General notes
Radiology
The procedures are laid out under a number of sub-headings, which follow a standard sequence. The general order is outlined below, together with certain points that have been omitted from the discussion of each procedure in order to avoid repetition. Minor deviations from this sequence will be found in the text where this is felt to be more appropriate.
Contraindications
All radiological procedures carry a risk. The risk incurred by undertaking the procedure must be balanced against the benefit to the patient as deduced from the information obtained. Contraindications may be relative (the majority) or absolute. Factors that increase the risk to the patient can be categorized under three headings: due to radiation; due to the contrast medium; due to the technique.
Risk due to radiation
Radiation effects on humans may be:
• hereditary, i.e. revealed in the offspring of the exposed individual, or
• somatic injuries, which fall into two groups: deterministic and stochastic.
1. Deterministic effects result in loss of tissue function, e.g. skin erythema and cataracts. If the radiation dose is distributed over a period of time, cellular mechanisms allow tissue repair. There is then greater tolerance than if the dose had been administered all at once. This implies a threshold dose above which the tissue will exhibit damage because the radiation dose exceeds the capabilities of cellular repair mechanisms.
2. Stochastic effects refer to random modifications to cell components, such as DNA mutations that can occur at any radiation dose; there is no threshold for stochastic effects.1 Stochastic effects, such as malignancy, are ‘all or none’. The cancer produced by a small dose is the same as the cancer produced by a large dose, but the frequency of occurrence is less with the smaller dose.
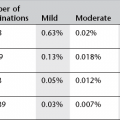
The current consensus held by international radiological protection organizations is that, for comparatively low doses, the risk of both radiation-induced cancer and hereditary disease is assumed to increase linearly with increasing radiation dose, with no threshold (the so-called linear no threshold model).2 It is impossible to totally avoid staff and patient exposure to radiation. The adverse effects of radiation, therefore, cannot be completely eliminated but must be minimized. There is a small but significant excess of cancers following diagnostic levels of irradiation, e.g. during childhood3 and to the female breast4 and amongst those with occupational radiation exposure.5 In the UK about 0.6% of the overall cumulative risk of cancer by the age of 75 years could be attributable to diagnostic X-rays. The most important factors which influence the risk of developing cancer after exposure to ionizing radiation are: (a) genetic considerations – specific gene mutations and family history; (b) age at exposure – children are, in general, more radiosensitive than adults; (c) sex – there is a slightly increased risk in females; (d) fractionation and protraction of exposure – higher dose and dose rate increase risk because of the influence of DNA damage.6 (Typical average effective dose equivalents for some common examinations are given in Appendix I.)
There are legal regulations which guide the use of diagnostic radiation (see Appendices II and III). These are the two basic principles:
1. Justification that a proposed examination is of net benefit to the patient.
2. ALARP – doses should be kept As Low As Reasonably Practicable; economic and social factors being taken into account.7
Justification is particularly important when considering the irradiation of women of reproductive age, because of the risks to the developing fetus. The mammalian embryo and fetus are highly radiosensitive. The potential risks of in utero radiation exposure on a developing fetus include both teratogenic and carcinogenic effects. The risk of each effect depends on the gestational age at the time of the exposure and the absorbed radiation dose. The developing fetus is most vulnerable to radiation effects on the central nervous system between 8 and 15 weeks of gestational age and the risk of development of fatal childhood cancer may be greater if exposure occurs earlier in pregnancy.8 The teratogenic risk of radiation is dose-dependent and exposure to ionizing radiation doses of less than 50 mGy has not been shown to be associated with different pregnancy outcomes compared with exposure to background radiation alone.8 The carcinogenic risk of ionizing radiation is harder to calculate accurately. It is thought that the risk for the general population of developing childhood cancer is 1 in 500.9 For a fetal radiation dose of 30 mGy the best estimate is of one excess cancer per 500 fetuses exposed,10 resulting in a doubling of the natural rate. Most diagnostic radiation procedures will lead to a fetal absorbed dose of less than 1 mGy for imaging beyond the maternal abdomen/pelvis and less than 10 mGy for direct abdominal/pelvic or nuclear medicine imaging. There are important exceptions which result in higher doses, such as CT scanning of the maternal pelvis.
Almost always, if a diagnostic radiology examination is medically indicated, the risk to the mother of not doing the procedure is greater than the risk of potential harm to the fetus. However, whenever possible, alternative investigation techniques not involving ionizing radiation should be considered before a decision to use ionizing radiation in a female of reproductive age is taken. It is extremely important to have a robust process in place that prevents inappropriate or unnecessary ionizing radiation exposure to the fetus. Joint guidance from the Health Protection Agency, the College of Radiographers and the Royal College of Radiologists recommends the following:9
When a female of reproductive age presents for an examination in which the primary beam irradiates the pelvic area, or for a procedure involving radioactive isotopes, she should be asked whether she is or might be pregnant. If the patient cannot exclude the possibility of pregnancy, she should be asked if her menstrual period is overdue. Her answer should be recorded and, depending on the answer, the patient assigned to one of the following four groups:
1. No possibility of pregnancy – proceed with the examination.
2. Patient definitely, or probably, pregnant – review the justification for the proposed examination and decide whether to defer until after delivery, bearing in mind that delaying an essential procedure until later in pregnancy may present a greater risk to the fetus and a procedure of clinical benefit to the mother may also be of indirect benefit to her unborn child. If, after review, a procedure is still considered to be justified and is undertaken the fetal dose should be kept to the minimum consistent with the diagnostic purpose.
3. Low-dose examination, pregnancy cannot be excluded – a low-dose examination is defined as one in which the fetal dose is likely to be below 10 mGy. The vast majority of diagnostic examinations fall into this category. If pregnancy cannot be excluded but the patient’s menstrual period is not overdue, proceed with the examination. If the period is overdue, the patient should be treated as probably pregnant and the advice in the section above followed.
4. High-dose examination, pregnancy cannot be excluded – a high-dose procedure is defined as any examination which results in a fetal dose greater than 10 mGy (e.g. CT of the maternal abdomen and pelvis). The evidence suggests that such procedures may double the natural risk of childhood cancer if carried out after the first 3–4 weeks of pregnancy and may still involve a small risk of cancer induction if carried out in the very early stages of an unrecognized pregnancy. Either of two courses can be adopted to minimize the likelihood of inadvertent exposure of an unrecognized pregnancy: (a) apply the rule that females of childbearing potential are always booked for these examinations during the first 10 days of their menstrual cycle when conception is unlikely to have occurred; or (b) female patients of childbearing potential are booked in the normal way but are not examined and are re-booked if, when they attend, they are in the second half of their menstrual cycle and are of childbearing potential and in whom pregnancy cannot be excluded.
If the examination is necessary, evaluation of the fetal dose and associated risks by a medial physicist should be arranged, if possible, and discussed with the parents. A technique that minimizes the number of views and the absorbed dose per examination should be utilized. However, the quality of the examination should not be reduced to the level where its diagnostic value is impaired. The risk to the patient of an incorrect diagnosis may be greater than the risk of irradiating the fetus. Radiography of areas that are remote from the pelvis and abdomen may be safely performed during pregnancy with good collimation and lead protection. Royal College of Radiologists guidelines indicate that legal responsibility for radiation protection lies with the employer, the extent to which this responsibility is delegated to the individual radiologist varies. Nonetheless, all clinical radiologists carry a responsibility for the protection from unnecessary radiation of:
Risk due to the contrast medium
The risks associated with administration of iodinated contrast media and magnetic resonance imaging (MRI) contrast are discussed in detail in Chapter 2 and guidelines are given for prophylaxis of adverse reactions to intravascular contrast.
Contraindications to other contrast media, e.g. barium, water-soluble contrast media for the gastrointestinal tract and biliary contrast media, are given in the relevant sections.
Contrast medium
Volumes given are for a 70-kg man.
Equipment
For many procedures this will also include a trolley with a sterile upper shelf and a non-sterile lower shelf. Emergency drugs and resuscitation equipment should be readily available (see Chapter 17).
See Chapter 9 for introductory notes on angiography catheters.
If only a simple radiography table and overcouch tube are required, then this information has been omitted from the text.
Patient preparation
1. Will admission to hospital be necessary?
2. If the patient is a woman of child-bearing age, the examination should be performed at a time when the risks to a possible fetus are minimal (see above). Any female presenting for radiography or a nuclear medicine examination at a time when her period is known to be overdue should be considered to be pregnant unless there is information indicating the absence of pregnancy. If her cycle is so irregular that it is difficult to know whether a period has been missed and it is not practicable to defer the examination until menstruation occurs, then a pregnancy test or pelvic ultrasound (US) examination may help to determine whether she is pregnant. Particular care should be taken to perform hysterosalpingography during the first 10 days of the menstrual cycle, so that the risks of mechanical trauma to an early pregnancy are reduced.
3. Except in emergencies, in circumstances when consent cannot be obtained, patient consent to treatment is a legal requirement for medical care.12 Consent should be obtained in a suitable environment and only after appropriate and relevant information has been given to the patient.13 Patient consent may be:
(a) implied consent – for a very low-risk procedure, the patient’s actions at the time of the examination will indicate whether they are content for the procedure to be performed
(b) express consent – for a procedure of intermediate risk, such as barium enema, express consent should be given by the patient, either verbally or in writing
(c) written consent – must be obtained for any procedure that involves significant risk and/or side effects. The ability to consent depends more on a person’s ability to understand and weigh up options than on age. At 16 a young person can be treated as an adult and can be presumed to have the capacity to understand the nature, purpose and possible consequences of the proposed investigation, as well as the consequences of non-investigation. Under the age of 16 years children may have the capacity to consent depending on their maturity and ability to understand what is involved. The radiologist must assess a child’s capacity to decide whether to give consent for, or refuse an investigation. If the child lacks the capacity to consent, the parent’s consent should be sought. It is usually sufficient to have consent from one parent. If the parents cannot agree, legal advice should be obtained.14 When a competent child refuses treatment, a person with parental responsibility or the court may authorize investigations or treatment which is in the child’s best interests. In Scotland the situation is different: parents cannot authorize procedures a competent child has refused. Legal advice may be helpful in dealing with these cases.
4. If an interventional procedure carries a risk of causing bleeding then the patient’s blood clotting should be measured before proceeding. If a bleeding disorder is discovered, or if the patient is being treated with anticoagulant therapy, the appropriate steps should be taken to normalize clotting before performing the procedure.
5. Cleansing bowel preparation may be used prior to investigation of the gastrointestinal tract or when considerable fecal loading obscures other intra-abdominal organs. For other radiological investigations of abdominal organs, bowel preparation is not always necessary, and when given may result in excessive bowel gas. Bowel gas may be reduced if the patient is kept ambulant prior to the examination and those who routinely take laxatives should continue to do so.
6. Previous films and notes should be obtained.
7. Premedication will be necessary for painful procedures or where the patient is unlikely to cooperate for any other reason. Suggested premedication for adults and children is described in Chapter 18.
Preliminary images
The purpose of these films is:
1. to make any final adjustments in exposure factors, centring, collimation and patient position, for which purpose the film should always be taken using the same equipment as will be used for the remainder of the procedure
2. to exclude prohibitive factors such as residual barium from a previous examination or excessive fecal loading
3. to demonstrate, identify and localize opacities which may be obscured by contrast medium
4. to elicit radiological physical signs.
Every radiographic view taken should have on it the patient’s name, registration number, date and a side marker. The examination can only proceed if satisfactory preliminary films have been obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree