FACIAL NERVE: MALIGNANT CONDITIONS
KEY POINTS
- The acute onset of a peripheral facial nerve palsy does not require magnetic resonance or computed tomography study unless there is reason to believe there is an underlying infectious (other than viral) or neoplastic cause that must be treated with haste.
- Peripheral facial nerve palsy that presents with a different timetable, recurs, or does not recover requires very detailed magnetic resonance and computed tomography studies of the facial nerve to search for a structural lesion that is very likely to be present in those atypical settings for Bell palsy, as cancer is a likely etiology in that situation.
- Atypical presentations of peripheral facial nerve palsy may be due to specifically treatable infectious and noninfectious inflammatory diseases; however, a manifestation of cancer, either perineural or in the parotid gland, is a primary concern in this clinical setting.
- Imaging can be very helpful to triage patients with peripheral facial nerve palsy to the next best step in the diagnostic process.
The most common malignant condition of the peripheral course of the facial nerve, from the labyrinthine segment distally, is by far perineural spread or direct invasion of the nerve by skin and parotid cancers, while primary malignancies of the distal nerve segment nerve are rare. In the canalicular/cisternal segment primary or metastatic skull base and temporal bone malignancies, neurotropic tumor or meningeal spread of secondary cancers can involve the nerve. Primary brain tumors can involve the tumor’s nucleus.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
A diligent search of all segments of the facial nerve, from its nucleus to its peripheral sites of innervation of the muscles of facial expression, is essential for evaluating imaging studies performed in patients with a peripheral facial nerve deficit believed to be due to cancer. The presentation of these cancers may mimic Bell palsy. Bell palsy is only a diagnosis of exclusion in a patient with a slow or stuttering onset or nonresolving peripheral facial nerve palsy; thus, it is important to establish whether imaging findings suggest an alternative diagnosis such as a malignancy to be the likely acute or subacute viral infection or reactivation that causes a Bell palsy1,2 (Chapter 127). This distinction relies heavily on excluding causative pathology, whether inflammatory or neoplastic, with a high degree of confidence.
The computed tomography (CT) and magnetic resonance imaging (MRI) anatomy of the facial nerve must be completely understood, including its brain stem nucleus, its course through the brain stem, its cisternal segment, its course through the internal auditory canal (IAC) and entire facial canal, and its entire course and distribution beyond the stylomastoid foramen. The connections of the facial nerve to the pterygopalatine ganglion should be understood. This anatomy is presented in detail in Figures 104.51–104.54, 175.8, 175.9, 175.15, and 175.16 as well as in Chapters 104 and 175.
IMAGING APPROACH
Techniques and Relevant Aspects
MRI and CT in this anatomic region always requires planning protocols with the highest possible spatial resolution. The principles of constructing such protocols are discussed in detail for such imaging in Chapters 1 through 3.
Specific protocols for magnetic resonance (MR) and CT studies for investigating facial nerve problems in general appear in Appendixes A and B. The facial nerve is typically studied with dedicated contrast-enhanced studies of the temporal bone, especially when the patient is acutely symptomatic. These studies must also include the entire peripheral course of the facial nerve as well as the posterior fossa. In clinical settings atypical for Bell palsy (Chapter 127) or otherwise suggestive of a structural lesion, these studies may need to be repeated at clinically reasonable intervals if no pathology is seen on initial imaging.
Pros and Cons
MRI should be done first since it most confidently excludes causative pathology at all segments (i.e., the brain stem, cisternal, exit canal/foramen, and extracranial segments) of the nerve from its brain stem nucleus to the parotid gland. MRI is more sensitive than CT for excluding intra-axial pathology such as demyelinating disease, pia-arachnoid diseases, and small neoplasms of the nerve that might involve the cisternal segment or the segment within the IAC as well as perineural spread of cancer.
CT may be done as a supplement to most confidently exclude similar pathology within the facial canal from the labyrinthine segment to the stylomastoid foramen and beyond the parotid gland distally. This supplemental imaging may be done as a routine study or only when MRI findings are suspicious for a lesion other than inflammatory enhancement. More typically, supplemental CT is done when the onset of symptoms is atypical for Bell palsy and the cause is not established by MRI or the MRI is suspicious for a cause but not definitive.
If there is obvious potentially acute or subacute infectious disease involving the temporal bone such as acute otomastoiditis or necrotizing otitis externa, then CT may be done initially. It should be noted that malignancy with facial nerve palsy may present initially with a concomitant suppurative process as a complication.
Radionuclide studies are nonspecific in this clinical situation and therefore are not useful diagnostically.
Controversies
Few treating physicians would suggest studying all patients with peripheral facial nerve palsy. For instance, most treating physicians will not image a patient with an isolated, acute onset of peripheral facial nerve palsy because about 75% of these palsies will be transient and will resolve in 4 to 6 weeks whether or not they are treated with steroids or antiviral medications. If the onset is slow or “stuttering” or associated with signs and/or symptoms of possible structural, perineural or other, manifestations of malignant disease, the patient should be studied with meticulous high-resolution CT and/or MRI promptly at the time of initial evaluation. Nonresolving peripheral facial nerve palsy or one that recurs is virtually always studied with imaging, perhaps serially.
SPECIFIC DISEASE/CONDITION
Perineural and Other Secondary Spread of Cancer to the Facial Nerve and Rare Primary Neurogenic Sarcomas
Etiology
The most common malignant condition of the peripheral course of the facial nerve, from the labyrinthine segment distally, is by far perineural spread or direct invasion of the nerve by skin and parotid cancers (Figs. 131.1 and 131.2). Parotid cancers can invade the nerve without necessarily manifesting as true perineural spread. Perineural spread may go proximally to the brain stem and distally to invade the superficial musculoaponeurotic system (SMAS). Specific etiologies with regard to skin cancer are discussed in Chapter 24; those related to parotid cancer are discussed in Chapter 179. These cancers may access the facial nerve directly or grow to the facial nerve along the trigeminal nerve.
Primary or metastatic skull base and temporal bone malignancies may involve the facial canal and the canalicular/cisternal segment. Meningeal spread of secondary cancers can involve the nerve’s canalicular/cisternal segments (Fig. 131.3).
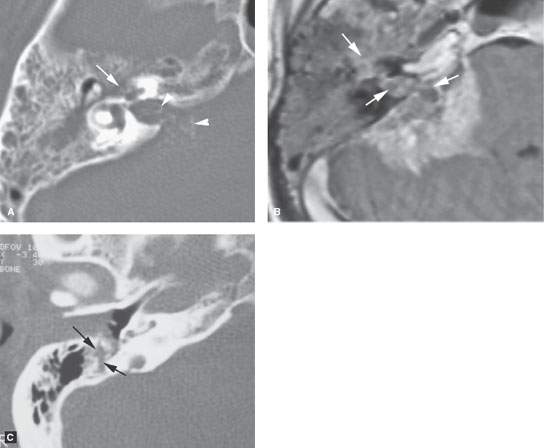
FIGURE 131.1. Two patients with facial nerve involvement A, B: Patient 1. Computed tomography (CT) and magnetic resonance imaging of perineural spread and temporal bone invasion from adenocarcinoma after parotidectomy. In (A), CT shows erosion of the tympanic segment of the facial nerve first genu (arrow) as part of more generalized erosion of the petrous bone including the otic capsule, the internal auditory canal (IAC), and cerebellopontine angle (CPA) involvement showing small calcifications versus impacted mucoid material (arrowhead). In (B), on contrast-enhanced T1 weighted image an enhancing mass involves the facial nerve in the middle ear, IAC, and CPA with extension to the cochlea (arrows) and invasion of the brain. C: Patient 2. External auditory canal carcinoma presenting with facial nerve paralysis due to direct invasion (arrows) of the distal facial nerve canal.
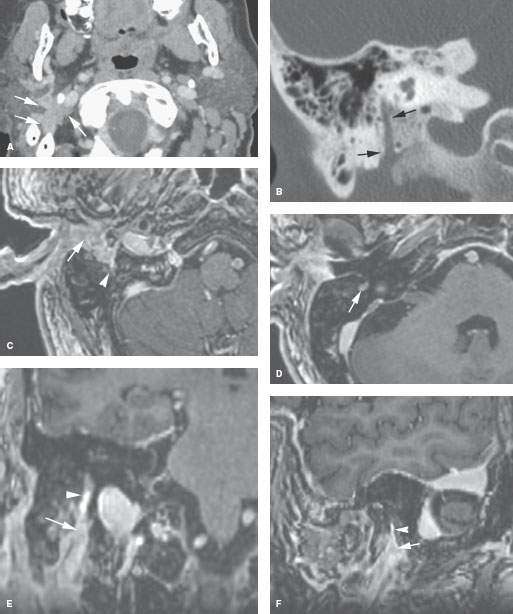
FIGURE 131.2. Imaging findings in perineural spread due to parotid adenoid cystic carcinoma. A, B: Computed tomography showing extension from the digastric groove to the retrostyloid parapharyngeal space causing cranial nerves VII and XI deficits (A). The descending facial nerve canal shows neither remodeling nor erosion (B). C–F: Axial three-dimensional contrast-enhanced T1-weighted images reformatted in (E) and (F). In (C), the cancer surrounds (arrow) and infiltrates (arrowhead) the stylomastoid fat pad. In (D), perineural spread in the descending canal is present (arrow). In (E) and (F), coronal and sagittal reformations, respectively, show the tumor at the stylomastoid fat pad (arrows) and spreading more proximally along the mastoid segment of the facial nerve to the second genu.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree