FACIAL AND SINONASAL VASCULAR MALFORMATIONS AND PROLIFERATIVE HEMANGIOMAS
KEY POINTS
- Magnetic resonance imaging and computed tomography in combination are the primary tools for confirming the diagnosis of craniofacial vascular malformations.
- Magnetic resonance imaging and computed tomography are required to evaluate the full extent and potential complication of vascular malformations.
- Magnetic resonance imaging and computed tomography cannot adequately evaluate the angioarchitecture and flow dynamics of high-flow vascular malformations.
Facial and sinonasal vascular malformations and proliferative hemangiomas are most often spontaneous developmental abnormalities that present as a facial mass of obviously vascular etiology. Sometimes the diagnosis is uncertain, especially in deeper lesions. These are most often some variety of venolymphatic malformation (Chapter 9). True proliferative hemangiomas commonly arise in the facial region. Occasionally, especially if associated with intracranial findings, they may be syndromic.
Acquired vascular malformations of the face are most often posttraumatic and may most prominently involve the orbit (Chapter 59) and cavernous sinus (Chapter 75). Cavernous carotid aneurysms will occasionally present as a sinonasal problem (Chapter 75).
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The embryology of congenital-origin vascular malformations is discussed in Chapter 9.
Applied Anatomy
The relevant anatomy of the face and sinonasal structures is discussed in Chapters 78 and 96, and that of the orbit, eye, and optic nerve/sheath complex is discussed in detail in Chapter 44. In particular, the anatomy of the arteries and veins of the face, sinonasal region, and eye and orbit should be reviewed.
IMAGING APPROACH
Techniques and Relevant Aspects
The craniofacial region is studied mainly with computed tomography (CT) and magnetic resonance (MR) techniques and is described in detail in Chapter 78. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate masses or potential vascular malformations are done with contrast including computed tomographic angiography (CTA) or magnetic resonance angiography (MRA) when potentially high-flow malformation or aneurysm is suspected.
Pros and Cons
The use of ultrasound is for the most part restricted to the confirmation of a vascular malformation. Beyond that, ultrasound has little role since it cannot map the entirety of most malformations nor define their precise relationship to important surrounding structures or assess potential intracranial associations, risks, or complications.
Low-flow malformations are studied primarily with magnetic resonance imaging (MRI) to map their soft tissue extent and relative content of blood vessel and lymphatic elements. CT may be used for the same purpose and to assess the malformation’s effects on surrounding skeletal structures. MRI may be more sensitive than CT to possibly related intracranial involvement with these vascular lesions. Both may be used to anticipate transcranial connections and the effects of larger communications that lead to the development of sinus pericranii.
CT may be used primarily in acute situations when the clinical presentation mimics an aggressive infectious process or tumor of possible sinonasal origin. It may be used as the primary tool in high-flow lesions, especially with newer 320 multidetector CT or its equivalent, since CTA with such units can show both angioarchitecture and flow dynamics. CT may also be done first for an emergent evaluation of possible associated infection, hemorrhage, or thrombosis. It is also a first choice in patients too sick or for some other reason unable to complete a very high quality, free of motion artifact, MRI examination. CT is a reasonable screening tool for identifying intracranial extension of disease and intracranial complications. CTA is a good and perhaps preferred screening tool to search for vascular complications such as aneurysms and cavernous sinus or other major dural venous thrombosis.
Catheter angiography can be used to evaluate the structure of high-flow vascular malformations prior to therapy and/or confirm the true flow dynamics if those are not clear from CT or MR images. In general, CTA and MRA remain incapable of clearly evaluating flow dynamics and detailed angioarchitecture, although this is changing with the coming of newer detectors as of mid 2008.
Vascular Malformations and Proliferative Hemangiomas
Etiology
A vascular malformation is usually a spontaneous developmental abnormality that frequently arises in and affects the craniofacial region. It may be acquired, usually due to trauma (Fig. 9.27), and occasionally is syndromic (Figs. 9.21 and 52.2 C–E). The best known of the syndromic variety is Sturge-Weber, which is associated with malformations in the distribution of the trigeminal nerve. Other rare syndromes with multisystem associations such as Maffucci may affect the facial region.
Facial manifestations of vascular malformations are often extensions from a vascular malformation originating elsewhere, such as those primarily of the parotid gland, orbit, or masticator space.
A proliferative hemangioma is typically a spontaneous benign neoplasm that may be of the involuting or noninvoluting type.
Prevalence and Epidemiology
Venolymphatic and other malformations and proliferative hemangiomas are typically sporadic occurrences, but some have syndromic links. They tend to present in infancy and early childhood, but vascular malformations may become clinically apparent into young adulthood. There is no significant gender predilection.
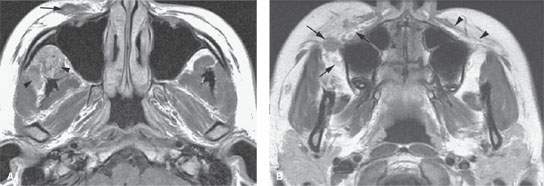

FIGURE 82.1. Magnetic resonance imaging of a patient with a venolymphatic malformation (VLM) involving the face. A: Contrast-enhanced T1-weighted (T1W) image showing the VLM growing along the superficial musculoaponeurotic system (SMAS) (arrow). A deeper component (arrowheads) is present in the infratemporal fossa and involving the masticator space. B: Contrast-enhanced T1W image shows the tendency for the lesions to grow along the SMAS layer and in this case extend into the buccal space (arrows). Compare with the normal SMAS layer on the left. (continued) C: T2-weighted image showing that these lesions are sometimes not obviously of fluid signal intensity, reflecting their slow-flow vascular spaces. In this case, the VLM is manifest as signal intensity less than fat within the buccal space and masticator space spreading just deep to the SMAS (arrows).
Clinical Presentation
These lesions will usually present as a palpable or visible mass, thereby mainly producing cosmetic issues. They may they interfere with vision, speech, chewing, and/or swallowing in an adult and feeding or breathing in an infant. They may bleed, thrombose, or become infected, in which case pain and inflammation and rapid enlargement may be part of the clinical picture. For instance, an unsuspected malformation might produce very severe bleeding during a routine dental procedure. The lesions may also be discovered incidentally on imaging findings done for other reasons.
Pathophysiology and Patterns of Disease
These conditions are discussed in general in Chapter 9.
A vascular malformation may be associated with similar intracranial malformations or show intracranial extension; thus, initial screening of the entire brain is reasonable.
The venolymphatic malformations frequently contain immune-competent cells that will cause the malformation to swell in response to viral or other upper respiratory tract infections. These and other complications are discussed in Chapters 9 and 59 (Figs. 9.1, 9.3, 9.4, 9.24, 59.3, 59.4, and 59.9). The lesions are usually well defined, but they may have indistinct margins, especially if complicated by hemorrhage (Figs. 9.3 and 9.4). They tend to spread along the superficial musculoaponeurotic system of the face, most often both on its subcutaneous and deeper aspect. Extension to the deeper spaces of the face is common especially to the buccal, submandibular, and masticator spaces and the parotid gland, and even deeper spread to the parapharyngeal spaces is not unusual (Figs. 82.1–82.4). The internal morphology and tendency to enhance will depend largely on the dominant vascular element being lymphangiomatous versus hemangiomatous. Large draining or feeding vessels are not prominent features of the lesions. An associated varix may be present. There are reports in the literature emphasizing the heterogeneity of these lesions and the likelihood of an associated varix1–5; the term varicose capillary angioma has been suggested for some of these mixed lesions. These sometimes cause or are associated with bony dysplasia especially of the mid face and mandible (Figs. 82.2 and 82.3). This may be due to the trophic effects of the flow in the lesion on the adjacent developing skeletal structures.
Arteriovenous malformations and fistulas are not uncommon orbital problems that often present in the clinical context of a “red or injected eye”; however, such a malformation arising in the orbit is relatively rare. Most occur in areas adjacent to the orbit, such as the face or cavernous sinus, and secondarily involve the orbit or manifest orbital symptoms or signs. They are vasoformative lesions responding to a congenital or acquired artery to vein shunt (Figs. 9.27 and 59.10). Their growth is in proportion to mechanical rheologic forces associated with the size and complexity of the arteriovenous shunt. Since treatment varies significantly, more than a casual understanding of their angioarchitecture and pathophysiologic mechanisms is in order and are described in Chapter 9 and in conjunction with cavernous carotid and orbit in Chapter 59. These may be congenital or acquired (Figs. 82.5).
A proliferative hemangioma is typically a spontaneous benign neoplasm that may be of the involuting or noninvoluting type (Fig. 82.6).
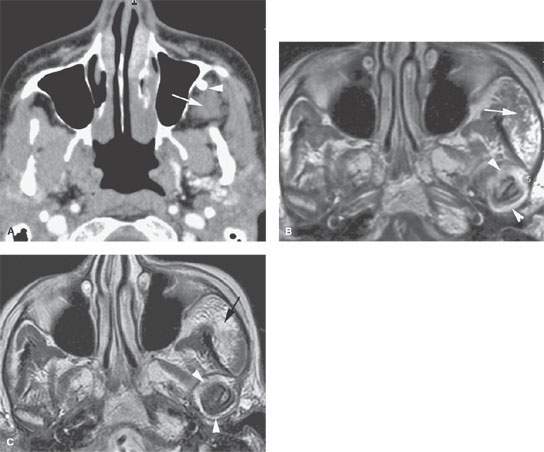
FIGURE 82.2. Computed tomography (CT) and magnetic resonance imaging study of a patient with a slow-flow venolymphatic malformation (VLM). A: Contrast-enhanced CT study showing little evidence of enhancement, with that component of the lesion probably being predominately lymphatic or the filling of the vascular spaces being delayed in the component within the infratemporal fossa (arrow). The phlebolith is a clue to the proper diagnosis. B: Contrast-enhanced T1-weighted image showing the VLM to not be obviously enhancing (arrow). There is abnormal enhancement within the temporomandibular joint (TMJ) space (arrowheads). Part of this enhancement could have been due to secondary altered joint mechanics and secondary TMJ dysfunction. C: T2-weighted image showing the VLM to be brighter than fat (arrow), with this morphology due to slow-flow vascular spaces. The effusion/possible synovitis in the TMJ capsule is easily identified by the presumed distension of the joint capsule and contained fluid-level signal intensity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








