Fig. 21.1
Single shot fast spin echo T2-weighted coronal (a, b) and axial (c, d) images. Intraoperative photograph of the pancreatic mass (e). Photograph of the gross specimen (f)
Case 2
A 56-year-old female with a history of lung infection with an incidental pancreatic mass (arrows) found on a surveillance CT of the chest. The patient underwent a distal pancreatectomy and splenectomy. What is your diagnosis?
(a)
Pancreatic adenocarcinoma in a background of IPMN
(b)
Acinar cell carcinoma
(c)
Malignant mucinous cystic tumor
(d)
Moderately differentiated adenocarcinoma, with peripancreatic fat, lymphovascular invasion, and perineural invasion
(e)
Poorly differentiated neuroendocrine neoplasm, with peripancreatic fat, lymphovascular invasion, and perineural invasion
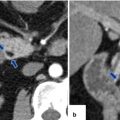
Fig. 21.2
CECT axial (a) and contrast-enhanced fat-suppressed gradient echo T1-weighted axial (b) images. Microscopic examination H&E (c–f)
Case 3
A 51-year-old male with history of a chronic cough. Surveillance CT (a) of the chest and MR (b, c) of the abdomen reveal a pulmonary lesion in the right lung ( arrow ) and two lesions in the pancreas ( short arrows ). The lesions show an avid uptake of FDG on PET/CT (d, e) ( arrowheads ), (f) (arrow). What is the most probable diagnosis?
(a)
Multifocal pancreatic adenocarcinoma with pulmonary metastases
(b)
Pulmonary and pancreatic tuberculosis
(c)
Primary carcinoma of the lung with pancreatic metastases
(d)
Primary lung carcinoma, synchronous with pancreatic serous cystadenomas
(e)
Disseminated B-cell lymphoma
Fig. 21.3
CECT coronal image (lung window of the chest) (a). Contrast-enhanced fat-suppressed gradient echo T1-weighted axial images of the pancreas (b, c). PET/CT axial images of the pancreas (d, e) and coronal image of the lung (f)
Case 4
Correlate the intraductal papillary mucinous neoplasm (IPMN) with the epithelium subtype:
1.
Intestinal ( )
2.
Oncocytic ( )
3.
Gastric/foveolar ( )
4.
Pancreaticobiliary ( )
Fig. 21.4
Histological examination (a–d) (H&E)
Case 5
Correlate diagnosis with ultrasonographic findings:
1.
Chronic pancreatitis ( )
2.
Acute pancreatitis ( )
3.
Pancreatic necrosis ( )
4.
Autoimmune pancreatitis ( )
Fig. 21.5
Transverse scanograms of the pancreas (a–d)
Case 6
Patient with history of a pancreatic mass ( arrows ) who underwent a distal pancreatectomy and splenectomy. What is the histopathologic diagnosis?
(a)
Malignant intraductal papillary mucinous neoplasm (IPMN)
(b)
Pancreatic lymphoma
(c)
Pancreatic adenocarcinoma
(d)
Acinar cell carcinoma of the pancreas
(e)
Autoimmune pancreatitis
Fig. 21.6
CECT axial images of the pancreas (a, b). Histological examination of the resected specimen (H&E) (c) and IgG4 stain (d)
Case 7
A 40-year-old female with an incidental finding on CT. What is your diagnosis?
(a)
Annular portal vein
(b)
Duodenal villous adenoma
(c)
Annular pancreas
(d)
Duodenal adenocarcinoma
(e)
Ectopic pancreas
Fig. 21.7
CECT volume rendered axial (a), coronal (b), oblique (c), and sagittal (d) images of the pancreas
Case 8
Findings on the contrast-enhanced CT images below are suggestive of:
(a)
Autoimmune pancreatitis
(b)
Diffuse pancreatic adenocarcinoma
(c)
Acute interstitial pancreatitis
(d)
Central gland necrosis
(e)
Necrotizing pancreatitis
Fig. 21.8
CECT axial (a, b) and coronal (c, d) images of the pancreas
Case 9
A 38-year-old female with history of mild left flank pain, nausea, and vomiting. Incidental pancreatic mass (arrows) was found on an abdominal CT surveillance for renal stones. Mass was resected with laparoscopic distal pancreatectomy and splenectomy. What is your diagnosis?
(a)
Mucinous cystic tumor
(b)
Solid pseudopapillary tumor of the pancreas
(c)
Olygocystic serous cystadenoma
(d)
Pancreatic pseudocyst
(e)
Cystic neuroendocrine neoplasm
Fig. 21.9
Single-shot fast spin echo T2-weighted axial (a) and coronal (b) images. Photograph of bivalved gross specimen (c). Histological examination (H&E) (d, e) and immunostain with B-catenin (f)
Case 10
Patient with history of acute pancreatitis, persistent epigastric pain, and abdominal distention. MR findings are suggestive of:
(a)
Pancreatic pseudocyst
(b)
Acute interstitial pancreatitis
(c)
Central gland necrosis
(d)
Hemorrhagic pancreatitis
(e)
Infected pancreatic necrosis
Fig. 21.10
Single-shot fast spin echo T2-weighted axial (a, b) images and contrast-enhanced fat-suppressed gradient echo T1-weighted axial (c, d) images
Case 11
Patient complaining of epigastric pain after a pyloric sparing pancreaticoduodenectomy performed 5 days prior. CT findings are suggestive of:
(a)
Pancreatic pseudocyst
(b)
Pancreatic hemorrhage
(c)
Pancreaticojejunostomy leakage
(d)
Duodenojejunostomy leakage
(e)
Afferent loop obstruction
Fig. 21.11
CECT axial (a, b) and coronal (c, d) images of the pancreas
Case 12
CT and MR findings of the pancreas and the kidneys may be associated with:
(a)
Birt–Hogg–Dube syndrome
(b)
Erdheim–Chester disease
(c)
von Hippel–Lindau syndrome
(d)
MEN type 1
(e)
MEN type 2
Fig. 21.12
Non-contrast CT axial (a, b) images and fat-suppressed T2-weighted axial images (c, d)
Case 13
A 40-year-old male with history of AIDS and chronic diarrhea. What is your diagnosis?
(a)
Acinar cell carcinoma
(b)
Groove pancreatitis
(c)
Secondary pancreatic lymphoma
(d)
Insulinoma
(e)
Gastrinoma
Fig. 21.13
Anterior view of an upper gastrointestinal series (a), CECT axial (b) image of the pancreas. Color power Doppler axial (c) image of the mass. Octreotide scan, coronal (d) image
Case 14
Correlate ultrasonographic findings of these four cystic masses of the pancreas with the diagnosis:
1.
Serous cystadenoma ( )
2.
Mucinous cystic tumor ( )
3.
Solid pseudopapillary tumor ( )
4.
Main duct-type IPMN ( )
Fig. 21.14
IOUS of the pancreas (a–d)
Case 15
A 39-year-old female with a questionable pancreatic head mass on abdominal CT. MR of the pancreas was performed for further evaluation of this finding. What is your diagnosis?
(a)
Pancreatic neuroendocrine neoplasm
(b)
Acinar pancreatic carcinoma
(c)
Invasive malignant intraductal papillary mucinous neoplasm (IPMN)
(d)
Ectopic pancreas (duodenum)
(e)
Normal variant of the pancreatic head morphology

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree