GLOSSOPHARYNGEAL NEUROPATHY AND REFERRED OTALGIA
KEY POINTS
- Computed tomography including computed tomographic angiography is the primary tool for looking for a structural cause of a cranial neuropathy that is likely to involve the skull base or more distal course of the nerve in question.
- Magnetic resonance imaging should be used if the pathology likely localizes to the brain stem or cisternal segment of the nerve(s) in question.
- Magnetic resonance imaging and magnetic resonance angiography cannot be trusted to confidently exclude all conditions that may lead to these neuropathies.
- The causative pathology may be of the end organ or other structures innervated by the nerve rather than the nerve itself.
- Diagnostic imaging, even performed optimally, fails to find a reason for these neuropathies in many patients; if the symptoms progress, follow-up imaging should be strongly considered.
INTRODUCTION
Clinical Presentation
The glossopharyngeal, vagus, spinal accessory, and hypoglossal nerves and cervical sympathetic plexus may be considered as a unit as well as individually. Although one of these may dominate the clinical presentation, more than one will often be involved following careful clinical testing. When more than one nerve is affected, and possibly associated with other symptoms or neurologic deficits, localization may be much easier and a very “directed” and concise imaging evaluation is possible. However, some situations require a comprehensive imaging study of nearly the entire head and neck region and sometimes the upper chest. For instance, cranial nerve (CN) X and cervical sympathetics have a long course between the brain and skull and the chest, and CNs IX and X have important pathways of referred pain. Such considerations and combinations of clinical findings may affect the imaging approach to identify a source of a patient’s presenting complaints and deficits. This clinically responsive tactical approach should become apparent later in this chapter and in Chapters 138 through 141.
Sometimes, lesions outside the expected course of the nerves or those involving end organs will be the source of symptoms—for example, a tongue base carcinoma causing ear pain that is referred along the glossopharyngeal nerve. Moreover, it is usually not possible to tell clinically if otalgia is more likely to be mediated by CN IX or X; thus, an “otalgia protocol” must cover the pyriform sinus as well as the tongue base as a possible symptom generator. It is critical to understand all of the neurologic deficits and complaints that might arise from these nerves to enable optimal protocol design for the most effective imaging as well as for optimal interpretation of the images.
Isolated glossopharyngeal nerve dysfunction is unusual. Pathologic processes that will be apparent on imaging studies usually involve the IX, X, XI complex. Isolated glossopharyngeal nerve pathology may cause otalgia, dysphagia, odynophagia or other throat pain, loss of cough or gag reflex, loss of taste of the posterior one third of the tongue, dry mouth hypotension, tachycardia, or bradycardia.
Clinical presentations that may involve CN IX are summarized as follows:
Lesions Within the Skull
- Brain stem and extra-axial lesions in the low cerebellopontine angle and medullary cisterns may present as lower CN deficits. Intra-axial lesions will almost always be accompanied by some sensory or motor symptoms and related physical findings.
Jugular Fossa Syndromes
- Several French eponyms have been applied to clinical findings when three, four, or five (if the sympathetics are included) members of this group of nerves are involved. These include Vernet syndrome (IX–XI), Collet-Sicard syndrome (IX–XII), and Villaret syndrome (IX–XII and the sympathetic plexus).
- French eponyms are mentioned because they are occasionally presented as an indication for the imaging procedure; however, it is more useful to describe the specific nerves at risk. If three of the five are involved, the lesion will be at or near the skull base. The lesion will usually be somewhere between the medullary cistern–jugular fossa region and the posterior belly of the digastric muscle. If just two are involved, the lesion could lie in this relatively confined space in and around the skull base but a more comprehensive imaging evaluation often becomes necessary.
Referred Otalgia
- Referred otalgia is a very important symptom in upper aerodigestive tract disease, and it will most commonly come to imaging if progressive. Once temporomandibular joint syndromes, the salivary glands, and similar sources of pain that may have a periauricular location have been excluded clinically, it is important that these patients also have a complete clinical evaluation of the nasopharynx, oropharynx, and hypopharynx as well as otoscopy by an experienced otolaryngologist. Depending on this initial triage, they may be referred for imaging.
- Otalgia may come from middle ear disease caused by eustachian tube dysfunction, such as that caused by nasopharyngeal carcinoma. Referred otalgia may be via CN IX from the tongue base or tonsil or via CN X from the pyriform sinus. The cause, if found, may be a carcinoma at one of these sites. Progressive, possibly referred, otalgia must be viewed with a very high index of suspicion even in light of negative upper aerodigestive tract endoscopy especially in the smoking/drinking population.
- Glossopharyngeal neuralgia is, in reality, intense throat pain but may be lumped in this group since referred otalgia may be an accompanying complaint. The clinical problem of “globus sensation” is best considered in this context as well. Glossopharyngeal neuralgia is a clinical diagnosis of exclusion, and nowadays a “functional” diagnosis such as this can only be made in the face of detailed negative imaging studies when the complaint is worsening progressively.
APPLIED ANATOMY
Cranial Nerve Nucleus and Cisternal Segment
CNs IX, X, and XI share nuclei of the medulla (Fig. 137.1). Motor fibers of all three nerves originate in the nucleus ambiguus dorsal to the inferior olivary nucleus. Sensory fibers of CNs IX and X arise from their superior and inferior ganglia at the level of the jugular foramen and enter the brain stem between the medullary olives and the inferior cerebellar peduncle. The fibers course in the tractus solitarius and end in the nucleus solitarius. Parasympathetic fibers originate from the inferior salivatory nucleus in the upper part of the medulla oblongata.
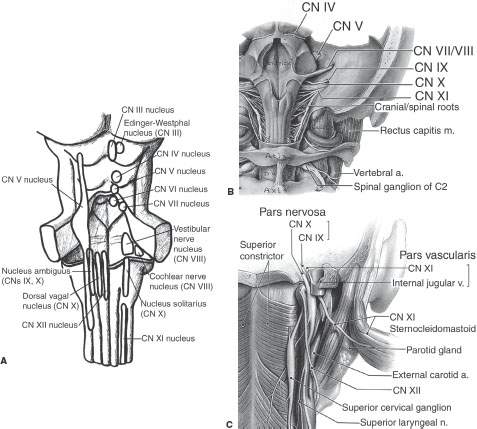
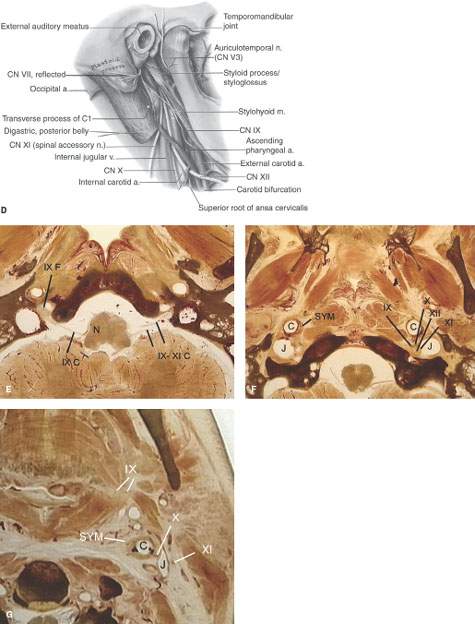
FIGURE 137.1. Anatomy of glossopharyngeal nerve. A–D: Anatomic drawings of the brain stem nuclei (A), cisternal segment (B), skull base segment coursing through the jugular foramen (C), and peripheral segment (D) of cranial nerve IX. E–G: Anatomic sections showing the course of cranial nerve IX from its nucleus in the medulla (N) to the tongue. (IXc, cisternal segment; IXf, foraminal segment; SYM, sympathetic plexus; C, carotid artery; J, jugular vein.)
Once they leave the medulla oblongata at the posterolateral margin, the roots traverse the basal cistern, often conjoined.
Foraminal/Skull Base Segment
The more medial and smaller of the two jugular fossa compartments known as the pars nervosa contains the terminus of the inferior petrosal sinus and the glossopharyngeal nerve (CN IX) (Fig. 137.1). The more lateral of the two known as the pars vascularis is larger and contains the jugular bulb, vagus nerve (CN X), and spinal accessory nerve (CN XI) (Figs. 104.10A–C and 137.2A–D). Within the jugular foramen, CN IX gives off its auricular or tympanic branch (Jacobson nerve), supplying sensory fibers to the middle ear.
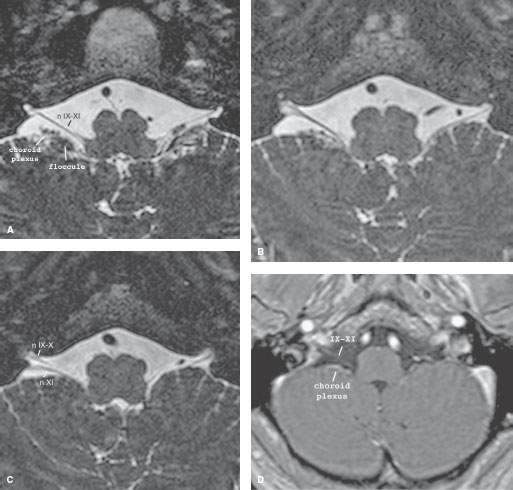
FIGURE 137.2. Normal magnetic resonance appearance of the cisternal segment of cranial nerves IX, X, and XI. A–D: On three-dimensional steady state (SS) images, the IX through XI complex leaves the medulla oblongata at the posterolateral sulcus and crosses the medullary cistern in front of the flocculus to the jugular foramen (A–C). The nerves do not enhance (D).
Peripheral Segment
The glossopharyngeal nerve follows the carotid sheath, diverging lateral to the stylopharyngeus muscle, where it lies between the internal and external carotid arteries (Fig. 137.1). Just above the level of the hyoid, the nerve curves upward and forward to terminate in the posterior sublingual space of the floor of the mouth. On its way peripherally, it sends motor and sensory branches to the pharynx and posterior third of the tongue.
Innervation End Organ
CN IX has a motor branch to the stylopharyngeus, superior pharyngeal constrictor (with branches of CN X), and styloglossus muscle (Fig. 137.1). Several branches supply sensation to the middle ear and bony eustachian tube, the posterior oropharynx and soft palate, and sensation and taste to the posterior third of the tongue.
IMAGING APPROACH
Techniques and Relevant Aspects
General imaging parameters used in cranial and cervical sympathetic neuropathies often require a combination of high-detail images from the posterior fossa to the hyoid bone and more of a survey approach from the hyoid to the thoracic inlet and upper chest. Detailed views of a specific end organ such as the tongue base may also be required. Overall, multidetector computed tomography (MDCT) is well suited to accomplishing all of these tasks very efficiently, and magnetic resonance imaging (MRI) can be focused on a specific area for problem solving when required.
For patients with glossopharyngeal neuropathy, a complete contrast-enhanced computed tomography (CT) study will usually include temporal bone and posterior skull base reconstructions with the same technique used to study primary temporal bone problems and high-detail images from the posterior fossa to the hyoid bone. Detailed views of the entire oropharynx are also required.
MRI may be used for the investigation of a glossopharyngeal neuropathy if the lesion is likely intracranial; however, MRI is more likely to be degraded in the pharynx below the hard palate due to motion artifacts and does not definitively exclude smaller skull base lesions. However, the evaluation of otalgia requires images to the bottom of the pyriform sinus since it is uncertain if otalgia may be referred via the Arnold nerve (from CN X) or the Jacobson nerve from CN IX. Magnetic resonance (MR) images through the pyriform sinus are generally less optimal in quality compared to CT.
Specific protocols for CT and MR studies for investigating a glossopharyngeal neuropathy appear in Appendixes A and B.
Diagnostic catheter angiography may be necessary in some instances to confirm the diagnosis of a paraganglioma if it is equivocal on imaging. Newer 320 MDCT units and those with similar z-axis coverage capability are able to assess flow dynamics and detailed angioarchitecture. Until these units become more generally available, diagnostic catheter techniques may remain necessary to assess these parameters, most often as a prelude to endovascular interventions that are usually an adjunct to surgical removal.
Radionuclide studies are used sparingly in cases likely to be due to skull base osteomyelitis. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) should have a minor adjunctive role in evaluating diseases that lead to these neuropathies.
Pros and Cons
MRI and magnetic resonance angiography (MRA) are not well suited to definitive evaluation of the region of the jugular fossa and posterior skull base. These imaging studies cannot confidently exclude causative pathology as being the main limitation; however, even obvious pathology may not be as definitively evaluated as with CT and computed tomographic angiography.
These limitations are essentially related to the inability of MRI to provide definitive bone information and because of the variability in the area of main interest around the petromastoid junction caused by the common occurrence of bone, air, and fat interfaces. This limitation of MRI and MRA is further complicated by flow-related artifacts that are often exacerbated by the use of contrast (Chapter 104).
On the other hand, if the lesion is likely to be intracranial— either purely intra-axial or caused by leptomeningeal pathology—then the use of MRI for the detection of those processes is clearly superior to CT. However, these intracranial sites are much less frequently the origin of disease in neuropathies that present without somatic sensory or motor deficits. MRI may be used first when the pathology is likely to be meningeal or intra-axial, although even in such cases well-done initial CT would produce at least suspicious findings that would lead to MR in any case.
PATHOPHYSIOLOGY AND PATTERNS OF DISEASE AS SEEN ON MAGNETIC RESONANCE IMAGING AND COMPUTED TOMOGRAPHY
Introduction
The specific pathologies that involve the CNs are variable but can be grouped by three broad mechanisms of disease, including primary neurogenic tumors, pathology that causes a particular point of compressive neuropathy, and infiltrating neuropathies (Fig. 137.3A–F). It is essential to determine first the specific localization of the offending pathology; this is logically and perhaps best approached by a systematic evaluation of the nerve from its brain stem origin to its end organ(s) that generate the signs and symptoms of disease. Following that, a morphologic evaluation of the disease process will almost always lead to a specific diagnosis or very short list of possibilities.
Cranial Nerve Nucleus
The CN nucleus is typically diseased due to intra-axial brain tumors, demyelinating disease, vascular disease, and rarely some unusual infectious disease (Fig. 137.4A–D). The clinical localization usually includes a combination of cranial neuropathy and sensory and motor findings and is more in the realm of central nervous system than extracranial head and neck pathology.
Cisternal Segment
The cisternal segment is most often involved by intracranial or transcranial extra-axial tumors, with the most common by far being paraganglioma, schwannoma (Fig. 137.5A–D), and meningioma (Fig. 137.5E–J). Uncommon pathologies include dural and leptomeningeal chronic inflammatory diseases as diverse as sarcoidosis and chemical meningitis from a ruptured dermoid or rarely epidermoid cyst and infiltrating malignancies such as lymphoma and leukemia and meningeal carcinomatosis (Fig. 137.6).
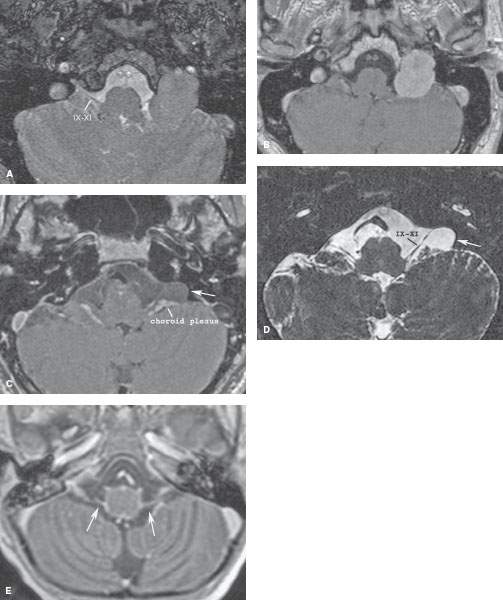
FIGURE 137.3. Lower cranial neuropathies—mechanisms of disease. A, B: Primary tumor. Neuropathy due to neurogenic tumors of cranial nerves IX, X, and XI occurs late in the disease. This patient with a jugular foramen schwannoma was still asymptomatic at the time of this study. It is most often very difficult to know from imaging the actual source cranial nerve of a jugular foramen neurogenic tumor. C, D: Compression. Lesions adjacent to a cranial nerve, such as this arachnoid cyst (arrow), may cause compressive neuropathy. E: Infiltrative disease. In this child with tuberculous meningitis, diffuse basilar meningeal enhancement as well as enhancement of cranial nerves IX, X, and XI is present. This pattern is also seen in meningeal carcinomatosis, leukemic and lymphomatous leptomeningeal infiltration, sarcoidosis, and other less common diseases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








