Fig. 13.1
Image a: Digital examination of a fetus with intact membranes. Image b: Digital examination of a fetus with ruptured membranes, X = internal uterine orifice, Y = external uterine orifice
Transvaginal digital examination is the gold standard for obtaining information about fetal position and presentation. Traditionally, obstetricians have determined the fetal head position by palpation of the sagittal suture and the anterior and posterior fontanelles. The position of the tip of the presenting fetal scalp is estimated relative to an imaginary line that connects the ischial spines of the mother; this position indicates which operative intervention is required, a primary Cesarean section or an instrumental delivery. An instrumental delivery should only be considered or attempted when head engagement is considered to have occurred, that is, when the leading part of the fetal head is positioned at least at the level of the maternal ischial spine (= station 0) or lower. Clinical assessment may be hindered by significant elongation of the fetal head, due to molding (see Fig. 13.2) and/or formation of caput succedaneum [7] (see Fig. 13.3).
Fig. 13.2
Example of fetal head molding (midsagittal view)
Fig. 13.3
Example of caput succedaneum (midsagittal view)
The progress of labor can be followed, first, by the descent of the fetal head into the maternal pelvis, which can be palpated on the abdomen; second, the descent of the presenting part of the fetal head relative to the ischial spines, which can be defined in a vaginal examination; and third, the dilatation of the cervix. It is also crucial to take into account information regarding caput and molding of the fetal head, the thinning and dilation of the cervix in response to the presenting part, and the strength and duration of the contractions. Signs of obstructed labor include a pause (or even reversal) in cervical dilation, due to swelling of the edematous, poorly effaced cervix; the interrupted descent of the fetal head; and an irreducible head molding that is difficult to feel, due to the development of a large amount of caput. In the mother, there is exhaustion, pyrexia, tachycardia, and signs of dehydration. In multiparous women, frequent, strong contractions may overcome the obstruction, but this runs the risk of uterine rupture. In nulliparous women, the uterine contractions may decrease in strength and frequency, and a retraction ring (Bandl’s ring) may be formed.
13.2 Treatment Options: Vaginal Operative Delivery
In the past, an essential part of obstetric practice included knowledge of difficult vaginal operative techniques and the ability to perform difficult vaginal deliveries. Hence, the rate of operative vaginal deliveries declined; for example, in Germany, the rate declined to 5.50 % in 2008 from 6.9 % 10 years earlier [14]. Inevitably, this decline in the rate of deliveries by vaginal operative techniques (vacuum extraction or forceps) led to less effective training of obstetricians in terms of vaginal operative deliveries. In current practice, the low acceptance of risk and high medicolegal awareness have caused obstetricians to strive to avoid difficult vaginal deliveries (see Fig. 13.4); thus, the clinician’s skill resides mainly in precisely identifying the fetal head position and station to ensure that the appropriate technique is applied to enable a safe vaginal operative delivery without complications. Thus, they should know when forceps or ventouse should be applied and when a Cesarean section is warranted.


Fig. 13.4
Effect of wrong placement of ventouse and forceps – cephalohematoma and injury of plexus and skin
An unsuccessful operative vaginal delivery could have serious consequences for the fetus. A study by Towner et al. reported that the incidence of intracranial hemorrhage increased from 1/860 with vacuum delivery to 1/334 with Cesarean section after a failed operative vaginal delivery [15].
13.3 Cesarean Section
On the other hand, the rising rate of Cesarean section is an international concern. Currently, nearly one third of newborns are delivered by Cesarean section (in Germany 30.24 % in 2008) [16]. During the past decade, there was a 50 % increase in the Cesarean section rate, a significant decline in the rate of vaginal births after Cesarean section (28.3 % in 1996 to 8.5 % in 2006), and a 42 % reduction in vaginal operative deliveries [17]. The rates of repeat Cesarean birth following a previous Cesarean have risen commensurately, reaching 83 % in Australia [18] and nearly 90 % in the USA [19]. Repeat Cesarean currently account for 28 % of all births in the United Kingdom [20].
The increases in Cesarean section rates are explained as follows: (1) The increase in repeat Cesarean section rate correlates with the increase in primary Cesarean section rates; (2) the involvement of midwives has fallen to a low level; (3) the reduction in operative vaginal deliveries has led to reduced obstetrician experience; thus, they feel less confident in conducting operative procedures; and (4) the lack of effective training for obstetricians in vaginal operative deliveries has caused them to abandon difficult deliveries in favor of Cesarean sections. On the other hand, the increased use of electronic fetal monitoring has increased our awareness of fetal distress. Thus, despite an abnormal CTG and/or low pH at fetal blood sampling, the majority of babies are born in good condition.
Blackwell et al. [21] showed that an overestimation of ultrasound-derived estimated fetal weight (EFW) could influence the likelihood of a Cesarean delivery due to the predicted risk of labor arrest. Labor outcomes of women with EFW overestimations that were >15 % above the actual birth weights were compared with those that had accurate EFW estimations. Overestimation of EFW occurred in 9.5 % of cases (23/241). The rate of Cesarean delivery to predicted labor arrest was higher in cases with EFW overestimations than in cases with accurate EFW estimations (34.8 % vs. 13.3 %; P = 0.01) independent of induction durations. All Cesarean section in the overestimated EFW group were performed based on the predicted risk of labor arrest.
A multicenter study at 14 Australian maternity hospitals [22] investigated 2,345 women with a single prior Cesarean that were eligible to attempt a planned vaginal birth after Cesarean section (VBAC) at more than 37 weeks of gestation. The subjects were divided into two groups: one group with a planned VBAC, the other with a planned elective repeat Cesarean section. They found significantly more serious neonatal morbidity and major hemorrhage in the VBAC group than in the Cesarean section group. This led to the recommendation that a first Cesarean section should be avoided, unless there is a clear medical necessity.
A Cesarean delivery may lead to serious complications, particularly when the head is deep in the birth canal. The complications include major hemorrhage, greater risk of bladder trauma, and extension tears of the uterine angle, which can lead to a broad ligament hematoma [2]. In pregnancies that occur after a Cesarean section, abnormal placental implantation has become a common complication. The increase in primary Cesarean section rates has also led to an increased risk of uterine rupture and last, but not least, an increase in repeated Cesarean sections.
13.4 Assessment of Station and Position
In view of these risks, ultrasound studies have recently been conducted to improve assessments of fetal head position and station (see Fig. 13.5). These studies have shown that transperineal ultrasound might enable the objective quantification of the level of fetal head descent in the birth canal by measuring the distance between the outer bony limits of the fetal skull relative to either the maternal symphysis pubis or the skin surface of the perineum. In 2009, Yeo and Romero [23] reviewed sonographic evaluations performed in the second stage of labor to improve assessments of labor progression and outcome. Molina and Nikolaides also discussed this subject in 2010 [24]. Thus, the obstetrics field has focused on making the appropriate decision when there is failure to progress in either the first or second stage of labor.


Fig. 13.5
Determination of station and position by ultrasound
13.4.1 Position
It is crucial for the obstetrician to establish why progress has become arrested and exclude obstructed labor before augmenting contractions [25]. The risk factors for arrest of descent during the second stage of labor include nulliparity, birth weight >4 kg, epidural analgesia, hydramnios, hypertensive disorders, gestational diabetes, male fetus gender, premature rupture of maternal membranes, and induction of membranes [26]. Fetal malposition at full dilation increases the risk of a prolonged second stage of labor, and it increases the risk of maternal morbidity [27]. Therefore, it is essential to make a precise diagnosis of OP position during labor (see Fig. 13.6). Traditionally, obstetricians determine the fetal head position by palpation of the sagittal suture and the anterior and posterior fontanelles. The fetal head position and the exact degree of internal rotation in the second stage of labor is prerequisite knowledge for a safe vaginal instrumental delivery [28] (it assists in the optimum placement of the ventouse cup) and for selecting the location of delivery (in the theater vs. in the labor room) [15, 29, 30]. Errors in assessments of fetal head position may result in deflexed and asynclitic head attitudes, which may cause failure of a vacuum delivery.
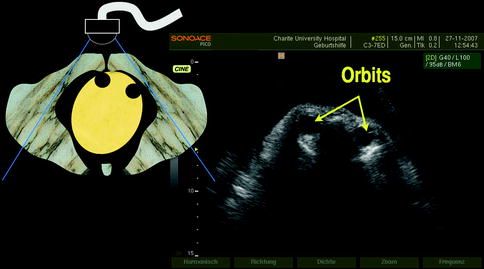
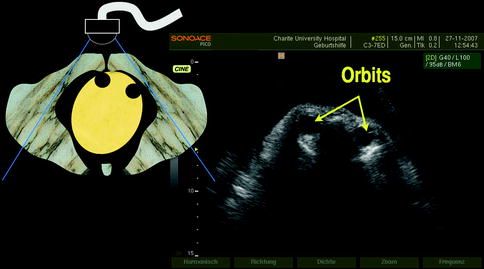
Fig. 13.6
Occiput posterior position. Demonstration of fetal orbits. Transabdominal ultrasound
Ultrasound to Determine Position
Several studies [31–35] in the last few years showed that precision and good reproducibility are lacking in the determination of fetal head position. Clinical examination alone is subjective, particularly in the presence of large caput succedaneum. Furthermore, extensive evidence has suggested that digital pelvic examination is not accurate for the determination of fetal head position during labor [36, 37]. In comparison, ultrasound can provide far more precise determinations of fetal head position and station. In all studies (see Table 13.1), large discrepancies were found between ultrasound and digital examinations, particularly during the first stage. Two studies of second stage fetal position [38, 39] compared ultrasound, digital examinations, and the actual position at delivery. They found a 70 % agreement between the digital exam and the actual position at birth, but the agreement between ultrasound and the actual position at birth was above 90 %. Note, that it is possible that some fetuses rotated between the time of assessment and birth, because all ultrasound errors occurred for patients in the +1 to +2 stations.
Table 13.1
Digital examinations versus ultrasound to diagnose OP position during the second stage of labor. In all studies, high rates of disagreement occurred between ultrasound and digital examinations—higher during the first than the second stage
N | % agreement with ultrasound (within 45°) | |
|---|---|---|
Souka et al. [31] | 133 | 66 |
Sherer et al. [36] | 102 | 47 |
Dupuis et al. [32] | 110 | 80 |
Akmal et al. [34] | 64 | 27 |
Clearly, noninvasive methods for detecting and correcting malpositions would reduce the need for medical and surgical interventions and improve outcomes for mother and baby. Sonographic assessment of the fetal head prior to delivery is frequently applied, most likely due to the ready accessibility to ultrasound equipment in outpatient clinics and delivery rooms. A study by Lieberman et al. [40] investigated how difficult it would be to interpret ultrasound images of fetal position, particularly for ordinary maternity practitioners (with less experience than a sonologist). They found that, among 4,054 ultrasonograms, 440 (10.8 %) were uninterpretable. The rates of failed identification reported for ultrasound were lower than those reported for digital examinations. The rates were higher early, compared to later, in the study period. Of note, “uninterpretable” images may cause less harm than “mistakenly interpreted” images, because the latter may lead to false certainty and inappropriate actions.
Sonographic techniques for determining fetal position include the abdominal approach, the vaginal approach, and three-dimensional (3D) ultrasound. Results from various studies revealed that accuracy was often improved with ultrasonic visualization, particularly when occiput anterior (OA) and OP positions could not be readily distinguished. The first determination of fetal head position by transabdominal ultrasound was published by Rayburn et al. in 1989 [41]. They differentiated between right OA and left OP positions, deflexed head, and asynclitism by defining the fetal cerebellum and orbits. According to that study, transabdominal ultrasound could explain an arrest of labor and allow a timely Cesarean delivery, or it could increase confidence in a forceps placement. Wong [42] investigated whether the accuracy of vacuum cup placement might be improved by intrapartum ultrasound assessment of the fetal head position during the second stage of labor. They found that the mean distance between the center of the chignon and the flexion point was 2.1 ± 1.3 cm in the group with both digital examination and ultrasound assessment and 2.8 ± 1.0 cm in the group with digital examination alone. The difference in mean distance between the two groups was statistically significant (P = 0.039). Thus, the accuracy of the vacuum cup placement was improved in the ultrasound group. There was no statistically significant difference in the two groups in terms of maternal and neonatal morbidities. There was one case of failed vacuum extraction in the no ultrasound group.
Asynclitism
Fetal head asynclitism is defined as a lateral flexion of the head. Two varieties of asynclitism are classically recognized. The anterior type is a posterior twisting of the head, with the sagittal suture close to the maternal sacrum; in this case, the anterior parietal bone is the leading part of fetal skull at vaginal examination. The posterior type is an anterior twisting of the head, with the sagittal suture close to the maternal pubis; in this case, the posterior parietal bone is the leading part of the skull at vaginal examination. Asynclitism, particularly the posterior type, is a common cause of prolonged or obstructed labor [43]. Diagnosis is traditionally based upon clinical findings in patients that experience a pause in fetal head descent during advanced first stage or second stage of labor.
Malvasi et al. [44] evaluated 150 women by transabdominal and transperineal ultrasound to detect asynclitic and deep transverse positions. They found that the digital examination was significantly less effective than ultrasound evaluation for the detection of either transverse position or asynclitism. The left transverse position and the anterior asynclitism were the most frequently observed. The authors described two new signs for diagnosing asynclitism: The “squint sign” and the “sunset of thalamus and cerebellum sign.” These signs facilitated the detection of both anterior and posterior asynclitisms (see Fig. 13.7a and b).
Fig. 13.7
Transabdominal intrapartum ultrasonography (US). (a) An occiput posterior left position and anterior asynclitism representing the squint sign with the orbit (orbit circumference). (b) A right transverse position, with the sagittal suture lies anteriorly, showing the right orbit
Transvaginal Ultrasound
As descent of the fetal head progresses, transabdominal sonography becomes difficult, due to shadowing by the maternal symphysis. Zahalka et al. examined the accuracy and time requirements for transvaginal scans (TVS) in the second stage of labor for determining fetal head position [45]. Fetal head position could be determined in all cases by TVS; in contrast, seven and nine cases could not be determined by digital vaginal examination and transabdominal ultrasound scans (TUS), respectively (P < 0.03; P < 0.008). Compared to TUS or TVS, the digital vaginal exam showed fetal head discrepancies of 60° or more in 13/60 (21.7 %) or 14/60 (23.3 %) cases, respectively, and a ≥90° discrepancy in 9/60 (15 %) and 12/60 (20 %) cases, respectively (P < 0.02 compared to both TUS and TVS). No significant differences in fetal head position were detected between TUS and TVS, when the examination was technically feasible. TVS was the most successful method of the three studied; it was most accurate for determining fetal head position in the second stage of labor, and it required the least time for performance. In conclusion, the authors postulated that TVS should be routinely performed in the labor room setting for the determination of fetal head position.
Assessing the position of the fetal occiput is difficult with transperineal ultrasound [38], because this method provides only a narrow anatomic section of the maternal sagittal plane. Consequently, it rarely allows visualization of the orbits or cervical spine, and a suprapubic scan may be necessary [46]. However, evaluation of fetal head rotation is also of value, as an angle <45° with respect to the anteroposterior plane of the maternal pelvis would suggest that the base of the skull is at or below the level of the ischial spines, which corresponds to the smallest diameter of the pelvis [7, 47]. When a fetal OP position can be identified and corrected manually, the mother and baby may be spared from instrumental or Cesarean delivery. Various techniques for digital or manual rotation are described in midwifery and obstetric textbooks. For digital rotation, the practitioner presses the fingertips against the fetal head and slightly lifts and rotates the head. For manual rotation, the whole head is inserted into the uterus or vagina, and the fetal head is grasped and rotated. These techniques are not widely used and require experience. They are considered safer than instrumental delivery by experienced proponents [48]. Sometimes, these procedures involve umbilical cord prolapse and fetal neck injuries, but no specific studies are available on the incidence of these outcomes. Reichman et al. [49] studied the efficacy of digital rotation for reducing persistent OP position; they included women at term, that had exhibited, in the second stage of delivery, babies engaged in an OP position. That trial was a before-and-after comparison of medically indicated, not prophylactic, rotations. Group 1 comprised 30 women that delivered in the first 6 months of the study period and did not undergo digital rotation. Group 2 comprised 31 women that delivered in the second 6 months of the study and, after receiving an ultrasound-confirmed OP diagnosis, underwent digital or manual rotation. Group 2 had a 77 % rate of spontaneous births, compared to 26 % in group 1. Group 2 women were more likely than group 1 women to deliver babies engaged in the OA position (93 % vs. 15 %) and less likely than group 1 women to have a Cesarean section (0 % vs. 23 %) or a vacuum-assisted birth (22 % vs. 50 %). These results suggested that digital rotation should be considered when managing the labor of a fetus in the OP position. The maneuver successfully rotated the fetus, and thus, it reduced the occurrence of Cesarean section, instrumental delivery, and other complications associated with persistent OP position.
Three-Dimensional Ultrasound
With transperineal ultrasound, one can simply rotate the transducer in the transverse plane to identify the midline of the fetal head, defined as the echogenic line interposed between the two cerebral hemispheres. This approach provides significant additional information, because a transverse view of the fetal head allows assessment of the angle between the fetal cerebral midline and the anteroposterior plane of the maternal pelvis [46]. It is nearly certain that, when the fetal head is directed upward and rotated <45°, the station is +3 cm or more. Three-dimensional transperineal ultrasound applied intrapartum allows clear discernment of the sutures and fontanelles: thus, the exact stage of internal rotation of the head can be determined in the second stage of labor [81]. Furthermore, 3D ultrasound can enable the determination of head asynclitism. In particular, a free cut within an ultrasound volume appears to be a valuable technique for displaying the head midline, despite extreme posterior flexion of the fetal head [50].
The ability to predict accurately, during the second stage of labor, whether the fetus will be in the OP position at birth is important, because it indicates whether a pregnancy will result in spontaneous vaginal delivery without complications or whether it will require an operative delivery (abdominal or assisted). A study by Blasi et al. [51] analyzed the predictability of fetal head position during the course of labor. They enrolled 100 women with singleton pregnancies during the first or second stage of labor and 84 were evaluated in the second stage of labor. The fetal head position and spine were evaluated by intrapartum transabdominal sonography. Women were followed up until delivery, and OP at birth was assessed. They found that, when the fetal head assumed an OA position during the second stage of labor, it was highly likely that the head would be in an anterior position at delivery. Conversely, when the head assumed the OP position during the second stage of labor, it was only 26 % (6/26) likely to be in the same position at delivery. They also found that the position of the spine during the second stage of labor could be used as a diagnostic sign in predicting the OP position at birth.
The goal of ultrasonography is not simply to predict the mode of delivery by fetal head position but to detect the actual position with a reliable, objective measure. A review by Verhoeven [52] showed that intrapartum sonographic assessment of fetal head position did not increase the predictability of Cesarean section. However, the full certain knowledge of position during labor may provide more time to consider therapeutic options and facilitate earlier implementation. In fact, digital examinations may do more harm than good; they may miss many fetuses in the OP position; thus, they may miss the opportunity to intervene with noninvasive corrective measures. Once diagnosed, triage can take place. Several years ago, attempts were undertaken to reduce the Cesarean section rate for dystocia [25]. However, first, a reliable method for routinely determining head position must be established; only then will it be possible to perform prospective, randomized studies to analyze the impact of those treatments on fetal head position.
13.4.2 Station
The traditional principle of applied obstetrics holds that a correct diagnosis relies upon the determination of the relationship between the fetal head and the maternal pelvis or the position of the tip of the presenting fetal scalp relative to an imaginary line connecting the ischial spines. This determination can indicate a normal, vaginal delivery, or alternatively, it can indicate which operative intervention is required (primary Cesarean section or instrumental delivery). According to international guidelines [7, 53, 54], instrumental delivery is attempted only when the head is considered to be engaged. The area above and below the maternal ischial spine is divided into fifths. As the presenting fetal part descends from the inlet toward the ischial spine, the stations are described as −5, −4, −3, −2, and −1; the 0 station is at the ischial spine level; then, the stations proceed to +1, +2, +3, +4, and +5. At station +5, the fetal presenting part is visible at the introitus [43]. Significant elongation of the fetal head due to molding and/or formation of caput succedaneum may hinder clinical assessment.
Over the last few years, studies have shown that digital estimations of head station during labor were imprecise and poorly reproducible. A study by Dupuis et al. [32] found that vaginal digital examinations of fetal head descent were unreliable, with errors in 50–80 % of examinations, depending on the true level of the head. However, they used a birth simulator, and the mannequin fetal head could not simulate molding or caput succedaneum; thus, the error rate is likely to be even higher in a clinical setting. Furthermore, a recent prospective study [55] performed with 508 women in term labor found very poor interobserver agreement in estimating fetal head station. In 446 women, the station could be estimated by both the researcher and the clinicians. However, in 131 women (29 %), the researcher and clinicians did not agree on engagement. The kappa statistic was 0.33 (95 % CI, 0.24–0.43). Thus, estimation of station by digital examination appeared to be imprecise and poorly reproducible.
Against this background, and in response to the uncertainty and lack of objectivity, recent studies have shown that transperineal ultrasound might provide an improved objective measure of fetal head progression in labor. Ultrasound scans of the fetal head in the maternal pelvis were systematically and prospectively evaluated. Based on those results, currently, intrapartal transperineal ultrasound is being intensively studied and evaluated as a new method for determining fetal head station, particularly in the second stage of labor.
Ultrasound to Determine Station
In the past few years, several sonographic approaches have been described for determining the station and rotation of the fetal head. These include linear measurements (distance between the fetal head and the maternal perineum) [56–59], subjective assessment of the fetal head direction [46, 60], and angular measurements [61–63].
The first sonographic attempt to assess engagement was published by a French group [64]. They measured the distance between the fetal head and the sacral tip based on echoes obtained in the A mode. A scale was established, and the ultrasound results were correlated to clinical findings. The authors stated that, when the distance from the fetal head to the sacral tip was ≤40 mm, the head was always engaged. In addition, they discussed whether the curved line of the pelvis might serve as an indication of a low station, appropriate for a low forceps approach, because, during the last period of the second stage of labor, the axis of the pelvis is no longer a straight line.
Twenty-six years later, Sherer and Abulafia [65] investigated the transabdominal approach to measure the station of the fetal head. They included 222 consecutive patients in labor that were >37 weeks’ gestation, with normal, singleton, cephalic-presenting fetuses, and with either ruptured or intact membranes. First, transvaginal digital examinations were performed; these were followed immediately by transverse suprapubic sonographic assessments performed by a single sonographer. The fetal head was considered engaged when, on transvaginal digital examination, the leading part of the fetal head was positioned at least at the maternal ischial spine (station 0) and when, on transverse suprapubic ultrasound, the fetal biparietal diameter was below the maternal pelvic inlet. Transvaginal digital examinations were consistent with ultrasound determinations with a raw percent agreement rate of 85.6 % (95 % confidence interval [CI], 80.8–90.3); kappa statistic = 69.5 % (95 % CI, 59.4–73.9; P < 0.001). This high rate of agreement between ultrasound determination and transvaginal digital assessment of fetal head engagement heralded the establishment of intrapartum transabdominal assessment for determining fetal head engagement.
Transperineal Ultrasound
Dietz and Lanzarone reintroduced the transperineal ultrasound approach in 2005. The group [66] performed transperineal ultrasound scans in 139 women in the first stage of labor. They quantified fetal head descent by measuring the minimum distance between the fetal head and a line positioned at a 90° angle from the central axis of the pubic symphysis in the midsagittal plane. They found that this measurement was reproducible and prognostic of the course of labor. Another study by the Dietz [58] group showed that head engagement measured by ultrasound, Bishop score, and maternal age were the strongest single predictors of delivery mode.
These investigations were followed by Henrich et al. [60], who were the first to use the transperineal approach to predict the success of vacuum extraction. The study included 20 women in labor. The group performed the transperineal ultrasound assessment while the woman was actively pushing, immediately prior to vacuum extraction, or at the time of the ventouse application. Fetal head descent was categorized into three stages, according to fetal head direction (defined as the direction, with respect to the infrapubic line, of a line drawn perpendicular to the widest diameter of the fetal head below the symphysis); the directions included head up, head down, and horizontal.
Recently, a simpler approach to fetal head direction quantification was suggested with the use of transperineal ultrasound [67]. The classical measurement described by Henrich was shown to be equivalent to the angle formed by the widest biparietal fetal head diameter and the symphysis pubis long axis. Increasing values of this angle signified progression of the fetal head, angles less than 90° were associated with a downward direction, angles of 90–120° corresponded to a horizontal direction, and angles >120° signified an upward direction of the fetal head.
13.5 Rotation
A group in Bologna, Italy [46], also used fetal head direction to investigate the ability of intrapartum transperineal sonography to diagnose station in the second stage of labor. They found that, on the sonogram, when the fetal head was directed downward, the station most frequently assessed clinically was ≤+1 cm from the ischial spines; when the direction was horizontal, the station was most frequently ≤+2 cm; and when the direction was upward, the station was usually ≥+3 cm. Failure to visualize the cerebral midline or a rotation ≥45° was associated with a station ≤+2 cm. Conversely, a rotation of <45° was associated with a station ≥+3 cm. The probability of a station ≥+3 cm was particularly high when an upward direction of the head was combined with a rotation <45°.
13.6 Distance Measurements
Another approach for determining station is to measure the head-to-perineum distance. Previously, this approach had only been performed before labor or in small pilot studies. Eggebø et al. [56




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree