Fig. 12.1
(a) ICG-Fluorescence imaging visualized the extrahepatic bile ducts in the hepatoduodenal ligament. (b) After ligation and division of the right hepatic artery and the right portal vein, ICG-fluorescence cholangiography was performed again. The confluence of the left hepatic duct (arrow) and the right hepatic duct (arrowhead) as well as the tiny bile duct from segment I (white arrowhead) were clearly delineated. (c) The right hepatic duct was ligated, referring to the fluorescence images of the bile ducts
The major advantage of fluorescence cholangiography during laparoscopic hepatectomy is that it enables visualization of the biliary tract in relation to the surrounding structures from various angles in real-time. In addition, it can save time and avoid bile duct injury associated with insertion of a tube for the injection of contrast material when using radiographic cholangiography [24]. Fluorescence cholangiography is expected to complement conventional radiographic cholangiography, though it has limitations in tissue-penetration ability of ICG fluorescence up to 5–10 mm [15] and delineation of the intrahepatic bile ducts.
Clinical Application for Identification of the Left Hepatic Duct with Severe Adhesion
Figure 12.2 shows a case of a patient who underwent laparoscopic left hepatectomy for two colorectal liver metastases 3 years after open sigmoidectomy and lymphadenectomy of hepatoduodenal ligament. Due to the severe adhesions around hepatoduodenal ligament following lymphadenectomy, the anatomy of the hepatic vessels and the biliary ducts were not identified by gross appearance. To avoid their injury, we attempted to identify them using a fluorescence imaging technique. This showed clear fluorescence of the extrahepatic ducts in the hepatoduodenal ligament (Fig. 12.2a and Video 12.2). Based on the information, the left portal vein and the hilar plate containing the left hepatic duct were dissected and identified (Fig. 12.2b), after which the left portal vein was ligated (Video 12.2).
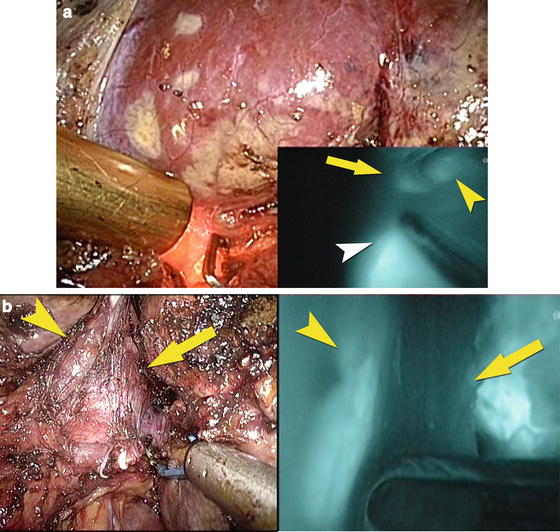
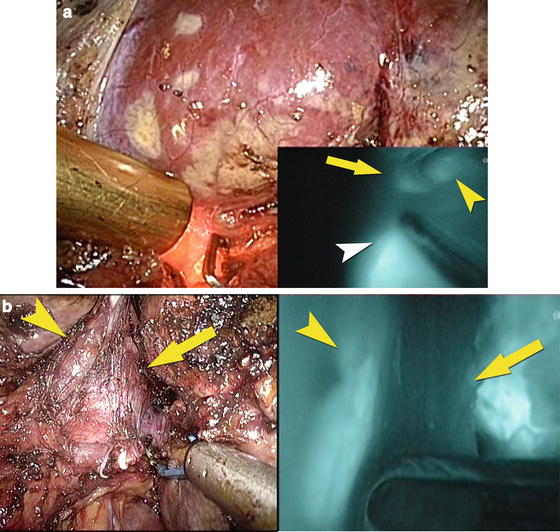
Fig. 12.2
(a) ICG-Fluorescence imaging visualized the extrahepatic bile ducts which were grossly unidentifiable because of the severe adhesions around the hepatoduodenal ligament. (b) After dissection of the left portal vein and the hilar plate, ICG-fluorescence cholangiography was performed again. The left hepatic duct in the hilar plate was visualized as fluorescence, while the left portal vein was identified as the defect of fluorescence
ICG-fluorescence cholangiography is useful for identifying the anatomy around the liver with severe adhesions following previous surgery. This technique may complement the theoretical disadvantage of laparoscopic hepatectomy lacking tactile feedback and serves as a guide for surgeons to identify the anatomy of the hepatic vessels during surgery.
Identification of Segments
Administration of ICG
For identification of segments as fluorescence, ICG (0.025 mg in 10 mL of normal saline) was administered into the portal branch through a needle after its puncture. In contrast, for identification of segments as the defect of fluorescence, ICG (2.5 mg in 1 mL of normal saline) was injected intravenously after clamping of the glissonian pedicle with interest.
Clinical Application of Positive-Staining Technique
Figure 12.3 shows a case of a patient with a colorectal liver metastasis located in segment IV after right hepatectomy. Due to the severe adhesions around the liver and the regeneration of the remnant left liver after previous right hepatectomy, both vascularization in the liver and the tumor-bearing segment were unclear. In order to identify its segment, the suspected portal branch of the tumor-bearing segment was identified by IOUS and punctured with a 22-gauge spinal needle, which was introduced through the abdominal wall and a guide hole on the flexible laparoscopic ultrasonographic probe (BK medical, Herlev, Denmark). After ICG (0.025 mg in 10 mL of normal saline) was administered into the portal branch through the needle, the liver surface corresponding to segment IVb started to fluoresce. The liver surface of the segment IVb provided clear fluorescence less than 5 min after the injection, after which the resection of the anatomical segment IVb was performed (Video 12.3).
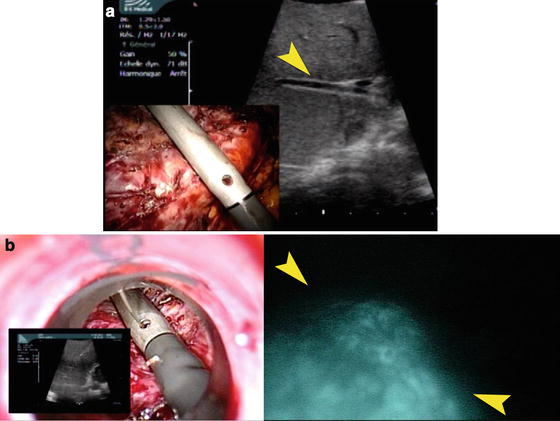
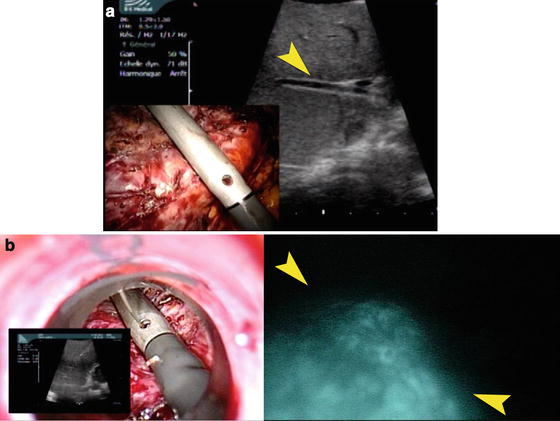
Fig. 12.3
(a) IOUS identified the portal vein flowing into the segment IVb (arrowhead) where the tumor was located. (b) After the puncture of the suspected portal vein of the tumor-bearing segment (left) and injection of ICG, the border between the segment IVb and the segment II/III was identified (arrowheads, right)
Clinical Application of Negative-Staining Technique
Figure 12.4 shows a case of a patient with a colorectal liver metastasis located in segment VI. Anatomical resection of segment VI was attempted to ensure the surgical margin, because intraoperative ultrasound (IOUS) revealed the tumor near from the root of the glissonian pedicle (Fig. 12.4a and Video 12.4). In order to identify the hepatic segment, the glissonian pedicle for segment VI was dissected while using IOUS. After temporarily clamping its root (Fig. 12.4b) and intravenous injection of ICG (2.5 mg), all hepatic segments except for segment VI provides clear fluorescence less than 5 min after injection (Fig. 12.4c). The resection line was marked with ultrasonic laparoscopic coagulation shears (Fig. 12.4d), after which anatomical resection of segment VI was performed. ICG-fluorescence imaging detected no bile leak on the raw surface of the liver after resection (Video 12.4).
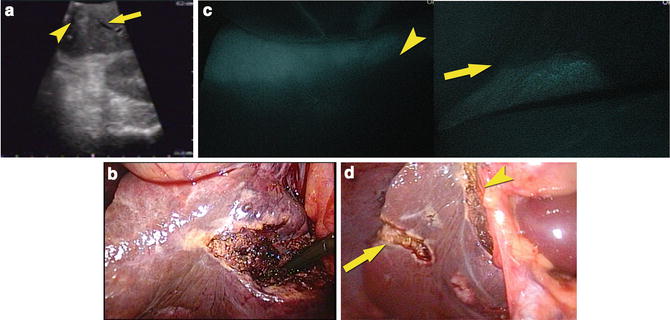
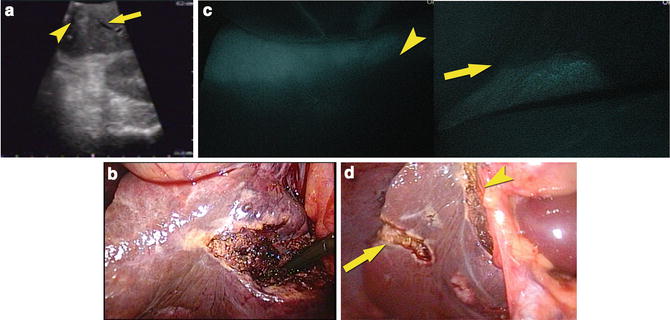
Fig. 12.4
(a) IOUS identified a tumor (arrowhead) and the glissonian pedicle flowing into the segment VI (arrow). (b) The gross appearance of the liver surface before injection of ICG with the glissonian pedicle clamped. (c) Fluorescence imaging on the liver surface of the segment V and VI (left) and that of the segment VI and VII (right). Segment VI was visualized as defect of fluorescence, and the borderline between segment V and VI (arrowhead) and that between segment VI and VII (arrow) were identified, respectively. (d) The gross appearance of a tumor and segment VI which was identified and marked with ultrasonic laparoscopic coagulation shears (arrowhead and arrow)
Usefulness of Identification of Segments Using ICG-Fluorescence Imaging
These techniques which enable identification of hepatic segments as defect of fluorescence were reported as the positive- or negative-staining technique in authors’ group [8]. The advantage of the negative-staining technique is not technically complicated as compared to the positive-staining technique [8] which requires to perform an image-guided puncture of a portal branch during surgery under laparoscopic control or through abdominal wall before surgery. Although laparoscopic anatomical liver resection is a technically demanding procedure [25], surgeons need to perform it to achieve equivalent oncological outcome for the treatment of hepatocellular carcinoma [26, 27] compared to open hepatectomy. These techniques guide surgeons to clearly identify the hepatic segments before transection of the liver parenchyma, ensuring accurate and efficacious laparoscopic anatomical hepatectomy and probably less postoperative secondary bile leak or abscess due to a devascularized parenchyma in the remnant liver.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree