Fluoroscopy is a type of imaging technique in which real-time movements of body organs and radiopaque contrast material are visualized. During a fluoroscopic examination, the operator or radiologist controls the functions of radiography equipment and x-ray tubes for real-time imaging of the patient. In abdominal imaging, fluoroscopy has a role in the diagnosis of various clinical conditions with gastrointestinal studies, postoperative studies, genitourinary studies, and more.
Technical Aspects
Fluoroscopy
History
Early fluoroscopes had an x-ray tube and fluorescent screen made of barium platinocyanide. Gradually, the screens were replaced by cadmium tungstate and then zinc-cadmium sulfide, which produced a yellow-green emission.
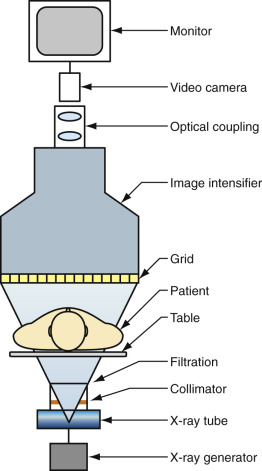
Fluoroscopy has evolved from the early days of images on a fluoroscopic screen of poor quality, a dark radiography room, and eye adaptation with red goggles to improved images with image intensifiers, video-recorders, and a variety of C-arm machines. Currently, it is available in many different configurations for use in various clinical applications. With technologic advancements in hardware and image processing, fluoroscopy has gained substantially both qualitatively and quantitatively. The introduction of flat-panel detectors, high-quality image intensifiers with video-recording capabilities, state-of-the-art C-arm design, and digital units has revolutionized the field of fluoroscopic imaging. The superior spatial and contrast resolution combined with faster image reconstruction and reduced radiation along with a variety of safe and effective contrast media has empowered fluoroscopy with advanced capabilities in the diagnostics and interventional realm. A variety of fluoroscopic units are now commercially available, and the components of basic fluoroscopic equipment are shown in Figure 2-1 . The main uses of fluoroscopy are listed in Box 2-1 .
- •
Gastrointestinal imaging
- •
Genitourinary imaging
- •
Angiography
- •
Other:
- •
Intraoperative
- •
Foreign-body removal
- •
Musculoskeletal
- •
Patient Preparation
It is important to have the patient empty his or her stomach to increase the sensitivity of the fluoroscopy examination, because food and food residue can mimic disease. Informed consent is required, and any medical history such as heart disease, asthma, allergy, thyrotoxicosis, and hypersensitivity to drugs should be elicited. Also important to consider: What medications (e.g., insulin) is the patient using? Is the patient pregnant or breast-feeding? Has there been a recent diagnosis of small bowel obstruction or perforation and, if so, what were the surgical details?
Patients scheduled for a double-contrast barium enema must adhere to a clear liquid diet for 24 hours before the procedure. Laxatives may be prescribed to ensure thorough bowel cleansing, and on the morning of the examination a bisacodyl suppository is given per rectum.
However, in the acute/emergency or postoperative setting, patient preparation is usually optional. Moreover, in this setting, iodinated contrast media are preferred over barium sulfate because the latter might interfere with a surgical procedure and any extraluminal collection of barium may create confusion with a diagnosis on subsequent examinations. A medical history of severe hypersensitivity to iodinated contrast media or certain medications should be obtained if the procedure requires its use.
Fluoroscopic Examinations
Fluoroscopic examinations are of two types: single-contrast studies and double-contrast studies ( Box 2-2 ). Single-contrast studies are performed either with barium or with iodinated contrast media. For double-contrast media, air or carbon dioxide is used ( Figure 2-2 ).
Single-Contrast Studies
- •
Precise control of barium column
- •
Easier identification of filling defects
- •
In suspected perforation, single contrast with water-soluble medium preferred
- •
Can be used to evaluate mechanical problems (e.g., obstruction, fistula)
- •
Optimal for patients unable to swallow gas-forming tablets
Double-Contrast Studies
- •
Thick barium coats lumen, and effervescent tablets ingested to distend lumen with air
- •
Produced see-through effect with better assessment of mucosal details
- •
Better distention and separation of the bowel loops
- •
Better detection of small mucosal lesions, polyps, ulcers

Gastrointestinal Fluoroscopic Procedures
- •
Stomal examinations, enema through ileostomy or colostomy for patency, recurrence of disease, and leak
- •
Feeding tube studies
- •
Oral cholecystogram and T-tube cholangiogram
- •
Hydrostatic reduction of pediatric abdominal emergencies such as intussusceptions and sigmoid volvulus
Genitourinary Fluoroscopic Procedures
- •
Cystography for evaluation of urinary bladder and vesicoureteric reflux
- •
Voiding cystourethrography for visualization of urethra
- •
Retrograde urethrography for anterior urethra
- •
Hysterosalpingogram for uterus and fallopian tubes
Interventional Procedures
- •
Placement of vascular catheter and stents
- •
Percutaneous biliary drainage procedures
- •
Urologic procedures: Retrograde pyelography, percutaneous nephrostomies, and suprapubic cystotomies
Other Examinations
- •
Sinogram
- •
Fistulogram
Fluoroscopic Contrast Agents
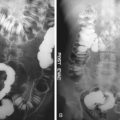
Fluoroscopic contrast agents are compounds that enable improved visualization of internal luminal structures, spaces, and tracts and also delineate tubes and catheters on fluoroscopy or radiography ( Figure 2-3 ).
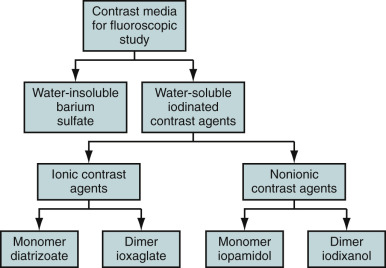
Fluoroscopic contrast agents can be divided into two types: positive contrast and negative contrast. A positive contrast medium absorbs x-rays more strongly than the surrounding tissue or organ being examined and appears radiopaque. A negative contrast medium absorbs x-rays less strongly and hence appears radiolucent. Positive contrast media are barium and iodine compounds ( Figures 2-4 and 2-5 ). Negative contrast media can be obtained by air or carbon dioxide ( Figure 2-6 ).

Barium
The higher the concentration of the barium sulfate suspension, the thinner are the layers that can be identified in the radiograph. The more viscous is the suspension, the better is the penetration into the finest folds and the more differentiated are the structures that become visible. Different barium preparations available for use are shown in Figure 2-7 . Various barium suspensions used for the evaluation of different parts of gastrointestinal tract are depicted in Table 2-1 .
| Gastrointestinal Tract Study | Barium Formulations (%) |
|---|---|
| Barium swallow | Single contrast: 50-100 w/v Double contrast: 250 w/v |
| Upper gastrointestinal tract (stomach and duodenum) | Single contrast: 35-80 w/v Double contrast: 250 w/v |
| Small bowel follow-through | 40-60 w/v |
| Enteroclysis | 50-95 w/v |
| Retrograde ileography | 20-25 w/v |
| Barium enema | Single contrast: 12-25 w/v Double contrast: 60-120 w/v (80 commonly used) |
Properties desirable for the conventional upper gastrointestinal and per-oral small bowel examinations include suspension stability, good coating ability for double-contrast views, and resistance to flocculation in the small intestine. For dense, uniform coating in the esophagus, stomach, duodenum, and colon, it is also desirable that the barium suspension have the ability to delineate fine mucosal surface details with reasonable flow rate and resistance to flocculation.
Water-Soluble Contrast Agents
Water-soluble contrast agents can be divided into ionic or nonionic agents or, depending on the osmolarity, as high- and low-osmolar agents (see Figures 2-3 and 2-8 ). Ionic contrast media have higher osmolarity and more side effects. Nonionic contrast media have lower osmolarity and tend to have fewer side effects. Water-soluble organic iodine compounds are used in certain circumstances in which barium is contraindicated—for instance, in suspected perforation of gut into the free peritoneal cavity, in postoperative cases to look for a leak, or when the risk for aspiration into the lung is high. Barium leakage into the peritoneal cavity can lead to formation of granuloma, and aspiration into the lung can leak to pneumonitis or pulmonary edema.