GRAVES DYSTHYROID OPHTHALMOPATHY (ORBITOPATHY)
KEY POINTS
- Imaging with computed tomography, magnetic resonance, or ultrasound can easily confirm the clinical impression of Graves dysthyroid ophthalmopathy.
- If an alternative diagnosis is possible, imaging will very likely help make that differential diagnosis more clear.
- Computed tomography and magnetic resonance imaging can be predictive of compressive optic neuropathy due to Graves dysthyroid ophthalmopathy.
- Computed tomography and magnetic resonance imaging are useful in treatment surveillance.
INTRODUCTION
Etiology
Graves disease is the most common cause of hyperthyroidism. It occurs far more commonly in women, and there is a familial predisposition. It is a potentially devastating disease with regard to its orbital manifestations that has several names, including dysthyroid ophthalmopathy, dysthyroid orbitopathy, and Graves dysthyroid ophthalmopathy (GDO). The latter designation will be used in this chapter.
This disease is also discussed and illustrated in Chapter 20 on autoimmune diseases.
Prevalence and Epidemiology
Graves disease is seen worldwide, with a marked predilection in women. It occurs primarily in adults between 30 and 50 years of age and is unusual in children. It is the most common cause of proptosis in adults.
Clinical Presentation
Proptosis is a common clinical presentation for GDO. The proptosis is most commonly bilateral, although thyroid ophthalmopathy is also the most common cause of unilateral proptosis in adults. Visual loss and disordered eye movements, with diplopia, may also occur.
ANATOMY AND PATHOPHYSIOLOGY
Anatomy
The relevant anatomy of the orbit, eye, and optic nerve/sheath complex is discussed in detail in Chapter 44.
Pathology and Patterns of Disease
Graves disease affects the thyroid gland and orbits. It is caused by B- and T-lymphocyte reaction to thyroid-stimulating hormone (thyrotropin) receptors (TSHR) that cause hyperstimulation of the gland and therefore a reduced thyroid-stimulating hormone level. Orbital fibrocytes of the extraocular fat and connective tissue also (like the thyroid gland) have a high expression of TSHR. The resulting lymphocyte and macrophage reactive process affects the extraocular soft tissues and most dramatically the extraocular muscles.
GDO, for imaging purposes, may be divided into two categories based on whether or not there is associated optic neuropathy1,2 (Figs. 58.1–58.5). It may also be grouped by its likely acute/subacute phase (Figs. 20.11, 20.12, and 58.1–58.5) and later chronic fibrotic changes (Fig. 58.6).
Optic neuropathy is usually caused by compression of the optic nerve at the orbital apex by enlarged extraocular muscles1,2 (Figs. 58.3–58.5). This may be aggravated by the associated inflammatory reaction and vascular congestion also seen as part of the disease (Fig. 58.1). Effacement of 50.0% or more of the fat around the extraocular muscles correlates with a 66.7% chance of neuropathy, while lesser degrees of effacement of the fat planes strongly suggest that the cause of optic neuropathy will be unrelated to Graves disease.1,2 Patients with optic neuropathy may also have dilatation of the superior orbital vein due to vascular congestion and hydrops of the retrobulbar segment of the optic nerve/sheath complex.1 Increased orbital fat may be the only major manifestation of this disease (Fig. 58.2), but for the majority of cases, enlargement of the extraocular muscle(s) is the main imaging feature. When only one muscle is affected (6% of cases), it tends to be the superior muscle complex rather than the medial or the inferior rectus as previously reported1 (Fig. 58.2). The remaining cases demonstrate enlargement of more than one muscle. The superior oblique muscle is much less often affected, and the lateral rectus is affected less than the others. The disease is generally bilateral but often not to the same degree. At early stages of orbitopathy, changes may appear unilateral.
Chronically, the muscles may become atrophic, fat replaced, and fibrotic (Fig. 58.6).
Pathologically Altered Function
The disease causes proptosis that may cause the cornea and sclera to become dry and irritated because those structures have less coverage by the eyelids and tear pool.
The swelling of the muscles may lead to disordered eye movements. When the swelling of the muscles and surrounding soft tissues becomes substantial, a secondary optic neuropathy and loss of vision may occur.
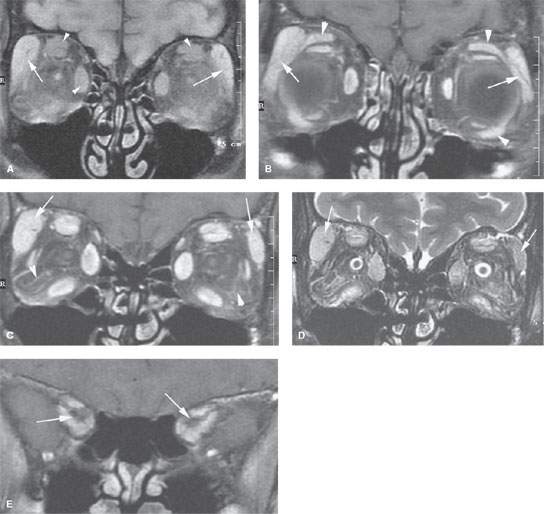
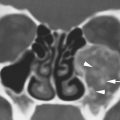
FIGURE 58.1. Magnetic resonance imaging study of a patient with active Graves dysthyroid ophthalmopathy (GDO) and bilateral optic neuropathy. A: T1-weighted (T1W) fat-suppressed image showing enlargement of the lacrimal glands bilaterally (arrows). The extraocular muscles are also enlarged (arrowheads). B: Contrast-enhanced T1W fat-suppressed images show enlargement and abnormal enhancement of the lacrimal glands on both sides (arrows). The extraocular muscles are also enlarged; note that the levator palpebrae and inferior oblique muscles can be involved in this process (arrowheads). C: Contrast-enhanced T1W fat-suppressed image slightly posterior to that seen in (B) again shows markedly enlarged, enhancing lacrimal glands (arrows). All extraocular muscles are enlarged. There is extensive edema and vascular congestion within the orbital fat (arrowheads). D: T2-weighted image showing the enlarged lacrimal glands (arrows). All extraocular muscles are enlarged. There is very extensive vascular congestion and edema in the orbital fat. E: Contrast-enhanced T1W image at the orbital apex shows marked loss of the orbital fat around the optic sheath. (NOTE: The compressive optic neuropathy resolved following successful treatment of the GDO.)
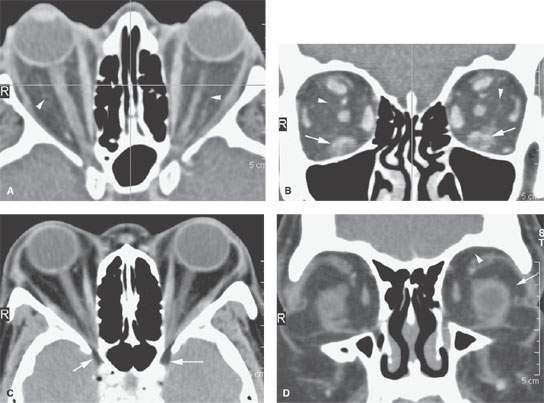
FIGURE 58.2. Two patients with bilateral proptosis. A, B: Patient 1 with subacute Graves dysthyroid ophthalmopathy (GDO) but no evidence of optic neuropathy. In (A), the axial contrast-enhanced computed tomography shows severe, bilateral proptosis. There is a generalized increase in the volume of orbital fat and evidence of edema and vascular congestion of the intraconal fat (arrowheads). In (B), coronal reformations show predominant involvement of the inferior rectus muscles on both sides. The muscles are edematous, and there is also edema surrounding both muscles. There is also generalized vascular congestion and edema within the intraconal fat (arrowheads). C, D: Patient 2 with bilateral proptosis. In (C), there is a generalized increase in the volume of orbital fat, so much so that it protrudes well through the superior orbital fissure (arrows)—a sign that has been associated with GDO. Note that there is no evidence of vascular congestion within the orbital fat. In (D), the coronal image shows the generalized increase in orbital fat with no real signs of abnormalities of the intraocular muscles. Note that both the intraconal (arrow) and extraconal (arrowhead) fat volume is increased. (NOTE: The second patient did not have GDO but was extremely obese and had excessive orbital fat on that basis.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree