EYE: TRAUMA
KEY POINTS
- The imaging findings in eye trauma are critical to treatment decisions including precise surgical planning.
- Imaging can identify findings that are critical to prognosis.
- Imaging may help detect important complications such as infection or retained foreign bodies.
Acute trauma to the eye may be blunt force or penetrating from a wide variety of untoward events. Both mechanisms can also occur during surgery, and both may result in the presence of retained foreign bodies. The chronic effects of ocular trauma due to those mechanisms as well as those due to radiation therapy are discussed in the next section.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The anatomy of the eye is discussed in detail in Chapter 44. A working understanding of the gross internal anatomy of the eye and surrounding preseptal and postseptal soft tissues is fundamental to analyzing ocular trauma. The anatomy related to the choroid, retina, and hyaloid membrane of the eye and various detachments and fluid collections related to these structures that can result from trauma are discussed in Chapter 45.
IMAGING APPROACH
Techniques and Relevant Aspects
The eye is studied with ultrasound (US), computed tomography (CT), and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. These traumatic conditions involving the eye may be seen coincidentally on images of the brain and face and, therefore, on images with much lower resolving power than when those studies might be focused on the eye.
Dedicated studies of the eye/orbit must be done with the highest possible resolution considering the constraints on the other orbital and intracranial anatomy that may need to be evaluated. Sometimes, a separate protocol for the eye and orbit is required if both the brain and eye/orbit must be studied definitively with CT and/or magnetic resonance imaging (MRI). Specific protocols for MRI and CT are presented in Appendixes A and B.
Pros and Cons
CT and US are generally the primary imaging examinations for ocular trauma, with MR used adjunctively and only when the ordering physician is confident that there is no retained metallic foreign body. CT can identify most clinically significant findings, including foreign bodies (Figs. 51.1–51.6), evidence of ocular injury such as hemorrhage, a breach of the sclera, or decompression (Figs. 51.7–51.10). CT can also confidently exclude tension orbit and detect some, but not exclude all, detachments and related intraocular fluid collections. CT can detect gross abnormalities in the vitreous body and gross abnormalities of the anterior segment such as lens dislocation and gross decompression, but it is relatively insensitive to more subtle injury in the anterior segment and the vitreous body (Figs. 45.6D, 51.4A, and 51.6).
CT is a primary study for evaluating delayed complications such as infection and for evaluation of orbital injury that require repair or that may threaten vision (Fig. 51.10).
US may not be possible in a painful, swollen injured eye; however, it can be used often and even in the face of open eye wounds (Figs. 51.4F,G and 51.8C). It is especially useful to localize small anterior foreign bodies (Fig. 51.4F). It also is especially helpful to identify detachments and related fluid collections and effusions that can be repaired and drained, possibly contributing to a better outcome. However, CT is superior in the detection and determination of the size and site of an intraocular foreign body.
MR is used adjunctively in highly selected cases of possibly retained foreign bodies and in delayed complications such as orbital infection1 (Fig. 51.8A,D). It is the primary study for evaluating disorders of the visual pathways that might be related to radiation injury.
SPECIFIC DISEASE/CONDITION
Blunt and Penetrating Trauma and Intraocular Foreign Bodies
Etiology
Blunt and/or penetrating trauma most commonly occur due to motor vehicle accidents, assaults, altercations, sports injuries, gunshot wounds, and a host of less usual circumstances. Postoperative trauma is another relatively common cause of ocular trauma that comes to imaging (Fig. 51.11A).
Any traumatic event may be associated with a secondary infection. Those effects are discussed in Chapter 50, and their end result may follow a final common pathway that leads to phthisis bulbi (a dead eye) (Fig. 51.12) or enucleation and a prosthetic false eye as an end stage.
Clinical Presentation
The injuries are almost always clinically obvious to both the patient and the treating physician; however, there may be so much periorbital and intraorbital swelling that the eyes cannot be examined. In less obvious injury, pain and alteration in vision will be the dominant complaints.
Pathophysiology and Patterns of Disease
Trauma may be blunt and have compressive and/or concussive or penetrating effects. These mechanisms may coexist. Either mechanism can cause lens dislocation, ocular hypotonia in the anterior or posterior segments sometimes with acute globe decompression, intraocular gas, and hemorrhage (Figs. 51.1–51.11A). Hemorrhage can be in the anterior chamber (hyphema), intravitreous, or in association with one or more of the three forms of detachments discussed in Chapter 45 (Figs. 51.4A and 51.6).
Penetrating objects can result in residual foreign bodies remaining embedded in the sclera or intraocular in either the anterior segment or the vitreous body, or they may come to rest in the orbit (Figs. 51.1–51.5).
Postoperative ocular trauma may result from these mechanisms and have the same outcomes as those just discussed for blunt and penetrating trauma. A seroma or hematoma may be present at the operative site. Diminished intraocular pressure (hypotonia) can allow fluid to build up in the choroid and precipitate a suprachoroidal dissection (Figs. 47.4 and 51.11A). Retained surgical material may have punctate gas collections; however, air alone is commonly present after some posterior segment intraocular procedures (Fig. 51.11B).
Scleral banding will result in a characteristic compression of the globe by the banding device (Fig 51.11C). Other implantable devices related to the management of glaucoma may be radiopaque and often have associated fluid collections, which can present a somewhat daunting set of findings if they have not been encountered (Figs. 47.1 and 47.2 and Chapter 47). If such devices are seen, communication with the ophthalmologist is suggested before attaching any particular significance to these devices unless they are the specific focus of the examination.
After enucleation, residual extraocular muscles may be retracted toward the orbital apex, and ball and cup prosthesis frequently replaces the eye (Fig. 51.11D). Early in the postoperative period, inflammatory reactive changes (Chapter 13) may be present and difficult to distinguish from infectious cellulitis. Those changes involute over time.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
Lens dislocation, ocular hypotonia with acute globe decompression, intraocular gas, and hemorrhage may all be visible on CT and MRI (Figs. 51.1–51.11A). Anterior segment decompression may be very subtle and difficult to appreciate on either study (Fig. 51.6A). The normal depth of the anterior chamber ranges from about 2.5 to 3.5 mm. In the context of trauma, a discrepancy ≥2 mm between the depth of the anterior chambers or an absolute depth >5 mm is suggestive of rupture of the posterior sclera.2 Hemorrhage can be located in the anterior chamber (so-called “eight-ball” hyphema), intravitreal space, or beneath one or more of the three forms of detachments discussed in Chapter 45. Acute hemorrhage in the vitreous body can mimic a radiodense foreign body (Fig. 51.4D compared with Fig. 51.7A).

FIGURE 51.1. Computed tomography (CT) study of a patient with a history of penetrating trauma. A: The extraocular metallic foreign body (arrow) is seen in the region of the lateral rectus muscle. On this image, there was no clear evidence of ocular injury. B: This image suggests minor decompression of the globe and suggests, by the gas pattern, that the path of the metallic foreign body had crossed the globe and penetrated its posterior surface (arrows). C: The path of the foreign body through the eye is further confirmed by the intraocular gas in the vitreous in this coronal section and the gas near the exit wound (arrows). (NOTE: While metallic foreign bodies are simple to localize with modern CT imaging, their path of entry and risk to the eye can also be ascertained with a high degree of confidence using simple multiplanar tools on a volume set of data if this is not clear from the clinical examination.) D, E: CT scan of another patient suffering facial trauma and possibly penetrating orbital injury. Some foreign bodies were visible on physical examination. In (D), foreign bodies that were lodged in the sclera are due to leaded glass (arrows). The arrowhead shows gas present; this could just represent air, but it might also represent gas in association with a nonradiodense foreign body. Clinically, it was uncertain whether some of the foreign bodies present were deep and had penetrated through the sclera. This image showed that the foreign bodies were limited to the conjunctival sac or affecting the cornea and sclera only.
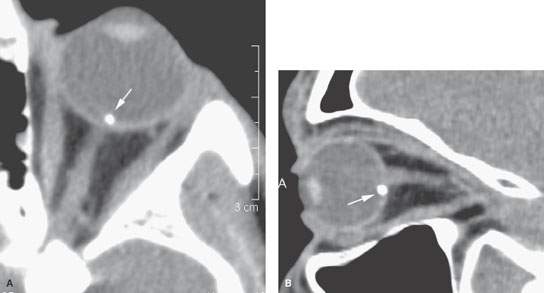
FIGURE 51.2. This patient suffered an injury to the eye that was believed to be due to a metallic foreign body. In (A) and (B) (arrows), the foreign body is correctly localized and is metallic in nature. A diligent search for injury along the pathway of the foreign body was conducted on the images but could not be found. An obvious entry wound was present clinically.
Foreign bodies embedded in the sclera maybe more difficult to detect than those that enter the eye since the sclera is of tissue rather than primarily water density, and some of the material that may enter the eye will approximate tissue density, especially plant matter (Figs. 51.1D,E and 51.3).
Penetrating objects can result in residual foreign bodies remaining embedded in the sclera or intraocular in either the anterior segment or the vitreous body (Fig. 51.1D,E). In general, these are much less likely to be seen on MRI than CT. If a metallic foreign body is suspected, MRI is contraindicated. Since glass contains metal, it is likely wise to avoid MRI in that case as well. These foreign bodies will often contrast well with the mainly fluid density of the anterior segment chambers and the vitreous body. A metallic foreign body is usually easy to find with CT. Glass is variable in its CT density depending on its metal content, and its detection depends on the type of glass, the size, and the location within the eye. Glass intraocular foreign bodies are found easiest in the anterior chamber and most difficult in the corneal surface.3
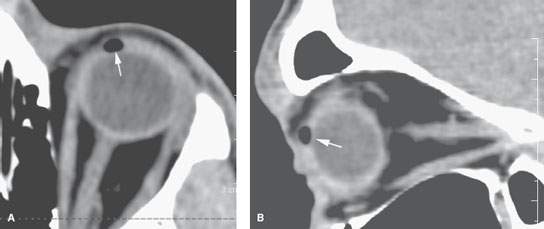
FIGURE 51.3. A patient suffering penetrating orbital trauma. The axial view in (A) and sagittal view in (B) show only gas within the scleral coat. This gas identified an area of nonradiodense debris embedded in the sclera. (NOTE: Gas may be an indication of a foreign body or may just be gas alone.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree