Femoroacetabular impingement (FAI) is a common cause of early-onset osteoarthritis of the hip. It can be caused by morphologic abnormalities involving the proximal femur or acetabulum, leading to abnormal abutment of the femoral head-neck against the acetabular rim. This repetitive trauma causes mechanical wear of the labrum and articular cartilage, leading to osteoarthritis of the hip. Magnetic resonance imaging is an accurate noninvasive imaging modality that can detect acetabular labral lesions and adjacent cartilage damage, and is able to detect underlying subtle anatomic variations of the femoral head-neck junction and acetabulum associated with FAI.
Key Points
- •
Femoroacetabular impingement (FAI) is a common cause of osteoarthritis of the hip in young adults.
- •
Impingement can be due to femoral abnormalities (cam impingement) or acetabular abnormalities (pincer impingement), or a combination of both (mixed type).
- •
FAI occurs as a result of abnormal contact between the proximal femur and acetabular rim, causing degeneration and avulsion of the acetabular labrum and cartilage damage.
- •
Early diagnosis of FAI is important for awareness, to initiate appropriate therapy and to delay the onset of osteoarthritis.
- •
The role of imaging in FAI is to make/confirm the diagnosis of FAI; depict and quantify morphologic osseous abnormalities of the femoral head and acetabular rim; define the exact location, extent, and severity of cartilage and labral damage; and to exclude advanced osteoarthritis and other diagnoses.
Introduction
Femoroacetabular impingement (FAI) is increasingly recognized as a pathomechanical process that can lead to hip pain and osteoarthritis in young adults. FAI occurs as a result of abnormal contact between the proximal femur and acetabular rim caused by morphologic abnormalities affecting the femoral head-neck junction or the acetabulum. In most cases a combination of femoral and acetabular abnormalities is identified. In addition, hypermobility of the hip can lead to FAI even in the setting of only minor osseous abnormalities, and reduced femoral antetorsion, impairing internal rotation, has recently been described as a cause of FAI. Repetitive microtrauma from impingement of the femoral head against the acetabulum causes degeneration and avulsion/tearing of the acetabular labrum, as well as progressive damage to the adjacent articular cartilage, leading to osteoarthritis of the hip. Through the development of hip arthroscopy, FAI can now be better treated, with fewer complications and shorter recovery time. Early diagnosis of FAI, before significant cartilage loss is evident, is therefore of paramount importance in initiating appropriate therapy and thereby reducing or delaying the onset of osteoarthritis. Unfortunately, the diagnostic accuracy of clinical tests for diagnosing FAI has been found to be too low to provide a conclusive recommendation. Therefore, imaging plays a crucial role in identifying morphologic abnormalities associated with FAI, and has become an important predictor of outcome and surgical success in patients with FAI.
Introduction
Femoroacetabular impingement (FAI) is increasingly recognized as a pathomechanical process that can lead to hip pain and osteoarthritis in young adults. FAI occurs as a result of abnormal contact between the proximal femur and acetabular rim caused by morphologic abnormalities affecting the femoral head-neck junction or the acetabulum. In most cases a combination of femoral and acetabular abnormalities is identified. In addition, hypermobility of the hip can lead to FAI even in the setting of only minor osseous abnormalities, and reduced femoral antetorsion, impairing internal rotation, has recently been described as a cause of FAI. Repetitive microtrauma from impingement of the femoral head against the acetabulum causes degeneration and avulsion/tearing of the acetabular labrum, as well as progressive damage to the adjacent articular cartilage, leading to osteoarthritis of the hip. Through the development of hip arthroscopy, FAI can now be better treated, with fewer complications and shorter recovery time. Early diagnosis of FAI, before significant cartilage loss is evident, is therefore of paramount importance in initiating appropriate therapy and thereby reducing or delaying the onset of osteoarthritis. Unfortunately, the diagnostic accuracy of clinical tests for diagnosing FAI has been found to be too low to provide a conclusive recommendation. Therefore, imaging plays a crucial role in identifying morphologic abnormalities associated with FAI, and has become an important predictor of outcome and surgical success in patients with FAI.
Clinical symptoms
Patients with FAI are usually young and physically active, and present with slow or more acute onset of anterior hip or groin pain and pain with hip rotation, particularly flexion and internal rotation. The prevalence of FAI is estimated to be between 10% and 15%. Sports activities such as soccer, football, kickboxing, hockey, or volleyball, which require hip flexion with variable torque or axial loading, may aggravate symptoms and are all associated with FAI. The pain in FAI often occurs after mild trauma or minor repetitive sports-related trauma, or occasionally without specific preceding trauma. Pain resulting from FAI has been described as being worse when significant stress is placed on the hip, when climbing stairs, or after prolonged periods of sitting. Patients with FAI and acetabular labral avulsion may report mechanical symptoms such as painful clicking or locking. The pain can also be located over the trochanters or be referred to the knee. Clinical and imaging review for potential referred pain from greater trochanteric enthesopathy, with gluteus minimus and medius tendon insertional partial-thickness or full-thickness tears, and of the lumbar spine for radiculopathy associated with disc hernia, may be required. Morphologic FAI abnormalities are often bilateral, but patients frequently present with unilateral symptoms. During physical examination, patients typically present with restricted internal rotation in hip flexion. Multiple clinical tests to diagnose FAI have been described. For example, the impingement sign (pain with flexion-internal rotation), the anterior hip impingement test (pain with flexion-adduction-internal rotation), or the FABER test (pain/decreased range of motion with Flexion and ABduction-External Rotation) are commonly positive in cam-type FAI, while posterior impingement tests with pain during forced external rotation in maximal extension can be positive in pincer-type FAI. However, these tests often have a low diagnostic accuracy and there can be overlap with other entities. Clinical experience is also influential ( Box 1 ).
- •
Young active individuals with increasing intensity of anterior hip and groin pain
- •
Activity-dependent pain
- •
Pain with flexion-internal rotation, climbing stairs, prolonged sitting
- •
Restricted range of hip motion compared with contralateral side, and/or compared with known clinical range of hip motion
- •
Painful clicking, locking
- •
Positive impingement tests
Etiology of femoroacetabular impingement
Hip impingement has been described after total hip arthroplasty in patients with abnormal hip anatomy, such as developmental hip dysplasia (DDH), slipped capital femoral epiphysis (SCFE), Legg-Calve-Perthes disease, or posttraumatic deformity whereby there is a mismatch between the femoral head-neck junction and the acetabulum.
A conceptual mechanism for the etiology of FAI and features associated with FAI has been described by Ganz and colleagues. This conceptual discussion allowed for some subdivision of potential causes of osteoarthritis instead of a general indiscriminant grouping of all hip joint forms being associated with “idiopathic osteoarthritis.” The etiology of FAI in patients without preexisting hip disease with subtle morphologic anatomic variations or abnormalities of the femoral head-neck junction or acetabulum continues to evolve. An osseous bony excrescence or “bony bump” at the femoral head-neck junction (cam deformity) may be the result of a subclinical SCFE during adolescence in some cases. Abnormal lateral extension of the physeal scar ( Fig. 1 ) caused by delayed separation of the common femoral head and greater trochanteric physis, or eccentric closure of the femoral head epiphysis, suggests an epiphyseal growth abnormality as the underlying cause for the decreased femoral head-neck junction. Congenitally reduced femoral antetorsion/anteversion can also impair internal rotation of the hip, leading to FAI. Genetic factors in the etiology of FAI have been proposed in a sibling study, which demonstrated an increased risk of siblings with FAI to have cam or pincer deformities. Putting a name to the impingement mechanism in young people allowed for potential treatment (eg, offset surgery and arthroscopic offset interventions) and being able to continue with sports and activities, instead of complete hip replacements at a young age or cessation of sports activities.
However, not all individuals with abnormal femoral and acetabular morphology develop symptoms, and morphologic findings of FAI-like appearances have been reported in asymptomatic subjects. These findings support the notion that additional factors, such as activity type and especially intensity of sporting or other activity, and vulnerability of the labrum and articular cartilage to injury, are important factors in determining whether the abnormal morphology will potentially result in symptoms.
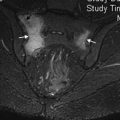
In addition, in a study of asymptomatic male Swiss army recruits, magnetic resonance imaging (MRI) findings suggestive of cam impingement were seen in 24% of asymptomatic subjects, and the prevalence increased with decreasing internal rotation to 48%. In the same cohort, MRI findings of cam-type FAI were associated with labral lesions and cartilage thinning, which are precursors of osteoarthritis. This demonstrates that in so-called asymptomatic subjects, restriction in range of hip motion and morphologic MRI abnormalities of labral and cartilage damage can be evident ( Box 2 ).
- •
Subclinical SCFE
- •
Growth abnormality of capital physis
- •
Growth variation of acetabulum
- •
Decreased femoral antetorsion
- •
Genetic factors
- •
Activity type and intensity
Pathogenesis of femoroacetabular impingement
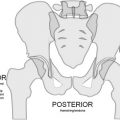
The normal anatomy of the hip joint allows for a wide range of motion. The morphologic abnormalities of the femoral head or acetabular rim that predispose a patient to FAI result in decreased joint clearance between the femoral head and acetabulum. In cam-type FAI, mechanical impingement of the femoral neck against the acetabulum and labrum occurs during terminal motion of the hip, leading to “outside-in” abrasions of the articular cartilage and damage to the adjacent labrum. Linear impact between a local (acetabular retroversion) or general (coxa profunda/protrusio) overcoverage of the acetabulum and a normal femoral-head morphology leads to pincer-type FAI, which first leads to acetabular damage ( Fig. 2 ). Reduced femoral antetorsion or anteversion can also impair internal rotation of the hip, leading to decreased joint clearance during flexion–internal rotation ( Fig. 3 ). Reduced femoral antetorsion has been reported in patients with FAI in comparison with controls. The detection of subtle anatomic and alignment abnormalities of the femoral head-neck junction and acetabulum is important for surgical planning, because arthroscopic labral or chondral debridement alone addresses only the site of secondary damage attributable to FAI and does not alter the underlying cause. Lack of treating the underlying osseous abnormality can lead to progression of the early labral and chondral lesions to osteoarthritis.
Mechanisms of femoroacetabular impingement: cam and pincer impingement
Two types of FAI can be distinguished. Impingement can be due to femoral abnormalities (cam impingement) or acetabular abnormalities (pincer impingement); however, in the majority of cases a combination of both (mixed type) exists.
Cam impingement is caused by abutment of an aspherical femoral head against the acetabulum during hip motion. The cam deformity refers to an osseous excrescence at the femoral head-neck junction or the aspherical portion of the femoral head. Posterior placement of the femoral head on the femoral neck with inadequate anterior femoral head-neck offset results in abnormal contact and mechanical impingement between the femoral head and acetabular rim when the hip is flexed and/or internally rotated. This process causes abnormal forces to act on the acetabular cartilage and subchondral bone in the anterosuperior acetabular rim area, which leads to damage to the labrum and articular cartilage. Cam impingement is more frequently seen in young athletic males.
Pincer impingement is the result of abnormal contact between the acetabular rim and the femoral neck as a result of acetabular abnormalities, such as acetabular retroversion, coxa profunda, or protrusio acetabuli, leading to anterior overcoverage of the femoral head. Acetabular retroversion refers to a posteriorly oriented acetabulum whereby the anterior acetabular roof edge lies lateral to the posterior edge. Abutment of the femoral head against the acetabulum results in degeneration and avulsion of the labrum with ganglion formation or ossification of the acetabular rim, which then further deepens the acetabulum, leading to worsening of the overcoverage. Persistent anterior abutment of the femoral head against the acetabulum can result in chondral injury of the femoral head, in the “contre-coup” area of the posteroinferior acetabulum. Pincer impingement is more frequently seen in middle-aged women ( Box 3 ).
- •
Cam impingement
- ○
Decreased femoral head-neck offset/aspherical femoral head
- ○
Abnormal contact between femoral head-neck junction and acetabular rim
- ○
Early cartilage damage at the junction of labrum and cartilage (acetabular > femoral), late extensive labral tears
- ○
Young males
- ○
- •
Pincer impingement
- ○
Acetabular overcoverage due to acetabular retroversion, coxa profunda, protrusio acetabuli
- ○
Abnormal abutment between femoral head against acetabulum
- ○
Early labral tears, secondary small chondral lesions near the labral defect
- ○
Middle-aged women
- ○
- •
Mixed type
- ○
Most common
- ○
Imaging of femoroacetabular impingement
Role of Imaging in Femoroacetabular Impingement
The role of imaging in FAI is to make or confirm the diagnosis of FAI and to depict and quantify the morphologic osseous abnormalities of the femoral head-neck junction and acetabular rim. Imaging is also central in defining the exact location, extent, and severity of articular cartilage and labral damage, and in excluding advanced osteoarthritis, which has a poor surgical outcome, and other diagnoses such as DDH, avascular necrosis, or stress fractures ( Box 4 ).
- •
Make or confirm clinical diagnosis of FAI
- •
Depict morphologic abnormalities of femoral head-neck junction, acetabulum
- •
Define extent of cartilage and labral damage
- •
Exclude advanced osteoarthritis
- •
Exclude other lesions that can mimic FAI (eg, DDH, avascular necrosis, stress fracture)
Radiographic imaging
Radiographic evaluation in patients with FAI includes a true anteroposterior (AP) pelvic view and an axial cross-table view of the proximal femur. Alternatively, an elongated femoral neck view (Dunn view) obtained in 45° flexion, which depicts the anterior femoral head-neck junction, can be obtained. It is important to follow standardized techniques for patient positioning to decrease the likelihood of incorrect diagnosis ( Fig. 4 ). Acetabular retroversion should only be diagnosed on an AP view of the pelvis to ensure satisfactory pelvic position without rotation or pelvic tilt, which can falsely create or obscure acetabular retroversion. Radiographic findings of cam impingement include an osseous excrescence at the anterolateral femoral head (see Fig. 4 ) and reduced offset of the femoral head-neck junction ( Fig. 5 ).
Acetabular retroversion can be diagnosed on AP radiographs by the “crossover” or “figure-of-8” signs and the “posterior wall” sign. The crossover sign in acetabular retroversion is created by the anterior acetabular rim being more laterally located than the posterior aspect of the acetabulum. The anterior aspect of the acetabular rim is directed more horizontally and medially, thereby crossing over the more straight and vertical posterior aspect of the acetabular rim ( Fig. 6 ). Prominence of the ischial spine, whereby the ischial spine projects into the pelvic cavity on AP radiographs of the pelvis ( Fig. 7 ), has been described in pincer impingement and acetabular retroversion.
Findings that can be seen with both cam and pincer FAI include synovial herniation pits, also known as fibrocystic change, at the femoral head-neck junction ( Fig. 8 ), and os acetabuli/fragmentation of the acetabular rim ( Fig. 9 ). This finding remains contentious in some circles ( Box 5 ).
- •
Pistol-grip deformity, profunda femora
- •
Abnormal lateral physeal extension
- •
Osseous excrescence at anterolateral femoral head, decreased femoral head-neck offset
- •
Acetabular overcoverage, positive crossover, figure-of-8 sign
- •
Protrusio acetabuli
- •
Prominence of the ischial spine
- •
Synovial herniation pits/fibrocystic change
- •
Os acetabuli, fragmentation of acetabular rim
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree