FIBROUS DYSPLASIA AND OTHER FIBRO-OSSEOUS LESIONS OF THE CRANIOFACIAL SKELETON
KEY POINTS
- Computed tomography is the primary tool for the evaluation of craniofacial skeleton osteodystrophies such as fibrous dysplasia and other fibro-osseous lesions.
- Magnetic resonance imaging may be used occasionally for problem solving.
- Magnetic resonance imaging findings may go unnoticed or be initially confusing in these disease states and mistaken for much more serious pathologic changes.
- Imaging sometimes does not specifically explain a functional deficit caused by these fibro-osseous conditions.
- Fibro-osseous lesions can cause complications that can have more consequences than the disease itself or add to the morbidity of that disease.
These fibro-osseous conditions that effect bones throughout the body frequently express themselves in isolated form in the craniofacial skeleton. The craniofacial expression may be part of a condition that involves more than one segment of the skull base and/or facial bones including the temporal bones (Chapter 119). The most common form of fibro-osseous disease is fibrous dysplasia. The craniofacial bone involvement may also be part of a systemic process. These systemic processes may be generally categorized as developmental/dysplastic, metabolic, dystrophic, and reactive. The fibro-osseous lesions are in the first category.
Patients may present with a variety of complaints, physical findings, and functional deficits that are common in other pathologic conditions of the craniofacial skeleton. Fibrous dysplasia and other fibro-osseous lesions are discussed here, in summary, with regard to their specific craniofacial manifestations. Fibrous dysplasia and other fibro-osseous conditions are discussed more completely with regard to their pathophysiology, computed tomography (CT) and magnetic resonance (MR) appearance, and treatment in Chapter 40.
All of these conditions can obstruct sinus ostia and impede normal mucociliary drainage pathways (Fig. 91.1). The sinus obstruction can lead to a mucocele that may be very difficult to differentiate from the primary dysplastic or neoplastic process. In fact, trapped mucosa within areas of abnormal bone can at times produce very bizarre mucocele patterns and infections.
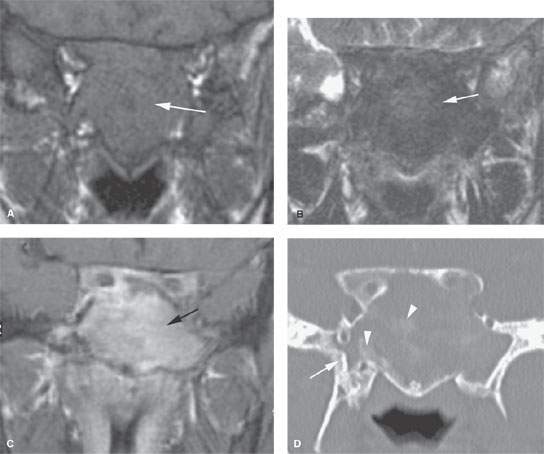
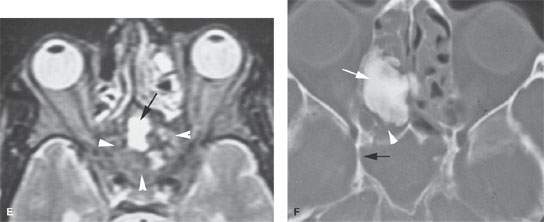
FIGURE 91.1. A–E: Computed tomography (CT) and magnetic resonance (MR) studies of a patient with fibrous dysplasia of the sphenoid bone. In (A), the non–contrast-enhanced T1-weighted (T1W) image shows a nondescript mass isointense to brain within the sphenoid bone possibly with an expansile nature. In (B), the T2-weighted (T2W) images show this to be homogeneously dark (arrow); a finding that suggests lack of mobile protons that is suggestive of a lesion with a significant fibrous component and/or calcification. In (C), the contrast-enhanced T1W image shows the abnormality to be diffusely enhancing, a finding fairly characteristic of fibrous dysplasia (arrow). In (D), CT study of the same patient shows that the lesion is within the sphenoid bone and as a predominately noncalcified matrix. This combined with the MR study suggests a diffuse fibrous matrix. There are focal areas of calcification of the matrix in a pattern most suggestive of fibrous dysplasia (arrowheads) and an area of bony thickening in the base of the pterygoid plates that suggests calcified fibrous matrix. In (E), the T2W image shows that the matrix of the lesion is mostly marrow equivalent or darker (arrowheads), although there are areas of bright signal intensity (black arrow). The bright signal intensity parallels that of mucosal thickening in the fluid, the vitreous body and cerebrospinal fluid suggest the presence of mobile protons in this portion of the lesion. Such findings can be due to the trapped sinus mucosa, a developing secondary mucocele, or nonfibrous matrix within the fibrous dysplasia. (NOTE: This case illustrates how it is sometimes difficult to recognize the nature of fibrous dysplasia on MR studies.) F: A second patient with a fibro-osseous lesion of the ethmoid complex. The matrix is densely calcified (arrow). There are likely trapped secretions or nonossified matrix posterior to the main portion of the lesion (white arrowhead). The sphenoid sinus is obstructed, and the lateral wall has a slightly expanded appearance (black arrow) suggesting an early secondary sphenoid sinus mucocele.
IMAGING APPROACH
Techniques and Relevant Aspects
In general, these fibro-osseous anomalies are best evaluated with standard, noncontrast, high-resolution facial bone imaging. Specific protocols by indication appear in Appendix A. Magnetic resonance imaging (MRI) may be used adjunctively in very limited circumstances, such as when there is doubt about the diagnosis as well as doubt about it actually being an infiltrating process with dural or other intracranial extension. Occasionally, complicating mucocele or infection might be evaluated with MRI for reasons discussed in Chapter 84.
Pros and Cons
The pattern of primary bone diseases and proper diagnosis generally will be much more apparent on CT than MRI (Figs. 40.8 and 91.1). In fact, when diffuse, bilateral, and reasonably symmetric changes are present, even relatively advanced disease can go unnoticed on MRI. Even when primary bone disease is localized, fibrous dysplasia and other fibro-osseous lesions can present very confusing findings, sometimes mimicking a more threatening mass on MRI while the benign and specific nature of the disease becomes quite obvious on CT. MRI really should be limited to problem solving in these types of disorders as suggested previously.
FIBROUS DYSPLASIA
Fibrous dysplasia of the cranial and facial bones is usually an isolated “monostotic” phenomenon, although it very often involves more than one contiguous part of the facial bones—for instance, being frontoethmoidal or sphenoethmoidal in its full extent (Figs. 40.8 and 91.2). It can also be part of a more widespread polyostotic process and associated with endocrine problems, as with Albright syndrome.
The craniofacial form of the disease is very common. It is often discovered incidentally on imaging studies done for unrelated complaints (Figs. 40.8 and 91.3). The maxilla, ethmoid, sphenoid, mandible, and bones of the calvarium may be involved (Figs. 40.1–40.6). Isolated areas in the sphenoid bone are often detected as bright areas in the base of the sphenoid bone on MRI as incidental findings (Fig. 40.5). These may need to be differentiated from areas of fat in the skull base or zones of arrested sphenoid sinus aeration or a skull base transitional status in preparation for sphenoid sinus aeration. Whatever the case, such areas are almost always of low biologic activity and will be of no ultimate consequence to the patient. If multifocal (Figs. 40.6) or polyostotic (noncontiguous) disease is present, a syndromic association may be considered.
When clinical concerns related to fibrous dysplasia arise, they are most commonly related to cosmesis. Functional problems do arise and include malocclusion, visual disturbances, and possibly compressive cranial neuropathy where the cranial nerves exit the skull (Fig. 40.1). There may also be initial concerns about the lesion in question representing a more ominous condition.
Fibrous dysplasia may enter into a rapid growth phase during pregnancy and adolescence (Fig. 40.3). In the latter instance, differentiation from a juvenile active ossifying fibroma (JAOF) (Fig. 40.7) might be difficult, and that lesion must be brought into the differential consideration.
Treatment is surgical and aimed at restoring cosmesis and preventing functional losses (Fig. 91.2). Recent advances in craniofacial surgery and three-dimensional treatment planning have led to improved results in these patients.
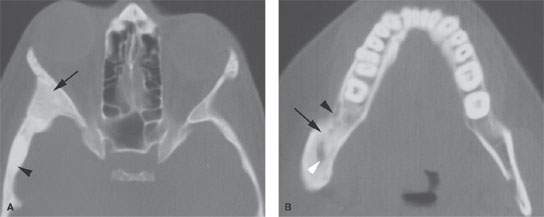
FIGURE 91.2. Two patients with fibrous dysplasia demonstrating slightly different appearances of the matrix. The cases are also meant to show that the distribution may be isolated or involve multiple bones of the face and skull. A: Patient 1. Computed tomography scan showing a homogeneously expanded appearance of the greater wing of the sphenoid (arrow) that continues into the squamous portion of the temporal bone (arrowhead). B: Patient 2. Another patient with fibrous dysplasia showing a relatively homogeneous and fairly dense amount of matrix calcification (arrow) that continues anteriorly, almost mimicking subperiosteal reaction (black arrowhead), and a more central area of nonossified matrix (white arrowhead). This is proven fibrous dysplasia, although on first observation one might be reasonably concerned about chronic osteomyelitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree