Normal Anatomy
The uterus is composed of the muscular layer, or myometrium. The body is the main portion of the uterus. The fundus is a more superior portion above the body of the uterus. The areas of the uterus where the fallopian tubes enter are called the cornua . The inferior portion of the uterus is the cervix. Peritoneal reflections are noted both anterior to the uterus, called the vesicouterine pouch, and posterior to the uterus, called the retrouterine recess or, more commonly, the posterior cul-de-sac. The central lining of the uterus is the endometrium, which is firmly adherent to the myometrium. The endometrium varies significantly in thickness in the menstruating female but is more stable in size in a postmenopausal female.
Some of the portions of the female pelvis, such as the broad ligaments and round ligaments, are poorly visualized by imaging. The fallopian tubes run laterally from the upper margins of the uterus. Different segments of the fallopian tube are lateral near the ovaries to medial near the uterus: the infundibulum with its associated fimbriae near the ovary; the ampullary region that represents the major portion of the lateral tube; the isthmus, which is the narrower part of the tube that links to the uterus; and the interstitial (also known as intramural ) part that transverses the uterine musculature.
The ovaries are elliptical in shape, with the long axis oriented vertically. However, the ovaries may be variable in location. In the nulliparous female, the ovary is located along the lateral pelvic wall called the ovarian fossa . This is bounded anteriorly by the obliterated umbilical artery, posteriorly by the ureter and the internal iliac artery, and superiorly by the external iliac vein.
The arterial supply to the uterus is primarily from the uterine artery, which is a major branch of the internal iliac artery. The ovaries have a dual arterial supply, with the main ovarian artery arising from the aorta laterally and slightly inferior to the renal arteries ( Fig. 23.1 ).

Normal Ultrasound Findings/Technique
The two main approaches for visualization of the pelvic organs are use of transabdominal or transvaginal sonography. Both of these techniques are used extensively in the evaluation of the female pelvis. The transabdominal approach visualizes the entire pelvis and gives a global overview. In an emergency situation, the main limitation of this technique is the inability of the patient to have a full bladder. Additionally, visualization of the deep pelvis in certain patients may be limited using the transabdominal approach, as lower-frequency transducers are often utilized. Transvaginal sonography has the benefit of using high-frequency transducers, which produce much better resolution. Small endometrial, adnexal, or ovarian abnormalities are much better delineated with the transvaginal technique. Large masses, such as large fibroids, may be out of the field of view of transvaginal sonography and may be better identified on abdominal sonography. Transvaginal sonography better distinguishes intrauterine fluid collections and adnexal masses from loops of bowel. Both techniques may be utilized depending on the situation.
Uterus
The uterus may be visualized using either the transabdominal and/or the transvaginal technique. The transabdominal technique is optimally performed with a distended urinary bladder. In situations in which transvaginal sonography cannot be fully performed in a timely fashion, a Foley catheter may be used to distend the bladder with saline. The highest-frequency transducer should be used to examine the uterus and ovaries. Usually, this is a 3.5- to 5-MHz transducer. Imaging of the uterus is performed in both longitudinal and transverse planes.
The uterus lies in the true pelvis between the bladder anteriorly and the rectosigmoid colon posteriorly. The uterus may be in variable positions. When describing the uterus, flexion refers to the axis of the uterine body relative to the cervix, whereas version refers to the axis of the cervix relative to the vagina. The uterus is usually anteverted and anteflexed but may appear retroflexed on transabdominal sonography due to displacement by the fluid-filled bladder. The size and shape of the uterus vary with age. In the neonatal stage, the uterus is 2.3 to 4.6 cm in length. It grows in size to approximately 8 cm in length by 5 cm in width and 4 cm in the anteroposterior dimension in the adult. In the multiparous female, the uterus increases both in length and in width with each pregnancy. In the postmenopausal female, the uterus atrophies and ranges in size from 3.5 to 6.5 cm in length in patients over 65 years of age.
On ultrasound (US), the uterus appears fairly homogeneous in appearance. The echogenic line noted centrally within the myometrium is the endometrium. The endometrium varies in size and appearance throughout the menstrual cycle. During the proliferative phase, it begins to thicken in the range of 4 to 8 mm, and by the secretory phase it may range in thickness from 7 to 14 mm ( Figs. 23.2 and 23.3 ).


Ovary
The position of the ovaries is variable. Normally, the ovaries are identified laterally or posterolaterally to the anteflexed midline uterus. However, as the uterus changes position, the ovaries may also change position. At times the ovaries are displaced from the lower pelvis and are best visualized on the transabdominal approach. In these cases, the ovaries may be out of the field of view using transvaginal sonography. On sonography, the ovary has a variable appearance. During the proliferative phase of the cycle, many follicles are identified within the ovary ( Fig. 23.4 ). Before ovulation, one follicle becomes dominant and reaches the size of 2 to 2.5 cm in diameter. Other follicles become atretic. After ovulation, the corpus luteum develops and may be identified by US as a hypoechoic or sometimes isoechoic lesion located within the ovary. Ovarian size varies with the age of the patient. Ovarian volume in the premenarchal female is up to 8 cc. In a menstruating female, normal ovaries may have a volume up to 22 cc. Visualization of the postmenopausal ovaries is more difficult due to atrophy.

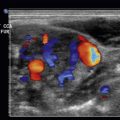
Hemorrhagic Ovarian Cyst
Hemorrhage into a follicular cyst or corpus luteum generates pain and may lead to an emergent presentation. The US pattern varies according to the age of the hemorrhage and the degree of clot formation. The typical appearance is that of a complex mass with internal echoes and some degree of posterior through-transmission. Although fresh blood may be anechoic initially, a hemorrhagic cyst is defined by low-level echogenicity in a fine, lacelike, reticular pattern for the first 24 hours, and this pattern is diagnostically specific ( Fig. 23.5 ). As clot retraction occurs, US may depict triangular or curvilinear echogenic regions at the cyst wall ( Fig. 23.6 ). Fluid-debris levels develop as the clot liquefies. Rupture of a hemorrhagic cyst may be associated with sexual intercourse, exercise, trauma, and pregnancy, and it may involve the right ovary more frequently because the left ovary is protected by a cushion of sigmoid colon. Although cyst rupture may cause massive hemoperitoneum, most patients can be followed with conservative treatment unless they are in unstable condition ( Fig. 23.7 ).



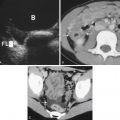
Endometriomas
Endometriosis affects an estimated 10% of premenopausal women. Ectopic endometrial tissue is estrogen sensitive, and it proliferates and bleeds synchronously with the endometrium. Without the normal drainage pathway of the vagina, bleeding from endometrial implants in the adnexa, uterosacral ligaments, or peritoneum often causes cyclic pelvic pain. As much as 80% of ectopic endometrial tissue is found in the ovaries. When larger focal deposits of endometrial tissue are present in the ovary, these endometriomas are detectable at imaging.
Spontaneous rupture of an endometrioma may lead to acute presentation but is uncommon. It causes severe, acute abdominal pain due to chemical peritonitis from the leakage of old blood. A ruptured endometriotic cyst is associated with pregnancy and the large size of the cyst. In nonpregnant patients, rupture commonly occurs at menstruation due to an increase in internal pressure.
Torsion of an endometriotic cyst rarely occurs because of adhesions; therefore severe abdominal pain and the typical findings of ovarian endometriotic cysts are indicative of rupture rather than torsion.
Endometriomas have a variety of appearances on US, ranging from an anechoic cyst to a complex cystic mass with septations and heterogeneous echogenicity. The most typical appearance on an endometrioma is that of a homogeneously hypoechoic, cystic mass with diffuse, low-level internal echoes and posterior acoustic enhancement. This homogeneous appearance has been termed the ground glass pattern . The additional presence of punctate, peripheral, echogenic foci within the cyst wall is a very specific sign for an endometrioma ( Fig. 23.8 ).