Abstract
This chapter contains information on the common nuclear medicine gastrointestinal imaging techniques. These include liver-spleen colloid imaging, blood pool agents, localization of ectopic gastric mucosa, hepatobiliary function, and gastrointestinal motility.
Keywords
technetium sulfur colloid, hepatoma, gastrointestinal bleeding, hepatobiliary imaging, cholecystitis, Meckel diverticulum, gastrointestinal motility
Liver-Spleen Imaging
Computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound offer better anatomic display of liver and spleen architecture than does radionuclide liver-spleen imaging, which is rarely performed. However, there remain a few indications for technetium-99m ( 99m Tc) colloid liver-spleen scans, such as the confirmation or evaluation of suspected hepatocellular diseases, hepatomegaly or splenomegaly, and the confirmation of specific space-occupying lesions such as hepatic focal nodular hyperplasia. Although this section is primarily directed toward these applications, as with the interpretation of any examination, it is prudent to have an understanding of other important entities that may be present incidentally, as well as their scintigraphic appearance.
Radiopharmaceuticals
The liver and spleen are organs of widely differing functions, but radionuclide colloid imaging capitalizes on a function common to both: phagocytosis. The most commonly used agent is 99m Tc-sulfur colloid, with an average particle size of 0.3 to 1.0 µm, which is larger than a true colloid. The uptake and distribution of 99m Tc colloid in the liver reflect both the distribution of functioning reticuloendothelial cells and the distribution of hepatic perfusion. In normal patients, most particles are rapidly accumulated by the phagocytes of the reticuloendothelial system of both the liver (Kupffer cells) and the spleen, allowing simultaneous imaging of both organs. Technetium colloid agents are cleared from the bloodstream with a half-time of 2 to 3 minutes. Under usual circumstances, 80% to 90% of the injected particles are sequestered by the liver, and 5% to 10% localize in the spleen. A small percentage of particles appears in other reticuloendothelial sites, particularly the bone marrow, but usually in amounts insufficient to permit imaging. In theory, there is some correlation between particle size and organ avidity for colloid: the larger particles are favored by the spleen, smaller particles go to the liver, and the smallest particles are sequestered by the bone marrow. As discussed later, visualization of uptake in the bone marrow on a technically satisfactory colloid liver-spleen scan is an abnormal finding. However, when amounts of 99m Tc colloid significantly higher than the usual liver-spleen scanning dose are used, routine bone marrow imaging is possible.
Planar Imaging and SPECT/CT
Sample imaging protocols for both planar and single-photon emission computed tomography (SPECT) imaging techniques, as well as dosimetry, are presented in Appendix E .
Imaging is performed using 4 to 6 mCi (148 to 222 MBq) of 99m Tc-sulfur colloid. Adequate accumulation of 99m Tc-sulfur colloid in the liver requires about 5 to 10 minutes in normal patients. This allows for an optimal target (liver-spleen)-to-background (blood pool) ratio. In patients with compromised hepatic function and/or portal hypertension, optimal liver concentration of the radiopharmaceutical may take considerably longer. In such patients, it is wise to wait 20 to 30 minutes before imaging.
Routine gamma camera images for liver-spleen scanning consist of anterior and posterior views and both lateral views. Each image is obtained for 500- to 1000-k counts by using a low-energy parallel-hole collimator. Various oblique images may be routinely obtained or performed as needed for further evaluation of a suspected abnormality in either organ. One anterior view with a lead marker identifying the right inferior costal margin is usually obtained as well. The marker should be of a known size so that hepatic and splenic measurements may be obtained. SPECT scanning of the liver occasionally adds additional information, although focal areas of decreased activity as a result of normal biliary and vascular structures may make interpretation difficult.
Tomographic imaging using 99m Tc-sulfur colloid requires a fundamental knowledge of cross-sectional anatomy of the liver and spleen as well as of surrounding unimaged structures. Transaxial images are displayed in the conventional CT format along with coronal and sagittal reconstructions. In general, defects thought to represent significant pathology should be seen in at least two orthogonal planes to be described with confidence. SPECT is most frequently used to evaluate known or suspected focal or multifocal space-occupying disease. In this setting, SPECT sensitivity and accuracy of localization have been shown to be superior to planar imaging. SPECT has proved especially useful in 99m Tc red blood cell (RBC) blood pool imaging for suspected liver hemangiomas using the same technical parameters as for 99m Tc-sulfur colloid.
Normal Liver Scan
In the normal liver, there is a homogeneous distribution of 99m Tc-sulfur colloid throughout the organ. The liver usually consists of a dominant right and a smaller left lobe ( Fig. 7.1 ), which may occasionally be absent. Numerous variant liver shapes have been described, the most notable of which are a long, thin right lobe (Riedel lobe) and a prominent quadrate lobe. The porta hepatis is frequently identifiable as an area of decreased activity in the inferomedial aspect of the right lobe; this should not be mistaken for a lesion. Peripheral marginal indentations in the liver may normally be produced by the lateral rib margins, the xiphoid, the gallbladder, the right kidney, the suprahepatic veins, the heart, and intrathoracic abnormalities that affect the diaphragmatic configuration. A right lobe defect is commonly seen in many anterior views, owing to attenuation of the photons by overlying breast tissue. Activity seen in the bowel should raise the suspicion of residual activity from another type of recent nuclear medicine study ( Fig. 7.2 ).


Normal length of the right lobe of the liver is generally 17 to 18 cm on the anterior view, measured from the highest point to the inferior tip of the right lobe. Evaluation of a liver-spleen scan should include (1) the size, shape, and position of the liver and spleen; (2) the homogeneity of activity within the organs; (3) the presence of any focal defects in activity; and (4) the relative distribution of colloid among the liver, spleen, and bone marrow.
Abnormal Liver Scan
Any localized space-occupying process in the liver may present as a focal area of decreased activity (commonly referred to as a defect ) on a technetium colloid scan, provided that it is of sufficient size to be detected. Radionuclide imaging simply confirms the presence or anatomic location of focal lesions in the liver rather than providing a definitive histologic diagnosis. The size and location of a lesion are of paramount importance in determining whether it will be detected by gamma camera techniques. By using present technology, lesions as small as 8 mm may be identified. The nearer these lesions are to the surface of the organ, and therefore to the camera collimator surface, the more readily they may be detected.
Defects in the hepatic parenchyma are nonspecific. Solitary intrahepatic defects may be produced by various lesions, any of which may also be multiple ( Box 7.1 and Table 7.1 ). In any patient with several liver defects, however, metastatic disease must be a prime consideration, particularly when accompanied by hepatomegaly or a known primary lesion. In most instances, particularly in cases of equivocal liver scan findings, ultrasonography, CT, or MRI should be performed. A large area of decreased activity in the liver may be produced by the inclusion of part of that organ in a radiation therapy portal. This type of defect, however, is usually readily recognized by its sharp linear edges, which correspond to the sides of the treatment portal. In addition to primarily intrahepatic lesions, peripheral defects in the liver are frequently produced by adjacent extraparenchymal pathology, including subdiaphragmatic fluid accumulations or renal tumors, or by peripheral lesions of a primary hepatic origin, including subcapsular hematoma.
Decreased Uptake
Metastasis (especially colon)
Cyst
Hepatoma (especially in cirrhosis)
Adenoma
Hematoma
Hemangioma
Abscess
Pseudotumor (cirrhosis)
Increased Uptake
Focal nodular hyperplasia
Cirrhosis with regenerating nodule
Budd-Chiari syndrome (caudate lobe)
Superior vena caval obstruction (arm injection, quadrate lobe)
| Lesions | Appearance |
|---|---|
| Hepatic adenoma | Usually photopenic defect |
| Rarely normal activity | |
| 99m Tc RBCs—normal | |
| 99m Tc hepatobiliary: | |
| Perfusion—normal | |
| Parenchymal—decreased | |
| Washout—delayed | |
| Focal nodular hyperplasia | 30% photopenic defect |
| 30% normal activity | |
| 40% increased activity | |
| 99m Tc hepatobiliary: | |
| Perfusion—increased | |
| Parenchymal—normal | |
| Washout—delayed | |
| Cavernous hemangioma | Photopenic defect |
| 99m Tc RBCs: | |
| Perfusion—decreased | |
| Blood pool—increased | |
| Hepatocellular carcinoma | Photopenic defect |
| 67 Ga—avidly increased | |
| 99m Tc RBCs—rarely increased | |
| 99m Tc hepatobiliary: | |
| Perfusion—decreased | |
| Parenchymal—normal or decreased | |
| Washout—delayed | |
| Cholangiocarcinoma | Photopenic defect |
| Metastases | Photopenic defect, early hyperperfusion |
| Liver abscess | Photopenic defect |
| 67 Ga—80% increased | |
| Focal fatty infiltration | Photopenic defect |
| 133 Xe—increased |
67 Ga , Gallium-67; RBCs , red blood cells; 99m Tc , technetium-99m; 133 Xe , xenon-133.
Increased radiocolloid concentration by the spleen and bone marrow compared with the liver (colloid shift) may be found in patients with diseases that cause derangement of hepatic function and/or portal hypertension. Among diffuse hepatocellular diseases, hepatic cirrhosis is the most common abnormality presenting in this fashion. Colloid shift from a dysfunctional liver to the spleen and bone marrow accompanied by other typical scintigraphic findings is a hallmark of this disease. Even patients with diffuse hepatic metastases may show colloid shift.
Other abnormal distributions of colloid include activity in renal transplants, diffuse lung activity, and focal hot spots in the liver ( Box 7.1 ). Diffuse pulmonary activity may be noted occasionally in cirrhosis, infection, and many other entities ( Box 7.2 ). In the presence of superior vena cava or innominate venous obstruction, a bolus of activity injected into an ipsilateral arm vein can travel via the collaterals to a recanalized umbilical vessel, delivering a large amount of activity to the anterior mid-portion of the liver (quadrate lobe), which causes a focal hot spot. Other entities that may cause apparent focal areas of increased hepatic activity are Budd-Chiari syndrome (hepatic vein obstruction), focal nodular hyperplasia, and cirrhosis (regenerating nodules).
Hepatic cirrhosis
Chronic obstructive pulmonary disease with superimposed infection
Bacterial endotoxin
Estrogen therapy
Neoplasms (various primary tumors and metastases, including hepatoma)
Disseminated intravascular coagulopathy
Mucopolysaccharidosis type II (Hunter syndrome)
Histiocytosis X
Faulty colloid preparation (excess aluminum)
High serum aluminum level (antacids)
Children (normal minimal uptake)
Transplant recipients (especially liver and bone marrow)
Pulmonary trauma
Hepatic Cirrhosis
A spectrum of technetium colloid scan findings is presented by hepatic cirrhosis. In its early phases, alcoholic hepatitis or fatty infiltration may present as a normal-sized or enlarged liver with diffusely diminished or inhomogeneous activity. As the disease progresses and parenchymal scarring becomes more prevalent, the liver may become smaller than normal. An oddity of this disease is that the right lobe is frequently more affected, giving a typical pattern of a small right lobe and a relatively enlarged left lobe. This probably occurs because the portal vein delivers more blood flow (and alcohol) to the right lobe of the liver.
Fatty infiltration of the liver may be focal or diffuse. Focal fatty infiltration is seen on CT as an area of low attenuation and can be confused with a neoplastic process. Usually, it can be differentiated from a true mass on CT by noting that there is no mass effect and that portal vessels run through the low-density area. If a technetium colloid scan is performed, the area typically shows normal reticuloendothelial activity. Fatty infiltration can also be noted as an incidental finding on a xenon ventilation lung scan by noting xenon retention in the liver, either focally or diffusely.
As the process of injury, scarring, and regeneration continues, activity within the organ becomes less homogeneous and is sometimes so coarsely mottled as to be confused with space-occupying lesions. In cirrhotic patients with this mottled pattern or with a large dominant defect, especially those who have demonstrated sudden unexplained clinical decompensation, superimposed hepatoma must be considered.
Colloid shift to the spleen and bone marrow is another prominent feature of all phases of hepatic cirrhosis. When hepatocyte function is severely depressed, persistence of technetium colloid in the blood pool may also be identified on static images, especially in the cardiac area. In the advanced stages of disease, the spleen is frequently enlarged, a finding that may correlate with portal hypertension. In some patients, ascites may be imaged on the anterior view as medial displacement of the right lobe of the liver from the ribs and lateral abdominal wall ( Fig. 7.3 ).

Diffuse and Infiltrative Disorders
Any disease that secondarily invades the liver may produce a pattern of hepatomegaly, with or without focal defects and commonly with diffusely diminished activity. Disease entities that may produce this pattern are listed in Box 7.3 . Hepatitis may present in this manner, reflecting diffuse parenchymal edema. If hepatic function is compromised, colloid shift may also be seen.
Normal variant (i.e., large patient with soft-tissue attenuation)
Diffuse hepatocellular disease (e.g., hepatitis)
Metastases
Diabetes mellitus
Fatty infiltration
Hemochromatosis
Amyloidosis
Lymphoma
Leukemia
Sarcoidosis
Lipid storage disorders
Passive congestion
Metastatic Disease
CT or MRI is the initial test of choice if a hepatic tumor or metastasis is suspected. Radionuclide liver-spleen scanning usually detects these as serendipitous findings when the examination is performed for some other reason. Applications of tumor-specific radiopharmaceuticals are discussed in Chapters 10 and 11 . The most characteristic presentation of liver metastasis on a technetium colloid scan is as multiple focal defects, although the lesions may present as coarsely inhomogeneous activity or simply as hepatomegaly.
Primary Liver Neoplasms
Hepatoma
Hepatoma usually presents as a focal defect on sulfur colloid images ( Fig. 7.4 ), although uncommon multifocal forms exist. The lesions frequently occur in association with preexisting diffuse hepatic diseases, most notably alcoholic or postnecrotic cirrhosis. The appearance of a prominent localized colloid deficit in a patient with one of these associations should alert the physician to the possibility of hepatoma. Hepatomas are also noted to be generally gallium-67 avid and with variable fluorodeoxyglucose activity. Therapy for hepatoma may involve direct infusion of chemotherapeutic or embolic agents into the hepatic artery. Evaluation of the catheter placement and distribution of blood flow can be done either with contrast angiography or by administration of 1 to 4 mCi (37 to 148 MBq) of 99m Tc macroaggregated albumin (MAA) (not colloid). The MAA lodges in the capillaries served by the catheter.

Focal Nodular Hyperplasia
The benign neoplasm of focal nodular hyperplasia generally occurs as an asymptomatic mass or as a serendipitously discovered lesion found predominantly in women. The lesions are unique because they contain adequate numbers of Kupffer cells so that they normally concentrate and occasionally hyperconcentrate radiocolloid. Thus in many cases, they appear indistinguishable from normal hepatic parenchyma ( Fig. 7.5 ); sometimes, they present as regions of increased activity on liver scans (these latter lesions do not require biopsy). When lesions discovered by other imaging modalities are of sufficient size to be detected by liver scintigraphy but appear normal on the liver scan, the diagnosis of focal nodular hyperplasia may be presumed in the proper clinical setting. About one-third of the lesions have decreased activity, and when this occurs, the mass cannot be differentiated from other causes of parenchymal defects.

Hepatic Cell Adenomas
Hepatic cell adenomas are usually encountered in young women who have used oral contraceptives (birth control pills). Although the disease usually is asymptomatic, hemorrhage, often of massive degree, occasionally occurs. Because Kupffer cells are not a prominent feature of these lesions, adenomas present as focal defects on technetium colloid images. Adenomas are also photopenic on hepatobiliary and RBC scans.
Miscellaneous Focal Lesions
Abscess
Abscess commonly presents as a nonspecific solitary focal defect on liver scans, although multiple lesions may occur. The diagnosis is frequently suggested by history.
Budd-Chiari Syndrome (Hepatic Vein Thrombosis)
Hepatic vein thrombosis may occur secondary to tumor invasion or hypercoagulation syndromes, but frequently no underlying cause is identified. The disease usually presents as an enlarged, congested tender liver accompanied by ascites. With early or partial hepatic vein obstruction, technetium colloid activity in the liver becomes diffusely mottled. As thrombosis progresses, activity in both lobes steadily decreases. Typically, the caudate lobe simultaneously enlarges and shows relatively increased activity. This latter phenomenon has been explained by the presence of separate venous drainage directly into the vena cava for the caudate lobe, which is unaffected by thrombosis of the major hepatic veins.
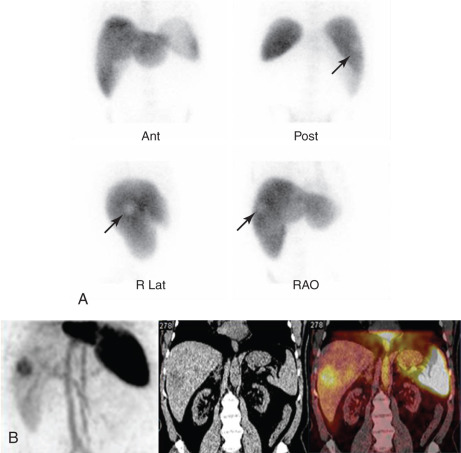
Hepatic Blood Pool Imaging
Although hemangiomas and cysts are usually occult, asymptomatic lesions, ultrasound can reliably distinguish between cysts (which are hypoechoic) and hemangiomas (which are hyperechoic). CT with intravenous contrast is more specific, usually demonstrating characteristic progressive enhancement toward the center of a hemangioma. Cavernous hemangioma is highly likely when a defect seen with 99m Tc-sulfur colloid imaging shows increased activity after administration of a 99m Tc blood pool agent, such as 99m Tc-RBC, owing to labeling of the blood pool in the lesion. To allow equilibration of the hemangioma blood pool with the labeled RBCs, delayed imaging (sometimes over several hours) may be necessary when planar imaging is used. Dynamic or immediate blood flow images frequently show normal or decreased perfusion of the lesions. Use of SPECT or SPECT/CT in the setting of suspected hepatic hemangioma increases the sensitivity of the study, especially when lesions are deep or less than 5 cm in diameter ( Fig. 7.6 ). SPECT provides nearly 100% sensitivity for detection of hemangiomas larger than 1.5 cm in diameter; sensitivity is 50% or less for lesions smaller than 1.0 cm in diameter.
Splenic Imaging
Normal Spleen Scan
On the posterior and anterior views of a technetium colloid scan, the normal spleen exhibits homogeneous activity equal to or less than that of the liver. The organ is ovoid in configuration, with occasional thinning of the anterior aspect. The normal length of the spleen on a posterior scan is about 10 ± 1.5 cm and should not exceed 13 cm. When imaging the spleen with colloid, routine anterior, posterior, and lateral liver-spleen scan views are obtained. Left anterior oblique and left posterior oblique views at varying degrees of obliquity also may be useful. Occasionally a right posterior oblique view may be needed to separate the left lobe of the liver from the spleen. After surgery or trauma, there may be questions about splenic remnants or accessory spleens. Historically, these were imaged with heat-damaged RBCs; however, for most purposes, use of 99m Tc-sulfur colloid is adequate ( Fig. 7.7 ).
Abnormal Spleen Scan
Focal Lesions
Solitary or multiple splenic defects are nonspecific and may be produced by a number of abnormalities. Careful correlation with pertinent clinical history is necessary to distinguish among these. More common abnormalities that may present as defects within the organ are cysts, hematomas, abscesses, infarctions, and neoplasms. Peripheral wedge-shaped defects may often be correlated with infarcts, especially when a pertinent history, such as of hemoglobinopathy, is obtained.
Metastatic lesions to the spleen are uncommon, although tumors such as lymphoma, melanoma, chorioepithelioma, or soft-tissue sarcoma may present with splenic lesions. Primary splenic neoplasms are extremely rare. Focal areas of decreased activity in the spleen occur in less than 1% of liver-spleen scans. If trauma is excluded as a cause, one-third of such defects are due to splenic infarcts, one-third to lymphoma, and one-third to metastatic disease. A history of immunosuppression or drug abuse increases the likelihood of abscess.
Splenomegaly
Liver-spleen scans may be inappropriately ordered to confirm clinical suspicion of splenomegaly, although ultrasound is less expensive and does not use ionizing radiation. The causes of splenomegaly are numerous ( Box 7.4 ), and unless focal space-occupying disease is identified, scans are generally unhelpful in determining the cause. Infiltrative disorders produce varying degrees of splenomegaly, with or without alterations in splenic activity. The findings are largely nonspecific and are best interpreted in light of clinical observations. Perhaps the one exception to this is massive splenomegaly, which is most often caused by chronic lymphocytic leukemia.
Massive Enlargement
Chronic leukemia
Myelofibrosis
Glycogen storage diseases
Thalassemia major
Moderate Enlargement
Cirrhosis with portal hypertension
Hepatitis, acute or chronic
Hemolytic anemia
Mononucleosis
Lymphoma a
a Depending on disease stage, these entities may also cause decreased activity.
Minimal Enlargement
Congestive heart failure
Metastatic disease a
Collagen disease
Infections
Splenic hyperfunction
Portal hypertension
Anemia
Leukemia
Lymphoma a
Sepsis
Melanoma a
Stress (recent surgery or chemotherapy)
Hepatocellular dysfunction (colloid shift)
Trauma
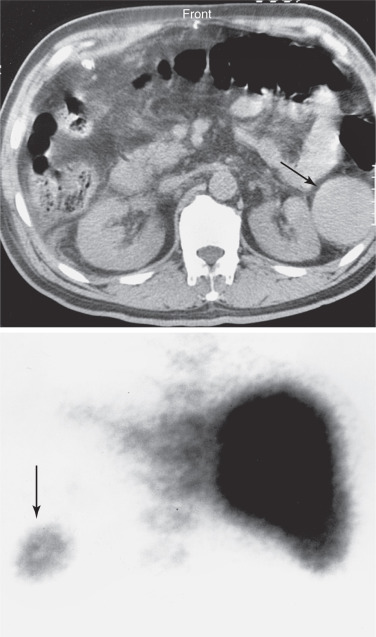
CT is the imaging method of choice for acute splenic trauma. The role of radiocolloid spleen imaging is usually very limited. After abdominal trauma, splenic tissue may seed to other locations (splenosis), such as the lung and peritoneal cavity. Such tissue fragments usually accumulate radiocolloid or heat-damaged 99m Tc-labeled RBCs ( Fig. 7.8 ) and, when correlated with ultrasound or CT imaging, can be substantiated as splenic tissue.

Nonvisualization of the Spleen
In certain cases, the spleen may not be visualized on a 99m Tc colloid scan even in the absence of a history of splenectomy ( Box 7.5 ). Congenital asplenia may be associated with a number of cardiovascular, pulmonary, and abdominal anomalies. In sickle cell anemia, the spleen may not be seen because of atrophy related to repeated infarctions (autosplenectomy); in some of these patients, the spleen remains anatomically intact but with depressed or absent reticuloendothelial function, owing to reversible mechanical obstruction of blood flow by the abnormal configuration of the RBCs (functional asplenia).
Focal Defects
Infarct
Lymphoma
Metastasis
Cyst
Abscess
Hematoma or splenic artery aneurysm
Anatomic variation
Artifact
Nonvisualization
Splenectomy
Sickle cell disease (functional or autosplenectomy)
Congenital absence of spleen (isolated or Ivemark syndrome)
Tumor replacement
Infarction
Traumatic avulsion or volvulus
Functional asplenia
Gastrointestinal Bleeding Studies
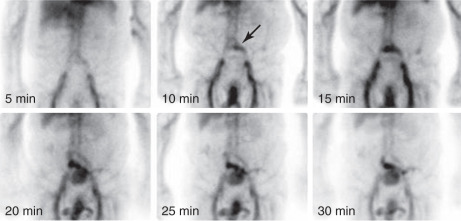
Technetium-99m in vitro labeled RBCs are the radiopharmaceutical of choice in the investigation of gastrointestinal (GI) hemorrhage, especially in cases of intermittent or slow bleeding, with a sensitivity for active bleeding of greater than 90%. Because the agent remains in the intravascular space, imaging may be performed over 24 hours. Any free technetium that is not bound to RBCs is excreted by the kidneys and gastric mucosa and passes into the bladder, small bowel, and colon. This latter problem is mitigated by use of in vitro labeling techniques, which allow for a high degree of RBC tagging and therefore a lower percentage of free technetium. With RBCs, most bleeding sites show an initial focus of activity, which increases and changes position and/or configuration with time. If the activity remains in the same location, static vascular abnormalities, such as an aneurysm or angiodysplasia, should be suspected. When delayed imaging is necessary to identify a bleeding site, there may be uncertainty with respect to the site of origin.
If the extravasated intraluminal agent is not identified shortly after its deposition, it may move to a more proximal or distal site during any prolonged intervals between images, especially with the increased peristalsis present in most patients with GI bleeding. However, establishing the mere presence of slow bleeding into the bowel remains possible, and therefore, the study is undoubtedly of value in many patients. The sensitivity is significantly greater than with angiography for the detection of lower GI bleeding, with the added advantage of being noninvasive. Because of significant background activity in the upper abdomen and the diagnostic efficacy of endoscopy in the GI tract, nuclear imaging techniques are most advantageous in evaluating lower GI bleeding, although active small bowel, duodenal, and distal gastric hemorrhage are routinely detected when proper timing and technique for imaging are used. The accuracy of endoscopy in making the diagnosis of upper GI bleeding exceeds 90%.
The common causes of lower GI bleeding in adults are diverticular disease, angiodysplasia, neoplasms, and inflammatory bowel disease. Preoperative localization of a bleeding site permits a more rational, tailored approach to angiography and surgical intervention. Because bleeding from these causes is frequently intermittent, chances of detecting the site of hemorrhage are enhanced by a radiopharmaceutical with a long intravascular half-life, such as labeled RBCs. Angiography may be negative in patients with intermittent bleeding or bleeding rates below 1.0 mL/min. With radionuclide techniques, bleeding rates on the order of 0.2 mL/min are reliably detected, and the sensitivity has been reported to be good even for bleeding rates as low as 0.04 mL/min, although a total volume of 2 to 3 mL of blood is necessary. These techniques are best applied to patients who are bleeding acutely. Patients with chronic, low-volume blood loss presenting with guaiac-positive stools or chronic anemias seldom benefit from the examination. Details of the technique are presented in Appendix E .
If 99m Tc-RBCs are unavailable or if time does not allow for the labeling procedure, 99m Tc-sulfur colloid has been used as a GI hemorrhage imaging agent, although this is not as accurate.
Interpretation
A positive scan shows a focal site of increased activity within the abdomen or pelvis, which progresses distally in the bowel ( Figs. 7.9 and 7.10 ; Box 7.6 ). Once bleeding is identified, multiple sequential images aid greatly in establishing its origin by recording the pattern of progression of the radionuclide within the bowel. Optimally, the images are viewed in cine mode. Because blood is an irritant to the intestine, movement of activity is often rapid and can be bidirectional. This is often true in the small bowel where a rapid serpiginous course of the labeled RBCs from the left upper abdomen to the right lower quadrant is characteristic. The earlier in a study that the bleeding is seen, the more accurate is the localization. Because the main purpose of the examination is to localize the site of bleeding, the study should be continued for a sufficient length of time to follow the progress of the labeled blood and permit mapping of bowel anatomy, which may vary somewhat from patient to patient. An area of activity that remains fixed in location over time should raise the suspicion of causes other than intraluminal bleeding. Occasional confusion of bladder activity with a rectosigmoid bleed can usually be resolved on postvoid views or lateral pelvic images. Interfering genital activity is usually identified by its location on anterior oblique or lateral pelvic views. Carefully performed labeled RBC studies show a high degree of sensitivity (> 90%), with a low false-negative results rate. In addition to providing evidence of active GI bleeding and its location, the examination may also be used as a guide for selective abdominal arteriography and to assess the results of interventional therapy.