Fig. 8.1
Ultrasound machine and examiner should be on the patient’s right side to allow for scanning with the right hand
Ultrasound machine and setting. The eye is particularly vulnerable to thermal hazard since the lens and the aqueous and vitreous humors have no cooling blood supply. The ultrasound model and probe used for eye exam should be appropriate to the ophthalmic purpose and ophthalmic preset should be chosen for safety. The depth should be set to visualize all the structures of globe including the optic nerve. Use ophthalmic setting or preset, if available. The gain should be set appropriately to create a hypoechoic posterior chamber. Otherwise, use the “small parts” or digit preset for the best image quality for the eye exam. If gain is set too high, it can cause small artifacts which can confuse the examiner to overcall pathology. In contrast, if gain is set too low, it can cause examiner to miss subtle pathology.
Transducer. The eye is superficial structure which is best visualized with high frequency probe. For point-of-care ocular ultrasonography, High-frequency (7.5–10 MHz or higher frequency range) linear array transducer with small footprint is used to match with the eye socket size (Fig. 8.2).


Fig. 8.2
Linear array transducer
Gel application. Water-soluble ultrasound gel will function as an acoustic coupling medium between the transducer and skin. After the eyes are closed, a copious amount of ultrasound gel should be used to cover the entire eye lid. It will make layer for transducer to float over and will prevent it from direct pressure to the globe. Any pressure to the globe could make discomfort or potentially cause damage to the eye. The gel for an ocular ultrasound exam does not need to be sterile but it is recommended to use sterile gel which is less irritating to the eye or to place a piece of Tegaderm (transparent film dressing) to the closed eyelid before applying the gel (Fig. 8.3). When Tegaderm is applied to the closed eyelid, make sure to get rid of all air bubbles to avoid production of the artifact (Fig. 8.4).



Fig. 8.3
Application of Tegaderm ensuring air bubbles are removed

Fig. 8.4
Application of copious amount of gel on the Tegaderm patch
Transducer Placement and Scanning Technique
The transducer should be well stabilized by resting the hand holding the probe on the patient. The examiner’s arm will be less fatigued when it is held like a pen while fingers and palm can be rested on the maxilla and nasal bridge. There are two views of ocular ultrasound exam; transverse view (the pointer toward patient’s right) (Fig. 8.5) and longitudinal view (the pointer toward patient’s head) (Fig. 8.6). When scanning in both planes, it is very important to sweep the transducer from up and down in transverse plane, side to side in longitudinal plane, tilt and fan the transducer for complete and thorough evaluation. Dynamic scan can be performed by asking the patient to move his or her eyes slowly up and down and side to side and in all four directions while maintaining a closed eyelid. While color flow and pulsed-wave Doppler can aid in evaluating the central retinal artery and vein, their use greatly increases the amount of energy (and heat) in the eye. We do not recommend the use of any eye Doppler setting to evaluate the eye at the present time.



Fig. 8.5
Transverse view

Fig. 8.6
Longitudinal view
Anatomy of the Normal Eye
The normal eye appears as a circular and hypoechoic structure on the ultrasound (Figs. 8.7 and 8.8). It is approximately 24–25 mm in diameter, with minimal individual variation. The eyeball lies on the orbit surrounded fat . The eyeball contains two compartment; anterior chamber and the posterior chamber .



Fig. 8.7
Normal eye anatomy

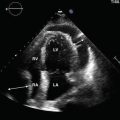
Fig. 8.8
Ultrasound image of a normal eye
The anterior chamber is filled with anechoic fluid (aqueous humor) and is bordered by the cornea anteriorly, iris and anterior reflection of the lens capsule posteriorly. The cornea appears as a thin convex hyperechoic layer which overlies the entire anterior chamber, parallel to the eyelid. It is contiguous with the sclera . The iris and ciliary body are seen as hyperechoic linear structures extending from the peripheral globe towards lens. The lens is biconvex structure which appears anechoic in the center with hyperechoic anterior and posterior margins.
The posterior chamber is filled with anechoic vitreous fluid, posterior to the lens. Vitreous is largely anechoic in a young healthy eye but opacities can commonly be seen in older patients. The posterior border of the globe consists of the retina, choroid and sclera. The normal retina cannot be differentiated from the other choroidal layers on the ultrasound. The choroid attaches firm to the retina on the optic nerve head and the ora serrata which can be observed on the ultrasound scan.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree