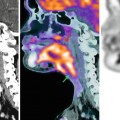
Fig. 50.1
Right retroperitoneal well-differentiated liposarcoma with partial dedifferentiation in a 66-year-old male. The patient underwent contrast-enhanced CT for a medical checkup (a, coronal view; b, axial view), where a large adipocytic tumor arising from the retroperitoneum on the right side was detected. This tumor displaced the right kidney anteriorly, causing hydronephrosis. Although the tumor consisted of adipose tissue for the most part, it also contained solid parts with calcification on the left side (arrows on a and b), which were suspected as areas of dedifferentiation. Figures(c) and (d) show an axial image (at the same level as that shown in b) and a maximum intensity projection image (MIP) of preoperative 18F-FDG PET, respectively. The adipocytic parts, corresponding to well-differentiated liposarcoma, did not show FDG uptake, whereas the solid parts, suspected to represent an area of dedifferentiation, showed elevated FDG uptake (black arrowheads in d). This tumor was diagnosed by histopathological examination of the surgically resected specimen as a well-differentiated liposarcoma with partial dedifferentiation
However, because retroperitoneal well-differentiated liposarcomas have often been present for long periods of time before they are diagnosed and are often larger at the time of detection as compared to the same tumors arising from the extremities, the prevalence of dedifferentiation is higher [17, 18]. Brenner et al. evaluated the 18F-FDG PET findings of 54 patients with liposarcoma and reported that the maximum standardized uptake value (SUVmax) of the well-differentiated subtype was significantly lower than that of the other subtypes, including the dedifferentiated subtype [21]. Nonetheless, 18F-FDG PET may be useful for the detection of dedifferentiated parts (Figs. 50.1 and 50.2). However, further studies are needed to confirm this perception.
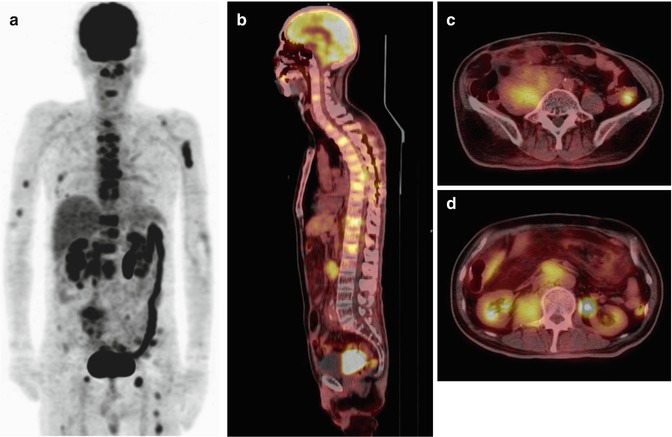
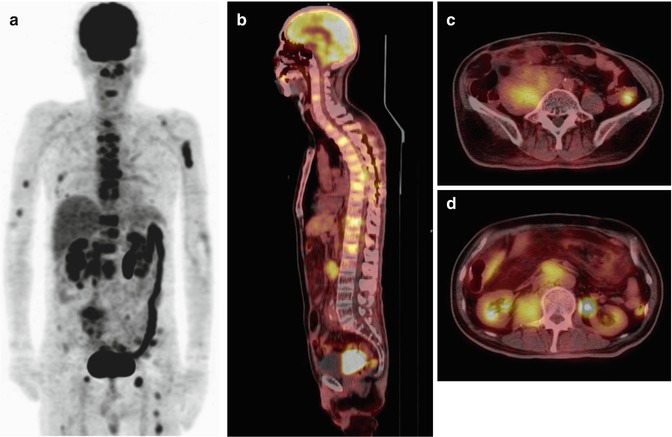
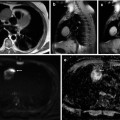
Fig. 50.2
A 60-year-old male with metastatic dedifferentiated liposarcoma was submitted to perform an 18F-FDG PET/CT. The patient had previous history of many operations and radiotherapy for repeated recurrences of well-differentiated liposarcoma, first diagnosed 14 years ago. He complained of a feeling weakness of his lower legs and gait disturbance. He was diagnosed as having compression fracture of the seventh thoracic vertebral body resulting in spinal canal stenosis, followed by emergency vertebral fusion surgery. The histopathological diagnosis was metastatic dedifferentiated liposarcoma of the thoracic vertebra. (a) Coronal MIP of an 18F-FDG PET/CT obtained 2 weeks later and coronal (b) and axial at two different levels (c and d, respectively) fused PET/CT images showed multiple bone metastases (a, b), a right retroperitoneal recurrent tumor (c), and para-aortic lymph node metastases (d)
In addition, Brenner et al. also reported from the same study that the pre-therapy tumor SUV obtained by 18F-FDG PET was a more useful parameter for survival prediction than the tumor grade or tumor subtype [21].
50.3 Leiomyosarcoma
Leiomyosarcoma is the second most commonly encountered (28 %) primary retroperitoneal sarcoma [4, 17]. Although some studies have suggested the usefulness of 18F-FDG PET for the evaluation of uterine leiomyosarcoma [22, 23], there are few reports on the usefulness of this diagnostic modality for retroperitoneal leiomyosarcoma. Punt et al. evaluated the 18F-FDG PET findings of 38 patients with leiomyosarcoma (including retroperitoneal lesions) and reported, based on a univariate analysis, the existence of a correlation between the SUVmax and the tumor grade and tumor size [24]. Because in general, leiomyosarcomas show high FDG uptake (Fig. 50.3), 18F-FDG PET may be useful for the detection of unexpected recurrences or metastases [25].
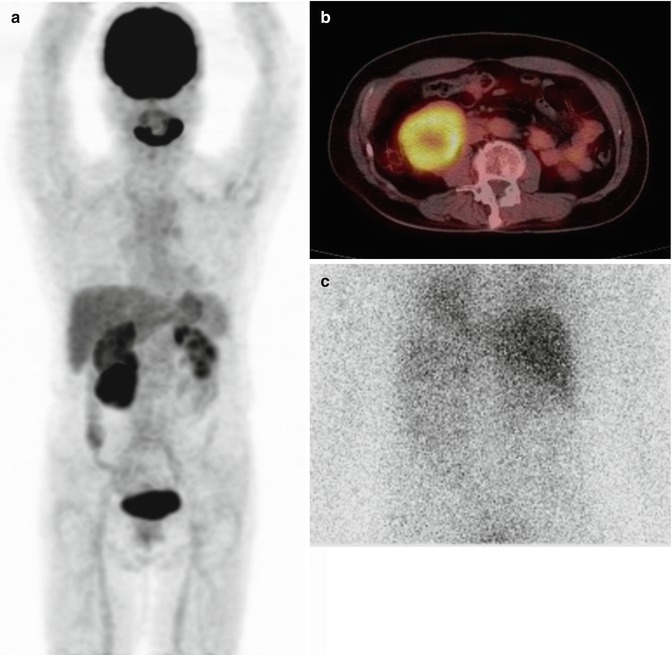
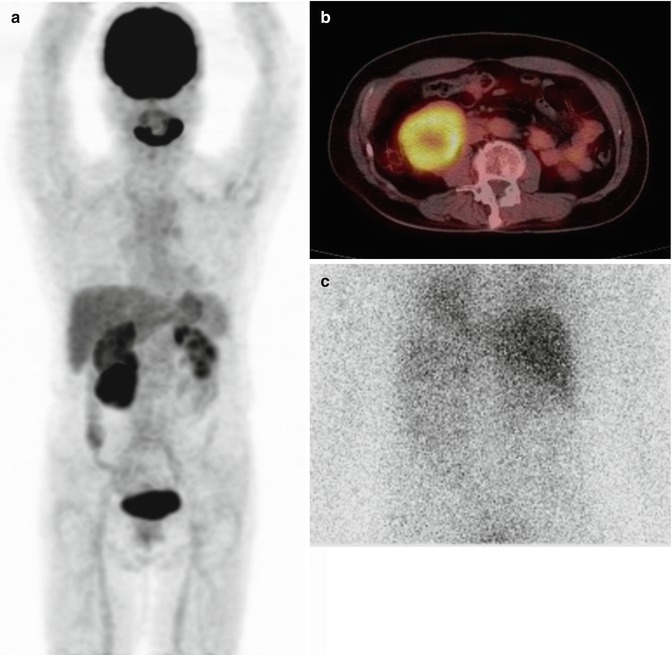
Fig. 50.3
Right retroperitoneal leiomyosarcoma in a 64-year-old female. The patient presented with hypertension of sudden onset, headache, and thumping, and CT revealed the presence of a right retroperitoneal tumor with right hydronephrosis. Coronal MIP of an 18F-FDG PET (a) and axial fused 18F-FDG PET/CT at the level of the tumor (b) showed high FDG uptake in the tumor. Although retroperitoneal pheochromocytoma was suspected according to the clinical symptoms, no uptake was detected on 131I-metaiodobenzylguanidine (MIBG) scintigraphy (c). In addition, the adrenal medullary hormone activities were within normal limits. The tumor was surgically resected with right nephrectomy. The histopathological diagnosis was retroperitoneal leiomyosarcoma
50.4 Malignant Fibrous Histiocytoma
Malignant fibrous histiocytoma (MFH) is the third most commonly encountered (19 %) retroperitoneal sarcoma, and overall, is the most common soft tissue sarcoma [4, 17]. Just as for other malignant tumors, 18F-FDG PET has been suggested to be useful for the evaluation of MFH because of its high FDG uptake [25]. However, there are no reports about the application of 18F-FDG PET for the evaluation of retroperitoneal MFH. Recently, Yokouchi et al. reported that 18F-FDG PET/CT is a promising diagnostic imaging technique for setting safe minimal margins for surgical resection of MFH [26]. However, their six cases of MFH did not include retroperitoneal lesions. Nevertheless, unless the tumor is located near the kidney or urinary tract, which often show physiological FDG uptake, 18F-FDG PET may provide valuable information about the extent of the tumor.
50.5 Neurogenic Tumors
Neurogenic tumors constitute 10–20 % of all primary retroperitoneal tumors [4]. Although they are more likely to be benign and have a better prognosis, patients with neurofibromatosis type 1 (NF1) are at a significantly increased risk of development of malignant peripheral nerve sheath tumors (MPNSTs) , with a lifetime risk of 8–13 % [27]. For patients with NF1, differentiation between benign and malignant tumors has important prognostic and therapeutic implications, and 18F-FDG PET is a sensitive and specific imaging modality for the diagnosis of MPNSTs in patients with NF1 [28, 29] (Fig. 50.4). Furthermore, previous studies have suggested a high sensitivity (94–100 %) and specificity (83–91 %) of 18F-FDG PET for distinguishing between MPNSTs and benign neurogenic tumors even in patients without NF1 [30].
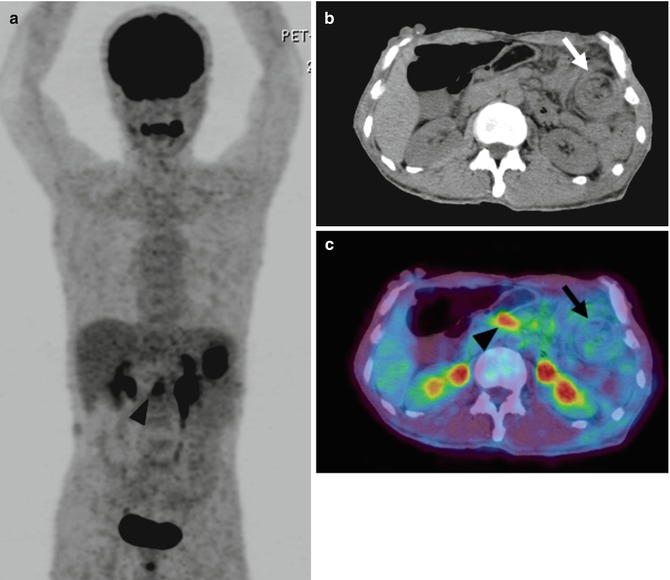
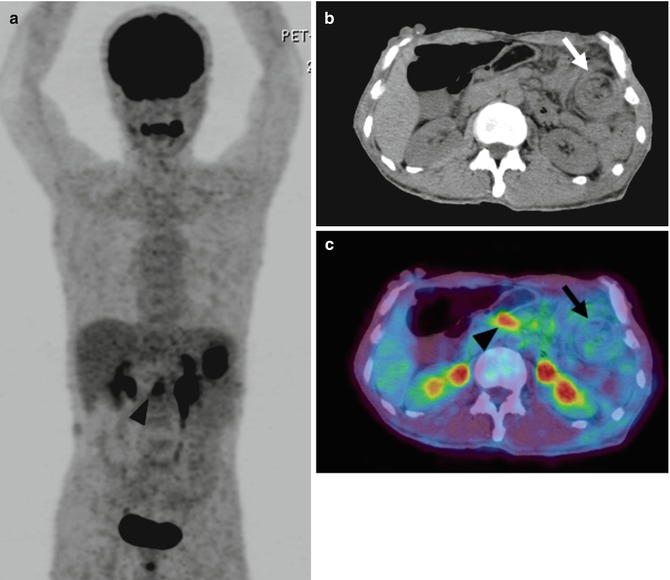
Fig. 50.4
Malignant peripheral nerve sheath tumor arising from the mesentery near the descending colon in a 60-year-old male. The patient had been under follow-up for neurofibromatosis type 1. He underwent CT to explore the cause of his stomachache, and bowel intussusception caused by a submucosal tumor of the descending colon was suspected. Figures (a–c) represent a coronal MIP of the 18F-FDG PET, axial unenhanced CT, and axial fused PET/CT image of the preoperative 18F-FDG PET/CT, respectively. Although the presenting portion of bowel intussusception did not show elevated FDG uptake (arrows in b and c), nodular FDG uptake in the center of mesentery was detected (arrowheads in a and c). These two lesions were surgically excised and diagnosed as malignant peripheral nerve sheath tumor arising from the mesentery near the descending colon and a lymph node metastasis. Metastatic lymph node showed higher FDG uptake than primary lesion and could be clearly detected in PET/CT
Schwannomas show various level of FDG uptake, even though they are benign tumors [31]. In most cases, they are solitary and unassociated with NF1. Solitary retroperitoneal schwannoma showing high FDG uptake may be confused with malignant tumors [32, 33]. Benz et al. reported that MPNSTs and schwannomas are less reliably distinguished as compared to MPNSTs and neurofibromas [30].
50.6 Pitfalls of 18F-FDG PET for the Diagnosis of Mesenteric and Retroperitoneal Tumors
Some benign diseases may show false-positive FDG uptake because of the elevated FDG uptake.
Desmoid tumors are rare, locally aggressive masses resulting from a benign proliferation of fibrous tissue [34]. Some previous reports have shown elevated FDG uptake in abdominal desmoid tumors, which may therefore be confused for malignant tumors [35, 36]. However, utilizing this same property, Kasper et al. have suggested that the effects of imatinib treatment in patients with desmoid tumors can be evaluated by 18F-FDG PET [37].
Mesenteric panniculitis is an acute benign fibrosing and inflammatory condition involving the adipose tissue of the mesentery. It may be misdiagnosed as a malignant tumor because of FDG uptake resulting from the active inflammatory state [38]. On the other hand, Zissin et al. examined the 18F-FDG PET/CT findings of 19 patients with known malignancy and incidental findings of mesenteric panniculitis and concluded that increased FDG uptake may suggest the coexistence of metastatic deposits, particularly in patients with lymphoma [39].
Retroperitoneal fibrosis is a chronic inflammatory disease, characterized by the presence of fibro-inflammatory tissue, typically surrounding the abdominal aorta and iliac arteries. 18F-FDG PET is valuable for monitoring the disease activity or detecting recurrent inflammation in these cases, because the 18F-FDG uptake has been shown to be correlated with the levels of inflammatory markers such as C-reactive protein and erythrocyte sedimentation rate [40]. On the other hand, elevated 18F-FDG uptake in active inflammatory states may lead to misdiagnosis of the lesions as retroperitoneal malignant tumors [41]. Recently, retroperitoneal fibrosis has been recognized as a manifestation, at least in some cases, of IgG4-related sclerosing disease [42]. 18F-FDG PET is often useful for evaluation of the systemic involvement in cases of IgG4-related sclerosing disease such as autoimmune pancreatitis, Mikulicz disease, and lymph node involvement (Fig. 50.5).
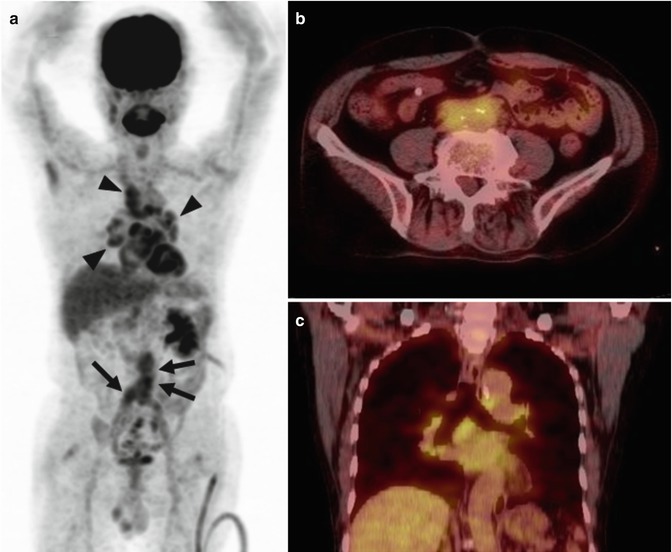
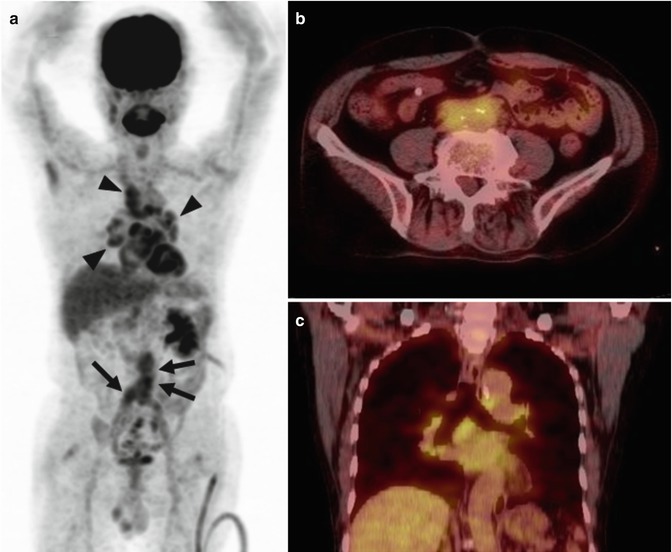
Fig. 50.5
Retroperitoneal fibrosis in a 74-year-old male. The patient had already been diagnosed as having retroperitoneal fibrosis at another hospital. He underwent 18F-FDG PET/CT for the assessment of a small lung nodule. Figures (a–c) represent a coronal MIP of the 18F-FDG PET, axial fused PET/CT image at the level of distal abdominal aorta, and coronal fused PET/CT image, respectively. FDG uptake, probably related to active inflammation, was observed in the fibrotic tissues surrounding the abdominal aorta (arrows on a and also depicted on b). Furthermore, the mediastinal and bilateral hilar lymph nodes also showed elevated FDG uptake (arrowheads in a and also identified on c). Although reactive changes associated with IgG4-related sclerosing disease or sarcoidosis were considered as differential diagnoses, no further examination, such as biopsy, was conducted because he did not have any symptoms
50.7 Other Functional Imaging Techniques
There is scarce experience with functional MRI or CT perfusion in the evaluation of mesenteric and retroperitoneal tumors. Between them, diffusion-weighted imaging (DWI) has shown its capability to distinguish lymphoma and benign and malignant retroperitoneal masses (Fig. 50.6). In the series by Nakayama and colleagues, the apparent diffusion coefficient (ADC) value of malignant lymphoma was significantly lower than that of malignant mesenchymal lesions and benign ones (Fig. 50.7) [44




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree