9 Functional Analysis and Surgery of the Spine in an Open MR System
Contents
Functional Analysis of the Spine
Examination of the Spine in the Seated Position
Intervertebral Disk Height in Relation to the Time of Day and Examination Position
Functional MR Myelography of the Lumbar Spine
Minimally Invasive Spinal Surgery
Soft- and hardware innovations over recent years now allow images to be obtained in real time (Debatin et al., 1998). In combination with the increasing availability of open-configuration scanners, the high temporal resolution of the image acquisition allows, on the one hand, functional examinations to be carried out for the entire musculoskeletal system (Schenck et al., 1995), as well as real-time guidance of minimally invasive interventions (Jolesz and Kikinis, 1995; Lufkin, 1995). As this chapter will show, both aspects are of direct relevance to the spinal column.
Open Configured MR Systems
Two goals are pursued with the open construction of MR systems:
• improved access to the patient during image acquisition (Lenz and Dewey, 1995),
• the patient should be allowed more freedom of movement during the examination.
Furthermore, sufficient room must be available for instruments (surgery) or for positioning aids (functional examinations).
Open-configuration scanners are primarily judged by the strength of the “main magnet,” which generates the static magnetic field and is the deciding factor for the type of system. In this respect, it should be borne in mind that the signal-to-noise ratio is proportional to the field strength. The signal in a 1.5 tesla environment is therefore three times higher than at 0.5 tesla. The gradient coils used determine the degree of spatial resolution and the rate of data acquisition. High-performance gradients have so far only been used in high-field systems. Furthermore, the systems also differ with respect to their radio-frequency coils (RF coils) for transmission and reception of the MR signal. As regards the “gap,” systems are available with a vertical patient access and others with a horizontal access. The currently commercially available open MR systems can be divided into three categories.
Categories of open MR systems
 Closed high-field system with a wide short-bore magnet (Example: 1.5 tesla Gyroscan ACS-NT).
Closed high-field system with a wide short-bore magnet (Example: 1.5 tesla Gyroscan ACS-NT).
 Open mid-field system with a vertical access (Example: 0.5 tesla Signa SP).
Open mid-field system with a vertical access (Example: 0.5 tesla Signa SP).
 Open low-field system with a horizontal access (Example 0.2 tesla Magnetom Open).
Open low-field system with a horizontal access (Example 0.2 tesla Magnetom Open).
Furthermore, there are numerous other systems whose description would be beyond the scope of this chapter. The open MR systems can also be combined with other systems, such as a fluoroscopy unit or an ultrasound apparatus, to form what are known as “hybrid units.”
The different systems have their various advantages and disadvantages. High-field systems, for example, allow better image quality at a higher acquisition rate. On the other hand, access to the patient is markedly poorer with high-field systems than with the open mid- and low-field systems. This makes interactive operations difficult in the high-field system. Low-field systems allow better access and more freedom of movement, yet at the price of a markedly reduced image quality and, above all, a clearly restricted temporal resolution. The horizontal gap usually associated with the majority of low-field systems is clearly inferior to the vertical access as far as freedom of movement for the patient and the interventionalist is concerned.
The mid-field system cited above was designed as a dedicated interventional MR system (Fig. 9.1).
The system is provided with a vertical, 58-cm-wide gap between the coils of the main magnetic field and there is enough room for direct access to the patient as well as for freedom of movement for functional examinations. There are two liquid crystal monitors mounted in the gap on to which the acquired MR images are projected (Fig. 9.2).
It is not possible to use volume coils due to the open construction of the MR system. Signal transmission and reception are accomplished by flexible transmitter and receiver coils of various sizes (Fig. 9.3).
To depict the spine, a homogenous high-frequency field is generated using a butterfly coil with two opposing elements (attached anteriorly and posteriorly onto the patient). Care should be taken that the high-frequency field is not parallel to the BO field when the patient is seated. The image quality achieved in this way lies between that of high- and low-field systems. Spatial resolution is sufficient for a comprehensive diagnostic work-up of the spinal column.
An open mid-field system (Signa SP, GE Medical Systems) was installed in the MR Center of the University Hospital of Zurich in autumn 1995. The practical knowledge reported in this chapter is based primarily on our experience gained with this system.

Fig. 9.1 Open superconducting interventional 0.5 tesla MR system (Signa SP, General Electrics). Between the two magnets that induce the main magnetic field is a gap 58 cm wide offering room for additional installations or free access to the patient during interventions.
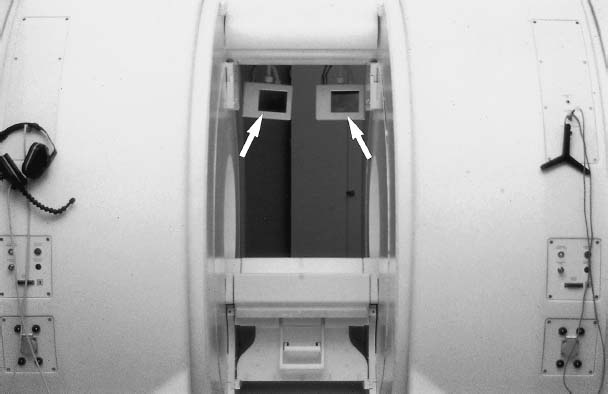
Fig. 9.2 Detail picture of the open MRI scanner. The latest image data are conveyed to the examiner via two LCD monitors (arrows), e.g. for the intervention guidance. The examiner can communicate with the patient directly from the control desk via headphones or, during interventions, the radiologist with assistants outside the scanning room.
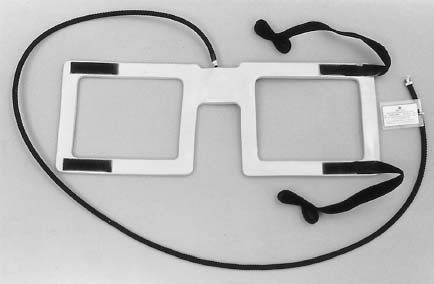
Fig. 9.3 Butterfly coil required for transmission and reception. The coil is attached to the patient over the site to be examined and connected to the magnet via a cable.
Functional Analysis of the Spine
Functional studies of the spine are performed for a large number of disorders, including degenerative diseases. Compression of the spinal cord can develop secondarily to degenerative diseases, resulting in their final stage in cord atrophy and producing the clinical picture of cervical myelopathy (Kunze and Arlt, 1991). Functional examinations, however, have also proven themselves in inflammatory diseases of the spine, as in for example rheumatoid arthritis (Roca et al., 1993) and trauma-related disorders (Mirvis et al., 1988; Rothhaupt and Liebig, 1994).
All available imaging techniques, including myelography, CT and MRI, have already been studied with regard to their suitability for the assessment of spinal function (Muhle et al., 1995). MR examinations were usually performed in closed systems, simulating motion sequences or changes in posture with mechanical aid appliances (such as non-metallic, MR-compatible positioning devices) (Naegele et al., 1992). However, all of these studies were of a static nature, i.e. spinal morphology was compared in at least two or several static conditions. Only fluoroscopy has hitherto allowed demonstration of the actual dynamic sequence of motion and the pathological aspects arising from this. Limited contrast and problems of overlapping, however, considerably restrict the use of fluoroscopy for the functional assessment of the spinal column, even if myelographic contrast media is applied (Wildermuth et al., 1997).
Given the use of fast data acquisition strategies, examinations using the open MRI, on the other hand, allow the presentation of dynamic motion sequences with the aid of tomographic data, in any slice orientation and with an inherently high soft-tissue contrast. In addition, the vertical type of gap allows the examination of the patient in both the seated and standing positions.
Examination of the Spine in the Seated Position
There are a few precautions to be taken in the interests of optimum image quality when examining the spine by MRI in the seated position. GRE sequences should be used because of their shorter acquisition time and low sensitivity to field inhomogeneities. In order to minimize arbitrary patient movements and to prevent coil movements relative to the spine, the patient should be secured as well as possible in a rigid corset or on a special chair (Fig. 9.4).
Only those movements relevant to the functional examination should be allowed. The examination parameters, such as phase encoding in the craniocaudal direction, field of view and image matrix, must be adjusted to individual needs. By taking these aspects into consideration, the lumbar spine can be comprehensively displayed in the seated position in high image quality (Schoenenberger et al., 1996).
Intervertebral Disk Height in Relation to the Time of Day and Examination Position
Assessment of intervertebral disks is often based on their height, which is subject to change during the course of the day, however, and is above all dependent upon position. Since the majority of patients have hitherto only been examined lying down, these aspects were only of minor consequence. In order to quantify these interrelations, which may well be of some significance in the assessment of functional MR images, the height as well as the proton density (as an indication of the water content) of lumbar intervertebral disks were assessed over the course of the day in 10 healthy volunteers in the sitting and lying positions (Schoenenberger et al., 1996; Duwell et al., 1996).
There was a marked reduction in disk height throughout the day, especially in the seated position. The most conspicuous difference in height was detected in the L4/L5 segment (0–2 mm). Interestingly, the proton density of the intervertebral disks did not demonstrate any significant differences at the various times of day. Yet, on the other hand, the transition from the lying to the seated position was characterized by a considerable reduction in proton density (Fig. 9.5).
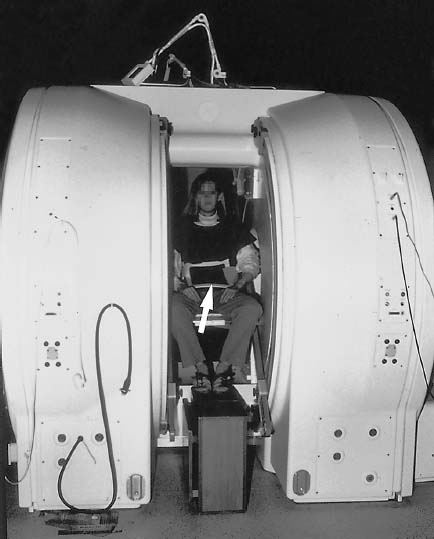
Fig. 9.4 Examination of the lumbar spine in the seated position. The vertical part of the butterfly coil is well visible (arrow).
Considering these results, two aspects appear to influence disk elasticity:
• slow morphological changes within the disk during the course of the day,
• fast changes resulting from fluid content displacements when position is altered (Duwell et al., 1996).
The second aspect deserves particular attention when assessing examinations of the spine in the seated position.
Functional MR Myelography of the Lumbar Spine
Stenosis of the spinal canal, the lateral recesses and the neuroforamina are usually indications of degenerative changes of the spinal column, which generally get worse in the course of ageing (Andersson and McNeill, 1992; Hasegawa et al., 1995). These stenoses can appear at several segmental levels. Their exact location and characterization are of great importance prior to initiating therapy, especially before performing decompressive surgery (Bell and Ross, 1992).
Even though it is possible to demonstrate the spinal canal comprehensively using a conventional closed MR system, many surgeons still prefer conventional myelography for preoperative planning, especially for patients with severe scoliosis, implants, or if an important functional component is expected (Jeanneret and Forster, 1993). For this purpose, conventional myelograms are obtained in different functional positions. The fact that the diameters of the spinal canal and neuroforamina are dependent upon position is given consideration by performing measurements in different positions (Schumacher, 1986; Mayoux-Benhamon et al., 1989). Although indispensable for conventional myelography, the intradural application of contrast medium is considered unpleasant by the majority of patients and subsequently leads to a considerable headache in up to 75 % of those examined (Peterman, 1996). Functional MR myelography in the open MR system is just as capable of obtaining the same diagnostic information for the surgeon, yet in a completely non-invasive manner. This has been documented in a recently concluded study (Fig. 9.6) (Wildermuth et al., 1997).
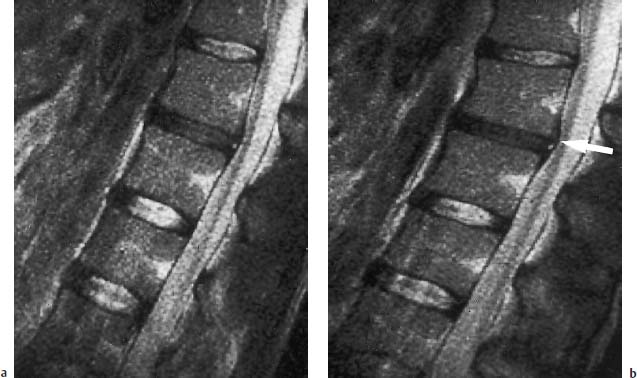
Fig. 9.5 a, b T2-weighted sagittal images of the lumbar spine: Image on the left (a) acquired at 9 a.m. and the image on the right (b) at 6 p.m. The L2/L3 intervertebral disk is dehydrated, the inferior plate of L2 displays a small posterior spondylophyte (arrow). The L3/L4 and L4/L5 disks have lost 2 mm in height during the course of the day.
The lumbar spines of 30 patients were subject to functional studies before surgery, both by using conservative myelography and in the open MR system (Wildermuth et al., 1997). Sagittal T2-weighted SE sequences were acquired for functional MRI examinations in the lying and seated positions (flexion and extension views) using the following parameters:
• TR = 3000 ms, TE = 85 ms,
• echo train length 8,
• bandwidth 16 kHz,
• slice thickness 5 mm with a slice increment of 1.5 mm,
• field size 20 cm,
• 256 × 256 matrix.
Three excitations were averaged. Using the MRI images, the largest sagittal diameter of the spinal canal, on the one hand, and the size of the neuroforamina using electronic measuring points, on the other, were measured from the imaged disk levels of the lumbar spine.
Comparison with data obtained from conventional myelographs produced a good correlation for the sagittal spinal canal diameters (correlation quotient r = 0.94). It was demonstrated that the diameter of the spinal canal varies only little during different types of movement, at least in a symptomatic orthopedic patient population. This result is all the more surprising since in a preceding study on healthy volunteers considerable differences in spinal canal width were shown to be related to movement (Schmid et al., 1997) (Fig. 9.7).

Fig. 9.6a, b Examination of the lumbar spine in the lying position. The multisegmental protrusions with narrowing of the dural sac (arrows) are visible both on conventional myelography and on the median sagittal T2-weighted image:
a Conventional myelography.
b Sagittal T2-weighted image.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


