Fibro-Adipose Vascular Anomaly (FAVA) is a recently identified type of vascular malformation predominantly affecting adolescent females. Comprising abnormal adipose and vascular components, FAVA is frequently misdiagnosed as other vascular anomalies. It primarily manifests with pain, functional impairment, and musculoskeletal symptoms, particularly in the lower extremities. Accurate diagnosis requires a combination of clinical, radiologic, and histopathologic evaluation, with MRI and ultrasound being the primary imaging tools. Management of FAVA is multidisciplinary and tailored to individual patients. Interventional radiology procedures, such as percutaneous cryoablation, sclerotherapy, and embolization, are effective in long term control of symptoms. Cryoablation is particularly successful in alleviating pain and improving function. Surgical resection is reserved for specific cases with extensive lesions involving joints or when there is severe muscle or joint dysfunction. Additionally, sirolimus, an mTOR inhibitor, has shown promise in symptom relief, although further research is needed to confirm its long-term efficacy. Early diagnosis and treatment are essential for improving the quality of life in FAVA patients. Advances in imaging and treatment strategies have enhanced the ability to manage this complex and rare condition effectively.
Introduction
Fibro-Adipose Vascular Anomaly (FAVA) was initially mislabeled as various other vascular anomalies, but was recently described as a unique intramuscular lesion affecting the extremities. This lesion is composed of an adipose component and a vascular malformation component (venous and lymphatic malformation). FAVA can be easily confused with other intramuscular lesions including venous malformations, arteriovenous malformations and PTEN-associated malformations amongst. FAVA remains a challenging diagnosis for the nonexperienced physician and its diagnosis is based on close clinical, radiologic and histopathologic correlation.
Clinical Presentation
In general, FAVA is most commonly seen in young females (3:1 female-to-male ratio), typically presenting between the ages of 10 and 20 years. Almost all patients present with pain and functional impairment as part of their symptoms. The pain associated with FAVA is multifactorial. Diffuse pain is typically related to the dense fibrous fatty changes within the muscle, which impair normal contractility and function. Focal pain may be attributable to the venous malformation component, due to thrombosis or phleboliths, or can be neurogenic in origin. The malformation involves the muscle, most commonly involving the lower extremities (80%-85%), particularly the calf muscles (gastrocnemius and soleus), resulting in localized swelling or soft tissue overgrowth. Less common it can present in other parts of the body (15%-20%) such as the forearm, arm, hand and trunk. Intra-articular extension has also been described. Due to the intramuscular location of FAVA lesions, musculoskeletal system related symptoms are most common and specific, for example, limited range of motion, contracture, and atrophy related to disuse of the affected muscles. Localized swelling and paresthesia can also be seen. The lesion is typically isolated to 1 muscle, with rare involvement of additional muscles, typically in the same limb. Joint or muscular contractures include ankle equinus, knee extension and hip adduction contractures. About 20% of patients with FAVA may have some form of skin involvement. Cutaneous lymphatic vesicles are the most common skin abnormality, but capillary malformation, dilated superficial veins or hypopigmentation of the skin can also be seen.
Imaging Features
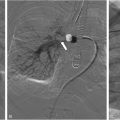
Ultrasound and Magnetic Resonance Imaging (MRI) are the primary imaging modalities in diagnosis of FAVA. The utility of plain radiographs and computerized topography (CT) is limited though these may help elicit additional findings, such as the presence of calcifications in associated venous malformations and bony deformities.
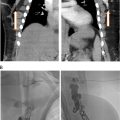
MRI
On MRI, a predominantly intramuscular malformation is seen that demonstrates heterogeneous high signal intensity on T2 weighted sequences ( Figs. 1 a and 2 a). On T1 weighted images, the lesion is predominantly of low signal with infiltrating high signal, due to variable amounts of fibrosis and fat content ( Fig. 1 b). The lesions demonstrate heterogeneous enhancement after gadolinium administration ( Fig. 1C ). MRI reveals the full extent of the lesion and helps differentiate focal, infiltrative and diffuse involvement. Phleboliths are seen as a focal areas of low signal intensity on T2 weighted sequences. On occasion, flow voids related to presence of vascular channels may also be seen.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree