Femoral Shaft Fractures
Fractures of the diaphysis (shaft) of the femur are nearly always the result of relatively high-energy trauma. The femur is the longest bone in the body and is one of the strongest. Motor vehicle accidents are the most common cause of femoral shaft fractures. Secondary causes are pedestrians injured by motor vehicles, falls from heights, and gunshot wounds.1 The incidence of femoral shaft fractures in the United States has been estimated at 1 to 1.3 fractures per 10,000 people per year. Femoral shaft fractures occur in a bimodal age distribution and typically are either high-energy injuries in young men or low-energy injuries in elderly women.2 In addition, so-called atypical femur fractures have been described in elderly patients with osteoporosis who have been on long-term bisphosphonate therapy.3,4
Although femoral shaft fractures no longer carry the significant mortality that was previously associated with them, mortality following bilateral femoral shaft fractures can still approach 30%.5,6 This is partially attributed to the fact that blood loss associated with each closed femoral shaft fracture can be as great as 500 to 700 mL (even more if the fractures are open). This amount of bleeding may substantially impact hemodynamic stability, even in a young and healthy patient.6 However, the predominant risk of mortality is related to associated injuries.6
Maintenance of mechanical stability of the femoral shaft is crucial for normal ambulation, and the bone must be capable of withstanding significant axial, bending, and torsional forces during movement. The femur is surrounded by several large muscles that power the hip and knee and provide stability to the limb while standing. Because of the numerous muscle attachments, fractures of the femoral shaft are often markedly displaced and require significant manipulation to achieve reduction.
The femoral shaft is filled with hematopoietic cells and fatty bone marrow. The fatty marrow extravasates into the venous and lymphatic system upon fracture, a process that is further contributed to by instrumentation of the femoral shaft.7,8 It has been theorized that this fat embolization can lead to a deleterious “second hit” or even fat embolism syndrome in patients who have sustained a femoral shaft fracture and who later undergo intramedullary instrumentation.9
Injuries associated with femoral shaft fractures are frequent and can be divided into two broad categories: systemic injuries (head, chest, abdominal, and other remote musculoskeletal injuries) and regional injuries (skeletal injuries ipsilateral to the limb). Commonly associated systemic injuries are head and thoracic injuries. When femoral shaft fractures are associated with a head or chest injury, treatment decisions regarding both the timing and method of fixation become complex.10,11 These issues were more completely discussed in Chapter 1.
Common regional injuries associated with femoral shaft fractures include a second fracture of the proximal femur, typically involving the femoral neck.12 Femoral neck fractures are present in 2 to 6% of all femoral shaft fractures,12 and a high index of suspicion must be maintained in order to diagnose this relatively common problem. Associated femoral neck fractures are sometimes missed on imaging studies, or may be occult in nature, or possibly even occur as an iatrogenic complication of fracture fixation. These associated femoral neck fractures are typically a high-angle Pauwels type C fracture (a vertical shear fracture pattern) of the femoral neck.12 If recognized, stabilization of the femoral neck fracture prior to instrumentation of the shaft is recommended.12 Other associated hip pathologies include posterior hip dislocations, associated acetabular fractures, and, uncommonly, ipsilateral intertrochanteric or subtrochanteric fractures. Associated distal femur injuries also occur with some frequency, complicating the management of the femoral shaft fracture. Supracondylar fracture, isolated condyle fracture, patella fracture, and even ipsilateral tibial plateau fractures can be seen, especially when the femur fracture occurs as a result of a motor vehicle accident.13
Classification
Classification of femoral shaft fractures is straightforward. Although there are several classification systems, a descriptive classification is the most useful and includes fracture location (proximal, middle, or distal), pattern (simple, wedge butterfly, or comminuted), and whether the fracture is open or closed. It is important to identify and characterize associated injuries, as they will often determine the timing and type of initial treatment, as well as the need for involvement of other clinical services. Other classification systems are predominantly used for communication, for research protocols, and for evaluating surgical outcomes. In addition to the anatomic classification, the two most commonly used classification systems are those of Winquist and Hansen14 and the Arbeitsgemunshaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA).15
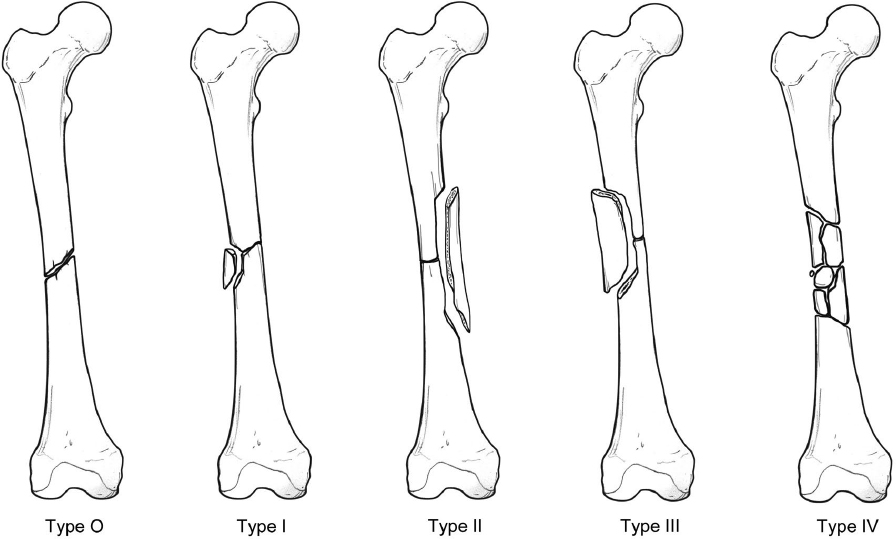
Winquist and Hansen graded fractures 1 through 4 based on their degree of diaphyseal comminution (Fig. 28.1).14 The more comminuted the fracture, the more injury the bone and soft tissue have sustained and the higher the likelihood of encountering problems in obtaining and maintaining adequate alignment and bone healing. Winquist grade 1 fractures are transverse or short oblique with less than 25% comminution. Grade 2 fractures have 25 to 50% shaft width comminution. Grade 3 fractures have more than 50% but less than 100% comminution. Grade 4 fractures have segmental comminution.
The AO/OTA classification system is predominantly used as a descriptor for research and comparing injuries for publication.15 The femur is designated by the number 3; the diaphyseal portion of the bone is designated by the number 2. The fractures are then further subdivided into types A to C. Type A fractures are simple fracture patterns such as spiral, short oblique, or transverse. Type B fractures have a small butterfly fragment or bending wedge. Type C fractures are segmentally comminuted injuries (Fig. 28.2). This classification system was not necessarily developed for treatment, but more for understanding the attributes of the fracture, the time needed for healing, and the potential complications associated with treatment of this injury.

As with all fractures, it is important to classify the fracture as an open versus a closed injury. However, extrapolating the original Gustilo and Anderson16 classification for tibia fractures to the femur does not render justice to the magnitude of injury to the soft tissues following a femoral shaft fracture. In contrast to the tibia, a small puncture wound in the thigh denotes a very high energy fracture because significantly more fracture displacement is necessary to cause an open wound in the thigh. Furthermore, there is usually a significant amount of muscle injury below the skin. Therefore, a femoral shaft fracture with any degree of open skin injury denotes a high-energy injury, and usually warrants a type 3 classification in the Gustilo-Anderson system.
Nonoperative Treatment
Nonoperative treatment of an adult femoral shaft fracture in the era of modern medicine is essentially nonexistent. Because of the extreme morbidity and mortality associated with nonoperative care of this injury, surgical management has become the mainstay of treatment. Nonoperative treatment originally consisted of closed manipulation/reduction with skin or skeletal traction. Traction was adjusted periodically as needed to obtain overall gross alignment of the limb. Bed rest is required for upward of 8 to 10 weeks prior to mobilization. Pins and plaster techniques and cast bracing followed traction treatment but generally showed unfavorable results.17 Fortunately, in 1940, Gerhard Küntscher introduced intramedullary nailing of the femoral shaft.18 His pioneering treatment ushered in today′s trend of operative management over nonoperative management for this fracture.
Surgical Treatment Indications
A fracture of the femoral shaft in an adult is an indication for surgical management. The type and timing of intervention are the key elements of the decision-making process. There are only a few limited reasons not to pursue surgical stabilization of the femoral shaft, and they include patients who are in extremis (with life-threatening injuries), patients who are medically unfit for anesthesia, and possibly Jehovah′s Witnesses who have sustained significant blood loss. All other patients should undergo surgical intervention to repair the femoral shaft in order to stabilize the injury, decrease pain, and restore as much function as possible to the limb.
Surviving the Night
The majority of femoral shaft fractures can be temporarily stabilized with the application of traction; in fact, most patients have a traction splint applied to the femur at the injury scene by the emergency medical services personnel. Fractures of the femoral shaft associated with an ipsilateral femoral neck fracture, vascular injury, or contaminated open wound represent situations with a heightened sense of urgency. Priority is given to treatment of the femoral neck fracture with combined neck–shaft injuries. Implants used to stabilize the femoral neck fracture have implications for the choice of fixation available to treat the femoral shaft fracture. Typically, this situation is managed by stabilizing the femoral shaft fracture with an intramedullary nail that is inserted in a retrograde fashion. Treatment of the femoral shaft fracture is always secondary and may be delayed after treating the femoral neck fracture if indicated by the patients’ clinical condition. Concomitant vascular disruption is another surgical emergency. Reestablishing blood flow to the injured lower extremity as soon as possible is of utmost importance. Fracture stabilization enables limb length to be restored and provides the necessary stability to the limb to protect the subsequent vascular repair. Most often, initial bone stabilization in the setting of a vascular injury is obtained by placement of an external fixator in order to minimize the length of time required for procedure. The external fixator is subsequently exchanged for an intramedullary nail on a delayed basis. Following the vascular repair, prophylactic ipsilateral leg fasciotomies are frequently necessary. Femoral shaft fractures associated with open wounds represents a continuum with respect to the degree of soft tissue injury and wound contamination. Surgical debridement of small and relatively clean inside-out–type wounds may be delayed more than large wounds with gross contamination. Grossly contaminated wounds are best treated with expedient surgical debridement.
Treatment Options
Surgical treatment of femoral shaft fractures can be quite varied, depending on institutional resources, the experience of the surgeon, and the clinical situation. The type and timing of fixation depend largely on variables beyond the fracture itself. The associated injuries to the patient are as important as the fracture type and location. Other factors that affect surgical decision-making include the amount of local soft tissue injury and whether the fracture is open or closed. Alternative forms of surgical treatment include external fixation, plate fixation (compression plating, bridge plating, or percutaneous bridge plating), and intramedullary nailing.
Intramedullary nailing of the femur has become the standard by which other treatments are measured. Although it remains the most common form of treatment, several options and controversies exist regarding intramedullary nailing of the femoral shaft. These include such factors as the direction of insertion of the nail (either antegrade or retrograde) and how the nail is secured to the femur (standard locking, cephalomedullary locking, static locking, or dynamic locking). Other decisions regarding nailing of the femoral shaft include patient positioning and the use of a fracture table versus manual traction. The patient may be positioned supine or lateral, and may be placed on a fracture table or a radiolucent table with the leg draped free. Finally, there are several special situations that influence treatment of the femoral shaft fracture, including the presence of an associated femoral neck fracture, a severe soft tissue injury, open fracture with segmental bone loss, an associated arterial injury, the multiply injured patient, patients with a significant chest injury, and patients with an associated head injury. Thus, there are numerous patient and injury factors that influence the decision-making process. All of these scenarios are discussed in detail in this chapter.
Surgical Anatomy
The femoral diaphysis comprises the region beginning 5 cm below the lesser trochanter and ending 8 to 9 cm above the knee joint. The region proximal to this is considered the subtrochanteric femur, and the region distal is considered the supracondylar portion of the femur. The femoral head and neck join the proximal femoral shaft at the intertrochanteric line. The greater trochanter projects proximally, laterally, and posteriorly from this junction and serves as the site of attachment of the gluteus medius and minimus tendons. The lesser trochanter projects in a posteromedial direction from this junction and serves as the site of attachment of the iliopsoas tendon. The proximal femur consists primarily of cancellous bone in the proximal metaphyseal region and tapers in width distally, transitioning into dense cortical bone near the level of the lesser trochanter. This dense cortical bone comprises the majority of the femoral shaft and is narrowest in diameter at the isthmus (proximal third of the femur).
Distally, the femoral shaft flares out and transitions into primarily cancellous bone and terminates at the femoral condyles. In the coronal plane, the axis of the femoral canal projects out the proximal femur through the piriformis fossa, making this site the ideal starting point for intramedullary nailing. The trochanteric portal is lateral to the piriformis fossa, so trochanteric portals are off-axis from the medullary canal. This leads to a tendency to varus malreduction if a nail that is straight in the coronal plane is inserted from the trochanteric portal. Because of the anatomy of the proximal femur, femoral nails that are intended for trochanteric entry typically have valgus bends that vary from 4 to 10 degrees.19 In the sagittal plane, the femoral shaft has an anteriorly directed bow. Harma et al20 measured the radius of curvature of this bow along the posterior femoral cortex in 104 normal subjects and found an average radius of curvature of 77 cm. This was significantly lower than the radius of curvature of the intramedullary nails they measured, which ranged from 150 to 300 cm. Furthermore, they found that the anterior bow increased with age in women until the age of 55 years, but was insignificantly correlated with age in men.
In the axial plane, the distal femoral condyles project posteriorly from the epicondylar axis, with the medial condyle projecting further than the lateral condyle. A line tangent to the most posterior projection of both the medial and lateral femoral condyles represents a convenient reference to compare with the axis of the femoral head and neck and quantifies the degree of twist, or torsion, in the bone. Yoshioka and Cooke21 defined the femoral head and neck axis by a line connecting the center of the femoral head with the midpoint of the narrowest segment of the femoral neck and referred to this axis as the functional neck axis (Fig. 28.3). If this axis projects anteriorly from the posterior condylar axis, the condition is referred to as anteversion. If it projects posteriorly from the posterior condylar axis, the condition is referred to as retroversion. Yoshioka and Cooke found this value on 32 cadavers to average 13.1 degrees of anteversion.

Femoral torsion can vary widely among individuals. Hoagland and Low22 reported a range of −2 to + 35 degrees. However, there is less variation between the limbs of the same individual. Kingsley and Olmsted23 reported an average side-to-side difference of 1 degree, whereas Reikerås et al24 reported a difference of up to 11.8 degrees.
Knowledge of anteversion is very important in understanding possible rotational mismatches following fixation of a femoral shaft fracture. For practical purposes, it must be assumed that the degree of anteversion in one limb is the same as that in the other, although the variation as noted above is recognized. Measuring the degree of femoral torsion clinically is difficult.25 Multiple techniques including physical examination, plain radiographs, ultrasound, and computed tomography (CT) scan have been described. Tornetta et al26 described the use of a standard C-arm machine to measure the degree of anteversion of the uninjured limb intraoperatively during intramedullary nailing of 12 unstable femoral shaft fractures, and was able to keep the side-to-side torsional difference between the limbs in all patients less than 10 degrees as confirmed by postoperative CT scan. The technique uses the goniometer on the C-arm machine to measure the value of a true lateral of the hip and a true lateral of the knee, with the difference between the values representing the amount of femoral version. The true lateral of the knee is obtained by superimposing the posterior femoral condyles and is well defined and relatively easy to do. One limitation of this technique is that a true lateral of the hip is difficult to define and reproduce consistently.
Our experience is that the subtrochanteric region of the proximal femur is relatively linear, and that a best-fit line corresponding to the axis of this segment of bone is compared with the functional neck axis defined by Yoshioka and Cooke21 (Fig. 28.3). We define a true lateral of the hip as the view when these two lines appear to be parallel on a single fluoroscopic image (Fig. 28.4). Often the functional neck axis is translated anterior to the subtrochanteric best-fit line when parallelism between the lines is established. Currently, the clinical significance of femoral rotational malalignment and whether a threshold value exists when functional outcome becomes compromised is unknown.

The establishment of safe and reproducible entry portals for nailing requires a detailed understanding of the osteology of the proximal femur and its corresponding imaging.
Piriformis entry portal nailing should begin about halfway down the piriformis fossa on the lateral image and about 5 to 6 mm from the top of the neck of the femur on the anteroposterior (AP) image (Fig. 28.5a). This starting point is anatomically aligned with the medullary canal. If you are too anterior, a neck fracture can occur,27 and if you are too posterior you run the risk of reaming out the back of the proximal femur.

With most trochanteric nails, the trochanteric entry portal nailing should begin at the tip of the trochanter on the AP image and nearly central in the neck on a true lateral of the hip (Fig. 28.5b). The starting guide pin should be aimed at the central portion of the medullary canal just below the lesser trochanter on the AP and lateral image.
Formal open reduction and internal fixation of the femoral shaft requires some knowledge of the surrounding soft tissues. The thigh is enveloped by a complex fascial structure called the fascia lata. The fascia lata thickens laterally to form the iliotibial band. The medial and lateral intermuscular septa extend from the deep surface of the fascia lata to the linea aspera of the femur, separating the thigh into anterior and posterior compartments. Prior to joining the fascia lata, the medial intermuscular septum splits to surround the sartorius muscle, and in this region contributes to the formation of the adductor canal in the middle aspect of the medial thigh. Although no discrete fascial structure subdivides the posterior compartment, the anteromedial portion is typically referred to as the medial compartment, given the common innervation and function of the muscles in this region. The anterior compartment contains the quadriceps muscles, which are innervated by the femoral nerve. The medial compartment contains the adductor muscles, which are innervated by the obturator nerve. The posterior compartment contains the hamstring muscles, which are innervated by branches of the sciatic nerve.
The femoral artery enters the thigh as the continuation of the external iliac artery as it emerges from below the inguinal ligament. Shortly thereafter it divides into superficial and deep branches as it exits the femoral triangle. The superficial branch enters the adductor canal anterior to the adductor longus muscle on the medial side of the thigh and eventually enters the posterior compartment through the adductor hiatus becoming the popliteal artery. The deep branch travels down the thigh more posteriorly between the adductor longus and magnus muscles. It gives rise to four perforating vessels that pierce the tendinous insertion of the adductor magnus muscle on the medial side of the femur, travel posterior to the bone, and enter the anterior compartment of the thigh through the lateral intermuscular septum.28 These perforating branches must be identified and ligated during a lateral approach to the femur. Femoral plating is usually done through a lateral approach. There are two options for exposure: longitudinal division of the vastus lateralis muscle, or elevation of the intact vastus lateralis off of the intermuscular septum and then the femur. The latter approach is associated with less muscle damage and the ability to directly visualize the perforating arteries. However, in obese or well-muscled individuals, exposure may be somewhat limited by soft tissue mass.
Surgical Technique
External Fixation
External fixation of a femoral shaft fracture is a damage-control procedure typically performed when a polytrauma patient is under-resuscitated or has a significant head injury, a very contaminated open soft tissue envelope, an associated ischemic vascular injury, or other surgical injuries requiring concurrent operating room teams.29,30 One of the key features of external fixation is the speed with which it can be placed. It should take approximately 15 to 20 minutes to apply a four-pin fixator to the femoral shaft and gain enough stability to control the limb.
A keen understanding of the relevant anatomy of the hip, thigh, and knee and quality radiographs of the entire femur are required prior to any surgical intervention. Radiographs of the femoral neck region (an internal rotation view is preferred in order to evaluate the femoral neck), the entire femoral shaft, and the knee joint are needed to rule out associated skeletal injuries. The fracture level should be identified and measured as it relates to key landmarks about the femur (i.e., the lateral epicondyle and the greater trochanter). This will assist the surgeon in identifying the level of the fracture by simple palpable landmarks. This is extremely important and facilitates the application of an external fixator when a C-arm is not available (as in the intensive care unit setting).
The patient should ideally be placed on a radiolucent table. The entire limb should be prepped and draped in a sterile fashion, including the hip joint and lateral crest of the ilium. Pins should be placed independently, with two pins close to the fracture and two pins distant from the fracture (Fig. 28.6). The first pin can usually be placed a few fingerbreadths below the tip of the trochanter, which should put it at the level of the lesser trochanter. The placement of the next pin is based on the location of the fracture; the pin is placed as close to the fracture as possible in the proximal fragment. The third pin is placed just below the fracture, and the last pin is placed at least two finger-breadths above the lateral epicondyle. An attempt should be made to place the two pins in each main fragment collinearly, although it is not absolutely mandatory. The pin is usually a 200 × 5 mm Schanz pin to allow for a double-stacked frame laterally (if needed). Larger pins (250 to 300 mm × 5 mm) may be needed for obese patients. The pins are ideally placed slightly anterolateral through percutaneous stab wounds in order to minimize soft tissue injury, tethering of the muscles, and risk to neurovascular structures during insertion.

The fascia is incised sharply, blunt dissection is carried out down to the level of the femur, and the cortex is palpated. The femur is predrilled with a 3.5-mm drill bit using a drill guide. The pins are then placed bicortically. Caution should be exercised when placing the pins to avoid inserting them too deep. Typically, increased resistance can be felt as the pin engages the far cortex if it is inserted very slowly with a power driver or by hand. A bar is then connected to both pins in each main fragment, effectively giving the surgeon an external handle on that fracture segment. Fracture reduction can then be performed using a combination of longitudinal traction and translation of the fragments in the appropriate plane.
If the two bars were strategically placed and they overlap following the reduction, they can be connected with a bar-to-bar type clamp. If the two bars do not overlap they can be connected using an additional bar. A second bar (a so-called double stack) may be added to strengthen the construct. If the frame is for temporary use only (which is frequently the case), a single-stack frame should be adequate and is less expensive. However, carbon fiber or steel bars smaller than 11 mm should be double stacked.
The skin around the pins should be released with a small incision if there is skin tenting. The pins are wrapped with sterile gauze to help with bleeding and drainage at the pin–skin interface. Range of motion of the hip and knee is allowed and encouraged as tolerated. Soft tissue irritation is common, and pin-site drainage may increase with activity and knee motion. Knee motion problems are one of the more significant disadvantages associated with the definitive management of femoral shaft fractures with external fixation.
Plate Fixation
There are two techniques for plate fixation of femoral shaft fractures: compression plating and bridge plating. Compression plating of fractures is most appropriate for simple fracture patterns, including spiral fractures, short oblique fractures, and transverse fractures. The more comminution that is present, the more difficult it is to plate the femur with compression techniques. For plating a comminuted fracture, bridge plating is the most useful and desirable technique.
Indications for femoral plating include a large associated open wound, and patients with significant head or chest injury. In the latter circumstance, treatment with intramedullary nail fixation could cause further injury to these organ systems.29 Complex combined femoral neck and shaft fractures, femoral shaft and distal intercondylar femur fractures, or periprosthetic femur fractures are also relative indications for plate fixation.31 Plates are ideally placed anteriorly and laterally to decrease tensile forces. Unfortunately, plating has a significant mechanical disadvantage compared with intramedullary nailing because it is off-axis to the mechanical load. When compression plating is applied, a 4.5-mm plate with a minimum of eight cortices of screw fixation above and below the fracture has traditionally been recommended. Newer plating techniques incorporate longer plates and fewer screws. As a general rule, no fewer than three screws should be used on each side of the fracture, and two or three empty holes on each side of the fracture will ensure an appropriate plate length. Early outcomes with these newer techniques look promising, but the ideal number of screws necessary remains elusive. When possible, the surgeon should use “balanced fixation”—an equal number of screws and plate holes on each side of the fracture.
Technique: Compression Plating
Patients are placed supine on a radiolucent table. The entire limb is prepped and draped to include the hip and the ilium. A long lateral incision is made centered over the fracture (Fig. 28.7). The fascia lata is incised longitudinally, anterior to the lateral intermuscular septum. Surgical dissection requires the vastus lateralis muscle to be elevated off of the lateral intermuscular septum (Fig. 28.8). Bleeding from perforating arteries is common and must be controlled. An alternative approach would be to plate the femur through the traumatic open wound, when present. Two principles to plating through traumatic wounds must but followed: first, the wound must be surgically clean, and second, care should be taken to avoid any further injury to the muscle envelope.


Reduction of the fracture is performed directly with pointed reduction clamps, if the fracture configuration permits. Alternatively, one end of the plate is affixed to the femur with one or two screws. Then, the femur is brought to the other end of the plate after controlling for length and rotation. Use of serrated jaw clamps (lobster claw) are discouraged, as they impart more soft tissue damage. Careful application of a plate-holding clamp may be needed but should be used with caution so as to avoid further injury to the bone and its vascularity. If an oblique or spiral fracture pattern is present, lag screws can be used to compress the fracture, and a large-fragment broad 4.5-mm lateral plate can be used in a neutralization mode. If the fracture is not amenable to lag-screw placement (such as a transverse fracture), compression can be applied through the plate with eccentrically placed screws, an articulated tensioning device, or a push-pull screw and Verbrugge clamp. Postoperative drains are recommended to prevent hematoma under the quadriceps. Early motion of the knee and hip are desired, and a continuous passive motion machine can be very helpful. Isometric quadriceps exercises and restricted weight bearing for 8 to 10 weeks are also recommended.
Technique: Bridge Plating
In more comminuted fractures where lag-screw fixation is precluded, bridge plating should be considered. The plate should be long enough to span the fracture and allow for three or four bicortical screws proximally and distally, as well as two or three empty holes proximally and distally. The plate is applied to the proximal fragment, aligned parallel to the bone, and secured with two 4.5-mm screws. Reduction of the fracture is usually performed indirectly in a closed fashion. This closed reduction may be accomplished through manual or skeletal traction on the leg, through the use of a provisional external fixator, or through the use of a femoral distractor. In open fractures, some direct manipulation of fracture fragments is possible but should be minimized to avoid further damage to bone vascularity. Length, axial alignment, and rotational alignment are controlled. Comparison radiographs of the opposite limb are sometimes necessary to confirm an acceptable reduction, especially regarding length and rotational alignment. (See Chapter 5 for details regarding the assessment of alignment, as well as Figs. 28.19, 28.20, 28.21, and 28.22 later in this chapter.) Once the limb and comminuted fracture are aligned appropriately, the plate is secured to the distal fragment with a plate-holding clamp. Care must be taken to make sure the plate is anterior enough to account for the anterior longitudinal femoral bow. If the fracture remains shortened, a push-pull screw with a lamina spreader or the compressor/distractor (articulating tensioning device) is then used to obtain the appropriate length. Two 4.5-mm screws are then placed in the distal fragment and the clamp is removed.
Generous use of C-arm fluoroscopy is needed to help confirm adequate alignment and rotation of the fracture. A few of the remaining screw holes are then filled with bicortical 4.5-mm screws. The soft tissue envelope is then closed over the plate with suction drainage placed deep to the fascia lata. Bone graft can be applied acutely if the fracture envelope is surgically opened, there is no concern of infection, and significant bone displacement is encountered. However, this would be unusual. In general, bone grafts are performed 8 to 12 weeks after the acute trauma, if needed. In open fractures, antibiotic-impregnated beads can be used in hopes of eradicating any potential infection that may be present.
Postoperative rehabilitation begins early with range of motion of the hip and knee. Both can be accomplished with the use of a continuous passive motion machine (CPM). The limb is kept touch-down weight bearing, and isometric quadriceps muscle strengthening is encouraged. Protected weight bearing is continued until bridging callus is seen (usually 12 to 14 weeks in closed fractures, and potentially longer in open fractures). When callus formation is present, weight bearing can be slowly advanced to stimulate further healing.
Technique: Percutaneous Bridge Plating
Bridge plating can also be performed using a percutaneous submuscular technique. Similar to traditional bridge plating, fractures amenable to this technique are predominantly comminuted mid-diaphyseal fractures in patients who cannot undergo intramedullary fixation. The patient′s limb is prepped and draped on a radiolucent table to enable control of the entire limb from the iliac crest to the foot. A small bump is placed under the ipsilateral sacroiliac joint to elevate the greater trochanter and improve access to the proximal lateral thigh. It is important to remember the impact of the bump when reducing the fracture and establishing the rotational alignment of the lower limb. The bump will elevate the ipsilateral hemipelvis and internally rotate the femoral neck. If the distal fracture segment is not internally rotated, an equal amount of relative retro-version may be introduced.
The limb is placed over a radiolucent triangle to facilitate lateral imaging. Longitudinal traction is applied to the limb by placing a thin wire through the proximal tibia or distal femur and connecting it to a tensioning-type traction bow. Fifteen to 20 pounds of weight are connected to the traction bow with a sterile rope that is hung over a bolster connected to the end of the operating table. Typically, this amount of weight in the presence of complete muscle relaxation will restore the limb length close to normal. Alternatively, a femoral distractor can also be utilized. If there is significant comminution, it may be helpful to obtain a leg-length measurement radiograph (or CT) of the opposite limb prior to surgery.
Our preference is to obtain this measurement intraoperatively using fluoroscopy prior to the start of the procedure. Measurement from the tip of the trochanter to the knee joint line using a radiopaque ruler is a good and reproducible means of assessing limb length. The length of the contralateral uninjured femur is measured prior to prepping and draping and recorded so that it can be re-created on the injured side. Positioning the contralateral limb in an identical position to that used during the surgical procedure while obtaining the measurement will minimize measurement error. This limb position can be obtained by placing the radiolucent triangle (prior to unwrapping the sterile cover) under the contralateral knee and placing the hip bump on the contralateral side. It is also important to note the position and tilt of the C-arm so that it can be reproduced intraoperatively. It has been our experience that if this level of diligence is not adhered to, there can be significant error introduced. Once limb length has been grossly reestablished, a large-fragment, broad, 4.5-mm plate can be selected to span from the vastus ridge to the epicondylar flare. Slight contouring of the plate is necessary to accommodate the metaphyseal flares and the anterior femoral bow, and can be performed with a table-top bender.
Two small incisions are made through the fascia lata laterally at the level of the epicondyle as well as over the vastus ridge (Fig. 28.9a). The plate is then inserted through the distal incision and slid submuscularly in a retrograde fashion until it is identified in the proximal wound. A bicortical screw is inserted at the level of the lesser trochanter, securing the plate. At this point manipulation of the proximal fragment is accomplished indirectly with traction, direct pressure, and strategically placed bumps, and occasionally with the use of percutaneous Schanz pins (5-mm manipulation aids) or ball-spike pushers (usually placed anteriorly to avoid interfering with plate placement laterally).

Once the proximal fragment is aligned with the plate, a second screw is applied percutaneously with the use of C-arm guidance (preferably close to the fracture). At this point, with the plate secured with two screws in the proximal fragment, the distal fragment is then manipulated into a reduced position with the use of bumps, traction, percutaneous Schanz pins, or ball-spiked pushers (Fig. 28.9b). Care should be taken to ensure appropriate rotation and length at this point. A third bicortical screw is then applied percutaneously through the plate, securing the plate to the bone. Once this third screw is placed, the length and rotation of the limb is established. A fourth screw is applied through the plate in the epicondylar region (Fig. 28.9c). Length and rotational alignment are reassessed, and supplemental screw fixation is applied percutaneously for a total of three or four screws proximally and distally.
The most difficult factor to confirm is rotational alignment, so scrutiny is encouraged. A reliable and reproducible technique to document and best approximate correct rotational alignment is to confirm that normal hip anteversion has been reestablished. A fluoroscopic true lateral view of the proximal femur aligning the neck with the shaft compared to a true lateral of the knee (without moving the extremity) will approximate anteversion. Every attempt should be made to match this measurement to preoperative values obtained of the opposite intact femur (see previous discussion on surgical anatomy).
At this point the patient′s wounds are irrigated and closed, the surgical drapes are removed, and range of motion of the hip and knee is performed. Rotational alignment and length can be compared clinically to the opposite limb at this time. Generally, abundant callus formation is usually seen with submuscular plating because the undisturbed muscular envelope helps lead to early periosteal callus formation. Weight bearing is still restricted for a total of 12 to 14 weeks to allow bridging callus to organize and mature. Hip and knee motion, as well as gentle strengthening, is encouraged during the early postoperative period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree