiomas occur in 25% to 50% of patients with von Hippel-Landau disease and in patients with Sturge-Weber syndrome (Fig. 52.2C–E). Coat disease (Fig. 52.2B), capillary angiectasis of the retina, Eales disease, and multiple retinal aneurysms must be considered in the differentiated diagnosis.
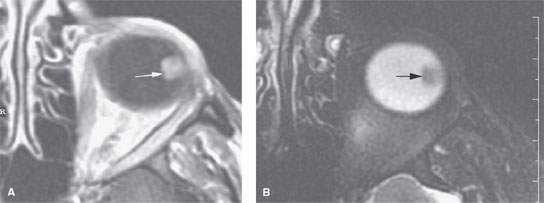
FIGURE 52.1. Magnetic resonance study of a patient with a retinal astrocytoma. A: T1-weighted image shows a well-circumscribed enhancing mass (arrow). B: T2-weighted image shows a low signal intensity discreet mass projecting into the vitreous body (arrow).
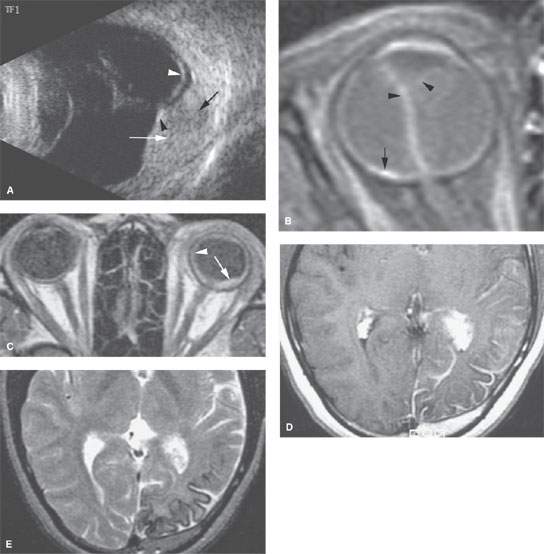
FIGURE 52.2. A series of images showing benign vascular retinal conditions. A: Ocular ultrasound in a patient with a retinal hemangioma seen as an echogenic mass lesion (white arrow) with its base over the choroid. There is an echogenic phlebolith (black arrowhead) showing slight acoustic shadowing (black arrow) and exudative retinal detachment (white arrowhead). B: Contrast-enhanced T1-weighted (T1W) fat-suppressed images in a patient with Coat disease with complete retinal detachment (arrowheads) related to retinal angiodysplasia (arrow). C–E: Magnetic resonance study in a patient with Sturge-Weber syndrome. In (C), a contrast-enhanced T1W image shows the retinal hemangioma (arrow) and generalized increased enhancement within the choroid (arrowhead). In the contrast-enhanced T1W image in (D) and the T2-weighted image in (E), the brain changes consistent with this disease state are present.
Choroidal osteomas are rare uveal tract tumors usually seen in young females. They appear on CT as dense calcific plaques along the choroids, usually near the optic disc (Fig. 52.3).
Masses with their origin in the ciliary body are uncommon. Medulloepithelioma and leiomyoma may both arise in the ciliary body (Fig. 52.4). Medulloepithelioma may mimic retinoblastoma in children and melanoma in adults.1 They are generally endophytic masses that can be seen during funduscopy. When poorly visualized by direct means, imaging may be adjunctive.
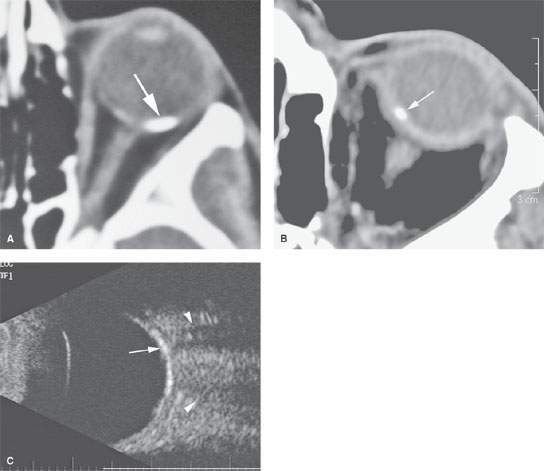
FIGURE 52.3. Three patients with choroidal osteomas. A, B: Typical appearance of these lesions as seen on computed tomography. C: In the third patient, ocular ultrasound shows the choroidal osteoma (arrow) as a calcified plaquelike lesion along the choroidal wall with related posterior acoustic shadowing (arrowheads).
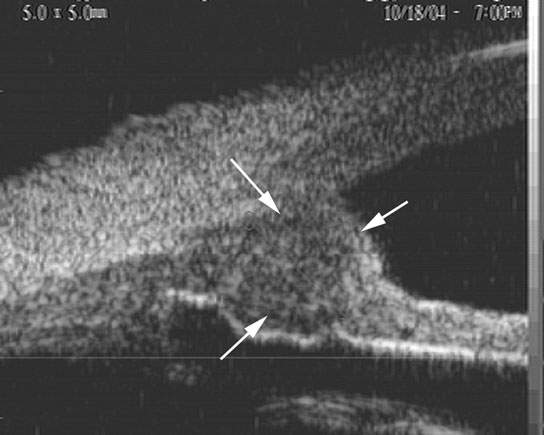
FIGURE 52.4. Medulloepithelioma of the ciliary body. On ultrasound biomicroscopy (50-MHz probe), the tumor is seen as a localized choroidal mass lesion (arrows), the internal structure of which may be varied.
Choroidal nevi are isolated choroidal masses present as gray-appearing subretinal lesions to funduscopy. They usually present without clinical symptoms. Distinguishing these from melanoma is difficult by any means.1 They may cause small subretinal effusions. They are usually diagnosed following enucleation for what appeared to be uveal melanoma.
Retinocytoma is a benign well-differentiated form of retinal tumor, occurring far less commonly than retinoblastoma. It generally presents as a unilateral mass with calcification, accounting for its misdiagnosis prior to surgical resection.2,3
Clinical Presentation
These intraocular tumors may be asymptomatic, or if there is involvement of the macula, they may present with central visual loss. If there is an associated retinal detachment, patients may also present with loss of peripheral vision and leukocoria (Chapter 45). Ciliary body masses may initially present as glaucoma.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
Ocular hamartomas tend to be small, en plaque lesions that cannot be detected by imaging until they are >3 mm in width. They may enhance with contrast on CT and have been reported as isolated lesions.
Cavernous and retinal hemangiomas can be associated with hemorrhagic retinal detachments and mimic the presentation of uveal melanoma (Fig. 52.2). They may be distinguished from melanoma on the basis of history, such as a patient with a known phacomatosis, or imaging findings on MR. Their enhancing CT appearance is nonspecific. They may be distinguished from melanoma by intense contrast enhancement on T1-weighted images or very high signal intensity on T2-weighted images.1
Choroidal osteomas are uveal tract tumors usually seen in young females that appear on CT as dense calcific plaques along the choroids, usually near the optic disc (Fig. 52.3). On MR, these may be seen as a signal void due to their dense calcific nature.
Medulloepithelioma and leiomyoma may produce enhancing masses in the ciliary body (Fig. 52.4). Medulloepithelioma is seen in children at a mean age of 4 years and is extremely rare in adults. Children may demonstrate dystrophic calcifications. Medulloepithelioma may mimic retinoblastoma in children, although it occurs usually in older children, and melanoma in adults because of the hyperintense signal on T1-weighted images.1 Masses are generally endophytic, and they can be seen during funduscopy. When poorly visualized by direct means, imaging may be adjunctive. Neurofibromas, schwannomas, and adenomas may also involve the uveal tract, but these are extremely rare.
Ultrasound
On US, cavernous and retinal hemangiomas are seen as a dome-shaped echogenic mass lesion with a base on the choroid (Fig. 52.2A). The internal structure is very varied. It usually does not calcify, but there may be an echogenic phlebolith noted on the surface of the hemangioma. Exudative retinal detachment and vitreous hemorrhage are seen very often with hemangioma.1
Choroidal osteomas are seen as dense calcified plaquelike lesions along the choroidal wall (Fig. 52.3C).
Ciliary body medulloepithelioma is seen as echogenic mass lesions arising from the ciliary body. They may show cystic changes and calcifications. There are no specific US findings for diagnosis. US biomicroscopy (anterior segment US) needs to be done for ciliary body lesion. It is usually proved by biopsy or after enucleation (Fig. 52.4).
Differential Diagnosis
From Clinical Data
Visualization of a retinal mass or choroidal mass may be masked by effusion, hemorrhage, and/or a detachment; thus, differentiation based on funduscopy may prove difficult. Virtually all of the benign tumors and vascular malformations can to some extent mimic malignant tumors, focal inflammatory diseases, degenerative disease such as macular degeneration, and vascular reactive changes such as Coat disease (Fig. 52.2B) seen in multiple disease states described in Chapters 45, 47, 49, and 50.
Some of the retinal masses are associated with oculocerebral syndromes such as astrocytic hamartoma in tuberous sclerosis and neurofibromatosis (Fig. 52.1) and choroidal hemangioma in von Hippel-Lindau and Sturge-Weber disease; therefore, the differential diagnosis is not difficult.
Choroidal osteomas may rarely be associated with hyperparathyroidism.
In adults, melanoma is simulated by choroidal nevi, macular degeneration, focal uveoscleritis, and metastases.1,4–9
Medulloepithelioma may mimic melanoma in an adult and retinoblastoma in a child.
Choroidal nevi are relatively common and may be indistinguishable from uveal tract melanoma.
The rare retinocytoma may be indistinguishable from retinoblastoma.
From Supportive Diagnostic Techniques
Imaging may be nonspecific, showing only a focal enhancing mass that may contain some calcium and may be associated with a detachment (Fig. 52.2).
Cavernous and retinal hemangiomas can be associated with hemorrhagic retinal detachments and mimic the presentation of uveal melanoma on imaging studies. They may be distinguished from melanoma if there is evidence of an associated condition such as a phacomatosis—for instance, Sturge-Weber syndrome—on images of the brain. Intense contrast enhancement on T1-weighted images or very high signal intensity on T2-weighted images can also help distinguish a hemangiomatous mass from a melanoma.1
Dense calcific plaques along the choroid usually near the optic disc on CT suggest choroidal osteomas (Fig. 52.3).
Enhancing masses in the ciliary body suggest medulloepithelioma, leiomyoma, and rarely neurofibromas, schwannomas, and adenomas of the uveal tract.
Multiplicity of lesions may suggest a relationship to a systemic disease such as a phacomatosis or manifestations of a systemic malignancy.
Medical Decision Making and Treatment Options
Medical
Non–sight-threatening lesions are usually observed, with the exception of retinal capillary hemangiomas. Some physicians recommend early treatment of these, before they enlarge and become less susceptible to treatment.
Surgical
Surgical repair of associated retinal detachments is usually attempted. Retinal capillary hemangiomas may be treated by either laser or cryotherapy.
Surveillance Options
Some lesions may be followed with imaging to confirm their benign nature based on lack of growth over some reasonable periods of time. This is most simply done with US or MRI if US is not definitive. CT should be avoided if possible to reduce exposure to ionizing radiation. If the follow-up is dependent of visualizing calcific changes, then CT may be necessary.
DISEASE ACUITY AND REPORTING RESPONSIBILITY
In most cases, the patient is being evaluated for a known mass, so there is no reason for routine, direct communication with the treatment team. One should immediately report detachments or related fluid collections since some of these might be amenable to surgical drainage. A direct communication is also wise if the mass is likely a malignancy or an incidental finding that might require some prompt intervention.
The report should endeavor to establish the etiology of a mass if it is not known and describe the full extent of the mass and any region findings that might aid in the differential diagnosis or related complications.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








