Gallbladder Carcinoma
Todd M. Blodgett, MD
Alex Ryan, MD
Hesham Amr, MD
Key Facts
Imaging Findings
GB mass with intense uptake often invading into liver
FDG PET for evaluation of localized or metastatic GBC
Also for staging and restaging malignant tumors leading to detection of unsuspected mets in 25-30% and leading to major changes in therapy in 15-20% of cases
CECT can demonstrate tumor extension outside GB and identify metastatic disease in the abdomen and pelvis
Intense FDG uptake in the primary GB mass often directly extends into liver
Abnormal uptake along bile ducts with subserosal and regional lymph node invasion
PET often reveals disease in nonenlarged lymph nodes
Distant hematogenous metastasis and peritoneal seeding may occur
Top Differential Diagnoses
Cholecystitis
Cholangiocarcinoma
Metastases
Gallbladder Polyp
Benign polyps in 4-6% of the general population; most show no radiotracer uptake
Diagnostic Checklist
Pitfall: Misregistered normal bowel activity onto liver or GB can be misleading without CT correlation for presence of mass lesions
TERMINOLOGY
Abbreviations and Synonyms
Gallbladder (GB), gallbladder cancer (GBC)
Definitions
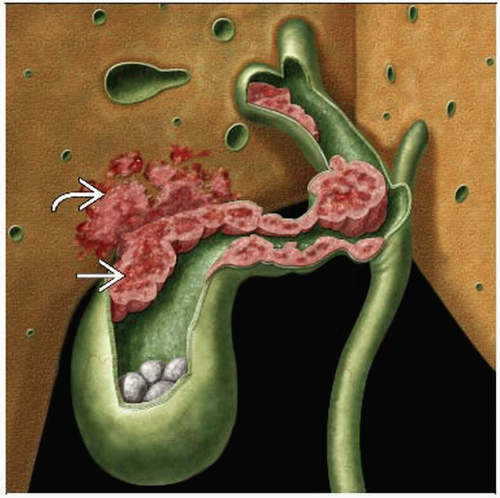
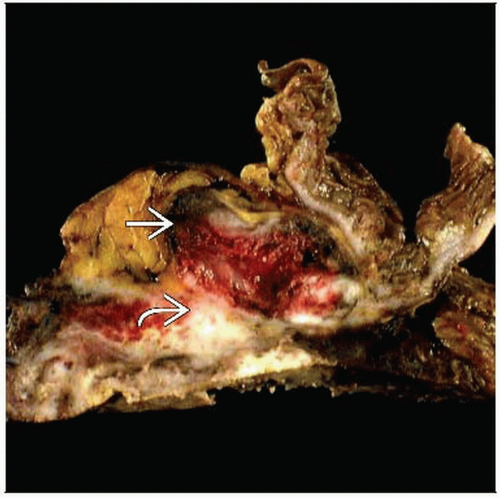
Malignant neoplasm arising from epithelial layer of the gallbladder mucosa
IMAGING FINDINGS
General Features
Best diagnostic clue: FDG-avid mass of the gallbladder with invasion of liver
Location
Most common site of recurrence is laparoscopic port incision
Most frequent sites of lymph node invasion are pericholedocal and cystic
Size
Variable, but usually large at diagnosis
Can be polypoid lesion if detected incidentally on CT
Morphology
Early disease presents as diffuse wall thickening or polyp
Rarely seen, as disease frequently presents in advanced stages
Advanced disease usually appears as large mass with signs of infiltration
Imaging Recommendations
Best imaging tool
Ultrasound
Mass within the gallbladder or focal thickening of the gallbladder wall
Endoscopic retrograde cholangiopancreatography (ERCP)
Obtain tissue sample for histologic diagnosis
Localize obstruction in jaundiced patients
Stent placement in the case of obstruction
CT/MR
Delineation of local invasion and metastatic disease, particularly in relation to vascular structures
FDG PET
Protocol advice
Use contrast-enhanced CT when possible for patients with suspected or known GB malignancy
FDG PET protocol
≥ 6 hour fast prior to scan
Patient with serum glucose ≥ 200 mg/dl should be rescheduled
Avoid exercise or cold temperatures prior to scan
Administer 370-555 MB (10-15 mCi) F-18 FDG IV 1-2 hours before scan
Scan with arms above head
Post-operative patients should be given 4-6 weeks to resolve inflammation prior to scan
CT Findings
Mass and thickening
Mass form is more common due to late diagnosis of most cases
Heterogeneous
Hyperdense areas due to necrosis
Hypovascular, poorly enhancing mass infiltrating GB fossa
Often direct extension to liver along main lobar fissure
Common duct invasion and periportal adenopathy present as hazy density around duct
Early disease presents as wall thickening
Focal and irregular
Disease may originate at site of chronic cholecystitis
Sometimes indistinguishable from inflammatory conditions
Evidence for neoplasm includes hyperemia of thick inner layer that is iso- or hyperattenuating to liver in portal phase
Gallstones
Association with porcelain gallbladder unclear, but its presence is frequently reported
Calcific gallstones present in 65-75% of patients with GBC
Less than 1% of patients with gallstones develop GBC
Staging
CT limited in staging the following entities
Nonenlarged malignant lymph nodes
Distant lymph nodes
Small liver metastases
Peritoneal seeding
Early vs. benign lesions
Invasion of liver and porta hepatis common
Whole body scanning important for detection of distant lung and bone metastases
Intraperitoneal metastasis and carcinomatosis indicate advanced disease
Lymph nodes
CECT may reveal lymphadenopathy in the porta hepatis
Involved lymph nodes appear ring-shaped with heterogeneous contrast enhancement
Metastasis to peripancreatic lymph nodes easily confused for pancreatic carcinoma
Nuclear Medicine Findings
FDG PET and PET/CT
Initial diagnosis
FDG PET has limited role in initial diagnosis because most GBC is diagnosed incidentally within the gallbladder after cholecystectomy
Tumor masses show peripheral uptake with areas of low uptake when there is necrosis
Uptake in primary mass may be seen to extend into liver in the presence of hepatic invasion
Mucinous tumors often demonstrate low FDG avidity
Staging
According to one study, typical SUV of metastatic disease ranges from 2.7-7.5
FDG PET often detects distant disease unsuspected on CT alone, particularly in nonenlarged lymph nodes
Major weakness of FDG PET alone is poor sensitivity for carcinomatosis
Metastasis tends to show increased radiotracer uptake
Combined-modality PET/CT superior to CECT for detection of metastasis
Low sensitivity for regional lymph node detection (vs. 24-40% sensitivity with CECT)
Regional and subserosal lymph node invasion may appear as abnormal uptake along bile ducts
Restaging
Most important contribution of FDG PET and PET/CT is identification of recurrent and metastatic disease
Interpretation of residual tumor in gallbladder fossa following cholecystectomy can be obscured by post-surgical inflammation
Sensitivity and specificity for recurrent disease approximately 80% and 80%
Response to therapy
FDG PET has been used for determination of therapy response, although there is a paucity of studies in the current literature
DIFFERENTIAL DIAGNOSIS
Cholecystitis
Acute cholecystitis
Intense FDG uptake
Must be differentiated clinically from malignancy
Ring-like appearance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree