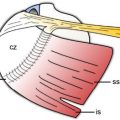
Figure 5-20. GHJ effusion distending the posterior recess. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows the normal recess and articular cartilage (arrowheads) located deep to the infraspinatus (infra). [C] Corresponding 12-5 MHz US image shows GHJ effusion distending the posterior recess (asterisk). Joint effusion tends to collect in the posterior recess due to the thin capsule and the low pressure exerted by the tissues above. [D] Corresponding axial STIR MRI confirms fluid distension of the posterior GHJ recess. Hum= humerus.
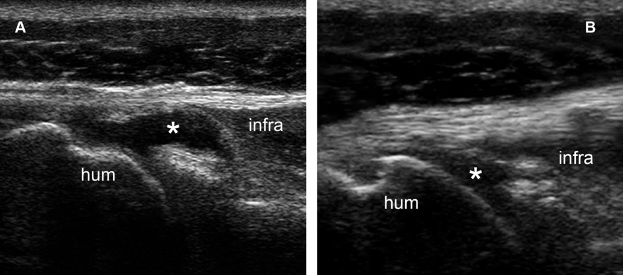
Figure 5-21. GHJ effusion distending the posterior recess. [A] Axial 12-5 MHz US image obtained during external rotation of the shoulder clearly depicts fluid distension of the posterior recess (asterisk). [B] The finding is much less conspicuous with shoulder in neutral position. Infra= infraspinatus. Hum= humerus.
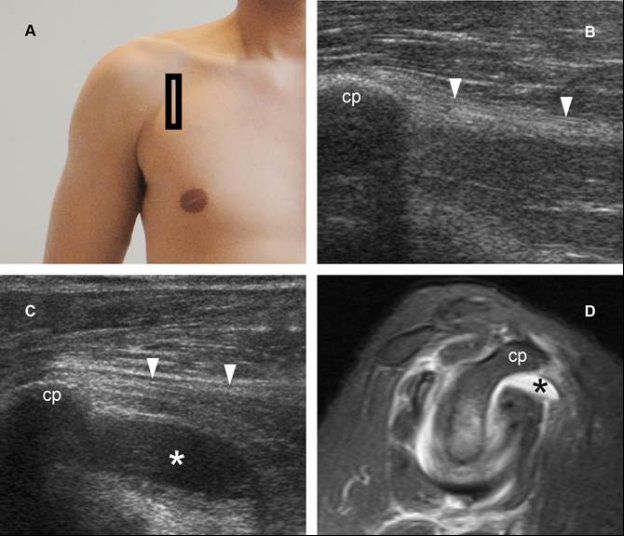
Figure 5-22. GHJ effusion distending the superior subscapularis recess. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image obtained from asymptomatic side shows the expected location of the superior subscapularis recess, deep to the coracoid process (cp) and the conjoined tendon of the short head of the biceps and the coracobrachialis (arrowheads). The superior subscapularis recess is not visible at US in healthy individuals. Because of its deep location, sonographic evaluation may require a lower-frequency curvilinear array probe for adequate assessment. [C] Corresponding 12-5 MHz US image obtained from symptomatic side shows GHJ effusion distending the subscapularis recess (asterisk). [D] Corresponding sagittal STIR MRI confirms fluid distension of the superior subscapularis recess in symptomatic side (black asterisk).
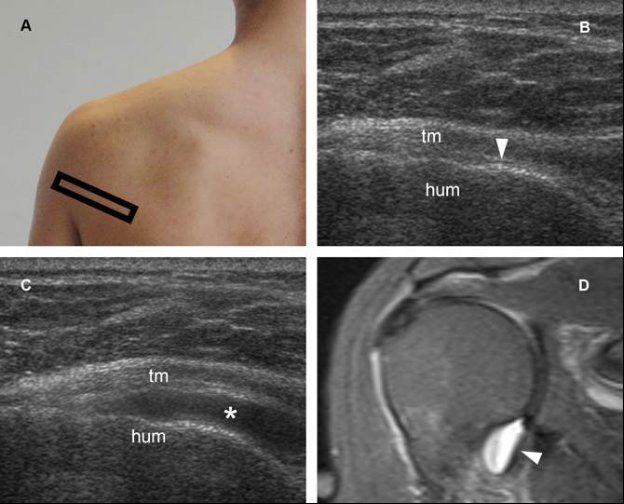
Figure 5-23. GHJ effusion distending the axillary recess. [A] Positioning of the probe. There are two techniques to evaluate the axillary recess: a caudal approach through the axilla and a posterior approach through the teres minor muscle. The latter is our preferred and usually well tolerated by the patient. [B] Corresponding 12-5 MHz US image obtained from asymptomatic side shows the normal recess and articular cartilage (arrowhead) located deep to the teres minor ™. [C] Corresponding 12-5 MHz US image obtained from symptomatic side shows GHJ effusion distending the axillary recess (asterisk). [D] Corresponding coronal oblique STIR MRI confirms fluid distension of the axillary recess in symptomatic side (arrowhead). Hum= humerus.
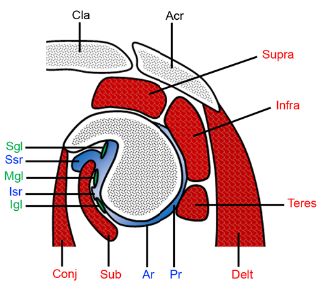
Figure 5-24. GHJ recesses. Schematic drawing of an oblique sagittal view through the glenoid. The superior subscapularis recess (ssr) extends below the coracoid process and above the subscapularis (sub). Sgl= superior glenohumeral ligament. Mgl= middle glenohumeral ligament. Igl= inferior glenohumeral ligament. Isr= inferior subscapularis recess. Ar= axillary recess. Post= posterior recess. Acr= acromion. Cla= clavicle. Conj= conjoined tendon of the short head of the biceps and the coracobrachialis. Delt= deltoid. Supra= supraspinatus. Infra= infraspinatus. Teres= teres minor.
Distinction between joint effusion and synovial proliferation is intuitive when fluid is clear and anechoic, but may be challenging when US depicts hypoechoic or hyperechoic material distending joint recesses (video 5-8).60 Poor compressibility, lack of internal movements during graded compression, and internal flow on Doppler US all suggest synovial proliferation rather than complex fluid. GHJ effusion is mostly associated with rotator cuff tears, while synovial proliferation is usually associated with systemic inflammatory arthropathies (video 5-9). Septic effusion is rare, requires early diagnostic arthrocentesis for optimal outcomes, and is depicted as nonspecific anechoic, hypoechoic, or hyperechoic material distending joint space at US.
2.2.2. Degenerative Joint Disease
Primary GHJ osteoarthritis is extremely rare. Conversely, secondary osteoarthritis is much more prevalent, and usually occurs as the end result of chronic rotator cuff tears. Irish surgeon, Robert Adams is credited as the first to describe the clinical findings of GHJ osteoarthritis secondary to rotator cuff tear in 1857.61 However, it was not until 1977 that Charles Neer coined the term cuff tear arthropathy.62 The diagnosis of cuff tear arthropathy is based on clinical and radiographic findings. US may help suggest the diagnosis when a chronic massive tear of the supraspinatus tendon is demonstrated in conjunction with reduced acromiohumeral distance and rounded greater tuberosity of the humerus (figure 5-25).
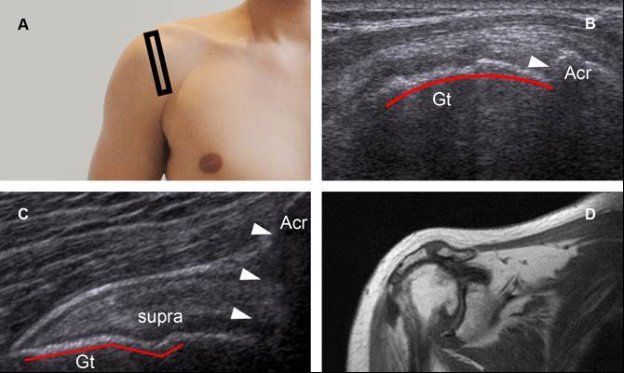
Figure 5-25. Cuff tear arthropathy. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows a massive tear of the supraspinatus tendon, reduced acromiohumeral distance (arrowhead), and rounded greater tuberosity of the humerus (red line). [C] Comparative contralateral image demonstrates normal contour of the proximal humerus (red line), normal acromiohumeral distance (arrowheads), and normal supraspinatus tendon (supra). [D] Corresponding coronal oblique T1-weighted MRI depicts typical findings of cuff tear arthropathy. Gt= greater tuberosity. Acr= acromion.
2.2.3. Chondrocalcinosis
US is not considered a primary diagnostic modality to evaluate glenohumeral cartilage because of shadowing, but a small part of the articular cartilage covering the humeral head can be assessed for abnormalities. US demonstrates normal cartilage as a homogeneously hypo-anechoic structure delimited by thin hyperechoic margin at the interface with the synovial fluid (figure 5-26).
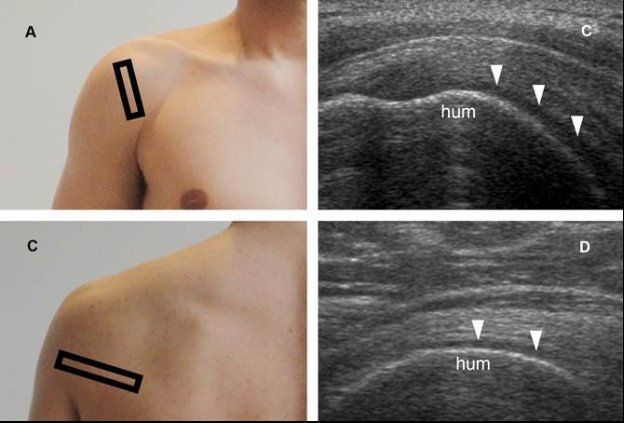
Figure 5-26. Articular cartilage. [A] Positioning of the probe. [B] Corresponding coronal oblique 12-5 MHz US image shows the normal cartilage covering the anterior aspect of the humeral head as a homogeneously hypo-anechoic structure (arrowheads). [C] Positioning of the probe. [D] Corresponding axial 12-5 MHz US image shows the normal cartilage covering the posterior aspect of the humeral head (arrowheads). Hum= humerus.
Chondrocalcinosis (see section 1.2.6) may be depicted as echogenic foci with no acoustic shadow within the hyaline cartilage covering the humeral head (figure 5-27).
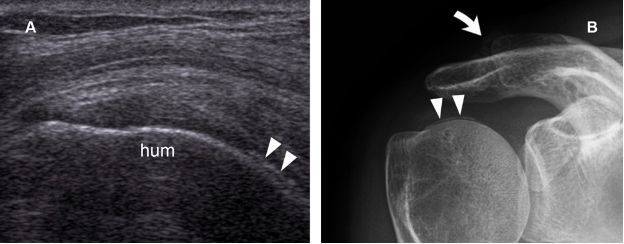
Figure 5-27. GHJ chondrocalcinosis. [A] Coronal oblique 12-5 MHz US image depicts tiny echogenic foci with no acoustic shadow within the cartilage covering the anterior aspect of the humeral head (arrowheads). [B] Corresponding radiography confirms GHJ chondrocalcinosis (arrowheads). Note also ACJ chondrocalcinosis (curved arrow). Hum= humerus.
2.2.4. Joint Instability
GHJ instability occurs when static or dynamic stabilizers become incompetent and involve multiple different diagnoses with a broad range of underlying pathology. Many classification schemes have been developed related to degree (dislocation, subluxation, microinstability), direction (anterior, posterior, multidirectional), etiology (chronic microtrauma, acute trauma, congenital abnormality), and duration of symptoms (acute, chronic, recurrent). A dislocation occurs when humeral head dissociates from the glenoid fossa, while a subluxation is characterized by humeral head translation to the edge of the glenoid, beyond physiological limits, and is followed by selfreduction. Microinstability implies multidirectional hypermobility due to excessive capsular laxity. GHJ instability can also be subclassified into voluntary and involuntary, and some patients with voluntary instability have associated psychological pathology.63
The clinical presentation can range from acute frank dislocation to chronic non-specific shoulder pain. Although US is not indicated to specifically address GHJ instability,64 it may occasionally depict abnormal joint motion during provocative manoeuvers (video 5-10). Acute dislocations are largely produced by trauma and discussed in chapter 6 because of its association with proximal humerus fractures. Glenoid and humeral causes of GHJ instability are also associated to fractures and further discussed in chapter 6. Since rotator cuff tendons are a major component of the dynamic stabilizers of the shoulder, depiction of GHJ instability should prompt a careful scrutiny for rotator cuff tears. In the absence of penetrating trauma or infection, intra-articular gas (see section 1.2.7) is a reliable indicator of recent GHJ distraction (video 5-11).
2.2.5. Loose bodies
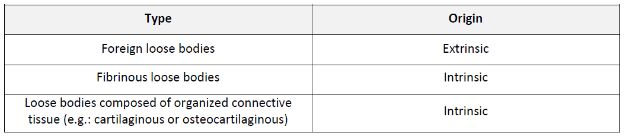
Loose bodies are fragments of solid tissue in a body cavity or joint that are commonly classified according to their composition (table 5-3).65 Loose bodies may also be classified as either stable or unstable. Unstable loose bodies are usually symptomatic because they are freely movable and predisposed to entrapment. Conversely, stable loose bodies are generally well tolerated by the patients because of its fixed position. Most GHJ loose bodies are considered stable during dynamic US evaluation.
Table 5-3. Classification of loose bodies.
Loose bodies composed of organized connective tissue are the commonest type and results from osteochondral fragments frequently associated with osteochondral lesions, synovial chondromatosis, and trauma. The detached cartilage does not lose its capability to absorb nutrients and oxygen from the synovial fluid and often increases in size, resulting in a smoother surface over time as the bony component of the osteochondral loose body gradually becomes completely surrounded by the chondral component. Radiographs may show the abnormality, but typically underestimate the problem because nonmineralized portions of the fragment are not radiographically apparent. At US, osteochondral loose bodies are depicted as echogenic structures with variable shadowing. Two common locations include the posterior recess (figure 5-28) and the long head of the biceps brachii tendon sheath (see figure 3-17). When entirely cartilaginous, the loose bodies are homogeneously hypo-anechoic and difficult to distinguish from surrounding fluid.
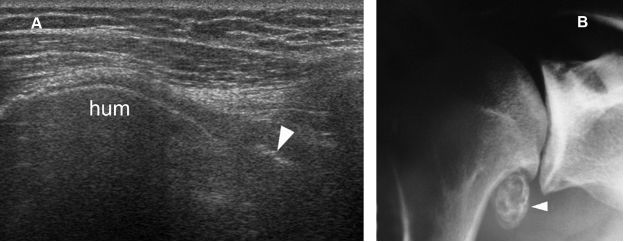
Figure 5-28. Loose body. [A] Axial 12-5 MHz US image obtained from a dorsal approach shows an echogenic loose body (arrowhead) in the axillary GHJ recess. [B] Corresponding radiography confirms sonographic finding. Hum= humerus.
Fibrinous loose bodies are second in prevalence to organized connective tissue, consist of concentrically laminated masses of fibrin, and result from fibrinous degeneration of the infarcted synovial tissue or from bleeding within the joint. They are usually numerous, almost invariably associated with an effusion, and typically associated to degenerative or inflammatory joint disease. Fibrinous loose bodies may resemble rice grains, melon seeds, or adhesive wafers, and are not visible on radiographs. At US, they appear as multiple small hypoechoic structures surrounded by fluid, although in some cases they may be difficult to differentiate from adjacent hypo-echoic pannus due to similar echogenicity.
Foreign loose bodies are the rarest type and may result from a dislodged piece of surgical hardware or a penetrating injury.
Whatever the type, estimating the size of the loose bodies is important for better management planning as arthroscopic removal of larger fragments may be difficult and time consuming.66
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree