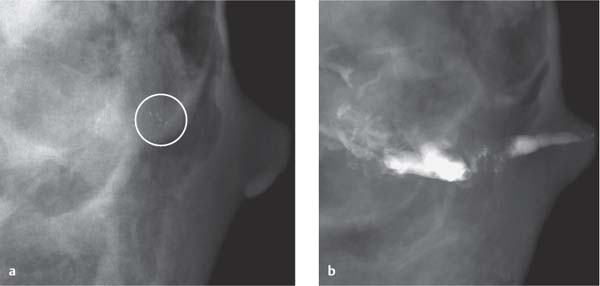
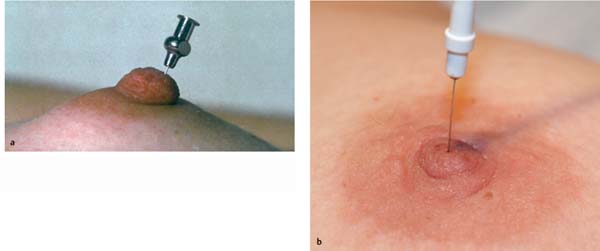
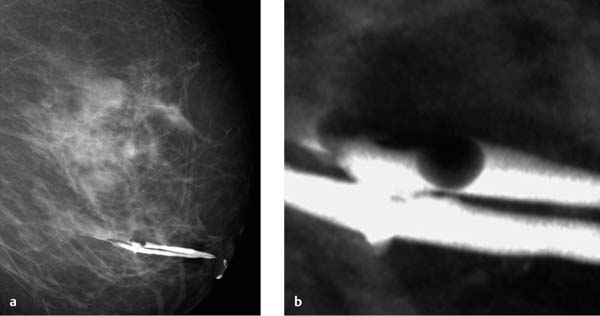
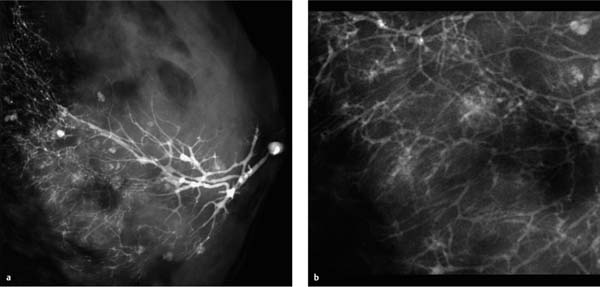
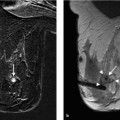
10 Galactography, MR Galactography, Ductoscopy Galactography, or ductography, is a mammographic technique for visualization of a mammary duct and its segmental branches by injecting a water-soluble contrast agent into the milk duct. Galactography is usually performed as part of the evaluation of a uni-lateral spontaneous bloody nipple discharge to determine the size, extent, and localization of an intraductal proliferation. It is not usually possible, however, to differentiate between malignant and benign galactographic findings. The sensitivity of galactography is approx. 70 to 85%, the specificity however, is only 40 to 60%. Preparation and materials. Before galactography is performed, at least one recent mammographic image of the ipsilateral breast should be made available to ensure that if intraductal microcalcifications are present, these are not overlooked because of super-imposition by the contrast material (Fig. 10.1). It is also recommended that secretion be obtained for cytologic analysis before performing the procedure. Galactography is usually performed with the patient in the supine position. Special blunt-tipped galactography needles may be used to cannulate the appropriate duct orifice. Alternatively, lymphography or sialography (30-gauge) needles may be used (Fig. 10.2). Some work groups prefer using a right-angle bent cannula (e. g., Jabczenski end-port, right-angle cannula). Tips and Tricks Before inserting the cannula into the milk duct, the needle system must be flushed with contrast material to avoid the introduction of air bubbles, which could be mistaken for filling defects caused by proliferative lesions on galactography (Fig. 10.3). Cannulation. After disinfection of the nipple, the secreting milk duct must be identified and is best visualized using a bright light and magnifying glasses (magnification factor 3×–5×). Possible incrustations on the papillary surface of the nipple should be carefully removed using a moist pad or disinfection swab. To locate the correct duct, only a minimal amount of fluid must be discharged from the nipple. The cannula is then inserted into the duct using mild pressure. Once the needle has passed beyond the sphincter of the orifice, it will normally advance easily without further resistance unless the duct’s course has a sharp retromammillary deflection, or a retromammillary tumor is present. Contrary to some reports in the literature, dilation of the duct opening before galactography is definitely superfluous. Rash probing and/or antegrade cannulation using strong pressure is painful and can quickly lead to traumatization of the nipple surface or to injury and paraductal administration of contrast material. Contrast administration. After correct cannulation of the appropriate milk duct, water-soluble contrast material is injected using mild pressure. Normally, only 0.5–1 mL is administered. Reports in the literature of administration of 3 mL and more pertain to cases with pronounced duct ectasia. Oil-containing contrast agents are generally no longer used. When the patient reports of a mild feeling of pressure in the breast, contrast injection is terminated and the needle removed from the duct while slightly pulling the nipple ventrally. The duct orifice is then closed using a liquid bandage spray. Any contrast material that has been expelled from the duct should be carefully removed from the skin surface before performing the galactography images. Some work groups prefer to tape the cannula in place before the image is taken. While moving from the examination table to the mammography unit, the patient should support the underside of the examined breast with the contralateral hand to avoid expression of the contrast material. Fig. 10.1a,b Masking of microcalcifications by intraductal contrast material in galactography. Mammography performed before galactography shows a retromammillary cluster of microcalcifications (circle) (a). Microcalcifications are masked by intraductal contrast material injected for galactography (b). Fig. 10.2a,b Insertion of a needle into a secreting duct for galactography. Lymphography needle (a). Sialography needle (b). Fig. 10.3a,b Air bubble artifact in galactogram. Two straight, communicating ducts of normal caliber in galactogram. Round, well-defined filling defect in one duct correlates with an air bubble introduced when contrast was injected (a, b). Magnified partial view (b). X-ray images. Galactography is a mammography examination in two orthogonal planes (craniocaudal [CC] and mediolateral [ML]) performed after injection of contrast material into the secreting milk duct. Breast compression should not be too firm to avoid expression of contrast material before the images have been completed. Once the images have been acquired, however, the nipple can be wiped clean of the spray bandage with a moist pad, and most of the contrast material is expressed by gently massaging the appropriate breast segment from the periphery toward the nipple. Pathologic secretion. Statements in the literature pertaining to the appropriate indications for performing galactography are inconsistent. Some work groups consider the secretion from a single milk duct to be an indication. Others perform a galactography only when the discharge is bloody (Fig. 10.4). Nevertheless, most agree that galactography is indicated in a patient with a spontaneous, pathologic secretion from one milk duct. In general, a pathologic secretion is considered to be bloody. A bloody secretion can be verified either by cytologic examination, or more quickly by gently touching a urine test strip to the expressed discharge. A secretion is always considered pathologic, however, when cytology reveals cells with atypia or carcinoma. A milky secretion, which is usually bilateral and discharged from multiple ducts, is not a pathologic secretion. Outside of the lactational period, however, one should consider hyperprolactemia as a possible cause. Note that the manual provocation of breast secretion is no longer part of the routine clinical breast examination. By squeezing the nipple, it is often possible to obtain a secretion from many women’s breasts. Fig. 10.4a–d Clinical appearance of breast secretions. Watery discharge from one duct (a). Green and yellowish discharge from several ducts (b). Pathologic secretions from one milk duct: fresh bloody discharge (c), older, brownish bloody discharge (d). Fig. 10.5a, b Normal galactography findings. Normal galactogram showing a milk duct and it’s branches from the nipple to the chest wall (a). Contrast material is also seen in paraductal cysts. Magnified partial view (b). The written galactography report should include information on the number of cannulated milk ducts, the amount of injected contrast material, and whether complications (description) occurred. Galactographic findings include Consequences.
Galactography
Technique
Indications
The Written Report and Evaluation Criteria
 a normal duct system
a normal duct system
 duct ectasia (found in approx. 50% of cases, usually without clinical significance)
duct ectasia (found in approx. 50% of cases, usually without clinical significance)
 a filling defect
a filling defect
 duct truncation
duct truncation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree