and Sofia Gourtsoyianni2
(1)
UOC Radiologia BR, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy
(2)
Imaging 2, Level 1, Lambeth Wing St Thomas’ Hospital, London, UK
Haemangioendothelioma, Epithelioid
Hepatic epithelioid haemangioendothelioma (HEHE) is a rare, malignant, vascular tumour which originates from endothelial cells and is more common among women. Its histologic appearance and behaviour range between haemangioma and haemangiosarcoma.
HEHE is known to occur in individuals of all ages, and no definitive etiological factor has been clearly identified. Its rarity and non-specific symptoms make the diagnosis of this entity very challenging, with the majority of cases being misdiagnosed.
There are two subtypes: the nodular, present in early stages, characterised by multifocal nodules, and the diffuse subtype at later stages when nodules grow and eventually coalesce, forming large confluent masses preferentially involving the periphery of the liver.
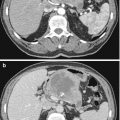
There is great heterogeneity regarding imaging features of HEHE. The liver lesions are typically hypoechoic on US, hypodense on CT and usually hypointense on T1-weighted images and hyperintense on T2-weighted images with a target-like appearance also reported. A hypointense centre may correspond to calcification, necrosis and haemorrhage. Moderate peripheral enhancement and delayed central enhancement are seen.
Definitive diagnosis of HEHE is established by immunohistochemical evidence of endothelial differentiation.
Haemangioma
Haemangioma is the most common benign liver tumour, comprised of interconnected endothelial-lined vascular channels, enclosed within loose fibroblastic stroma and fed by hepatic artery branches.
At nonenhanced CT haemangiomas appear as hypodense well-defined lesions. After contrast administration, early nodular peripheral enhancement is seen, followed by slow centripetal fill-in. In the delayed phase, the lesion is isodense or slightly hyperdense to the adjacent parenchyma.
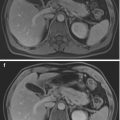
At MRI, haemangiomas characteristically present with a very long T2 relaxation and appear hypointense on T1-weighted images. Large haemangiomas are usually heterogeneous, containing various combinations of fibrosis, haemorrhage, thrombosis, hyalinisation and cystic degeneration. Typical imaging findings are early hyperintense peripheral nodular enhancement with complete fill-in on delayed imaging.
When small, haemangiomas usually present with uniform early enhancement. Persistent central hypointensity occurs due to fibrosis, thrombosis or degeneration.
Haemochromatosis
In the primary or genetic form of haemochromatosis, there is excessive absorption of iron in the intestine, which cannot be eliminated by the body and accumulates in various organs, causing irreversible damage. In the secondary form, the excess in iron comes from multiple blood transfusions or blood disorders, such as haemolytic anaemia.
The magnitude of body iron stores distinguishes patients who will benefit from treatment from those merely at risk for the disease. MRI is the most sensitive and accurate method to demonstrate and quantify iron overload by using dedicated T2* GRE imaging with different echo times that allow for precise quantification of iron deposition in μmol /g (T2* relaxometry). Liver signal decrease is proportional to the magnetic susceptibility changes induced by iron. T2 relaxometry is the best method to quantify liver iron concentration using MRI. It is accurate and reproducible at all levels of iron overload and also allows myocardial iron concentration to be measured. However, T2 relaxometry models are not yet standardised nor are widely available. On the other hand, signal intensity ratio (SIR) methods, measuring SIR between the liver and other tissues in which iron is not generally deposited, usually paraspinal muscles, although less accurate with values of liver iron concentration >350 μmol Fe/g, have high specificity at all levels of iron overload, have been standardised, are reproducible and are already widely available.
In haemochromatosis the pancreas and myocardium may also be involved but not the spleen. Pancreatic involvement aids in differentiation between cirrhosis with liver iron overload and haemochromatosis with secondary cirrhosis. Hereditary haemochromatosis is associated with an increased risk of HCC.
Hepatic Abscess
Hepatic abscesses appear as isolated or multiple, focal, cystic, liver lesions presenting with thick enhancing capsule on cross-sectional imaging in a patient that is usually febrile.
Hepatic abscess may be due to biliary tree infection and ascending abdominal infections (appendicitis, diverticulitis, IBD) or secondary to RF or transarterial chemoembolisation with immunosuppressed patients being more prone. Appearances depend on the pathogen, with Candida producing multiple small abscesses (<5 mm).
On ultrasound hepatic abscess presents as a hypoechoic to anechoic round mass that might contain septa and debris. Presence of gas is hyperechoic with an acoustic shadow.
At CT, liver abscesses present with peripheral enhancement and central low density. They can occasionally appear solid.
At MRI, they appear heterogeneously hypointense on T1-weighted images and hyperintense on T2-weighted images, with peripheral enhancement. On DWI-MRI abscesses show restricted diffusion on higher b-value images and low ADC values.
Hepatic Adenoma
Hepatic adenoma is a rare benign liver tumour, containing well-differentiated hepatocytes but lacking bile ducts or portal tract. It is seen most commonly in patients with previous history of oestrogen intake (e.g. oral contraception), androgen steroid therapy or underlying metabolic disease. Eighty percent are solitary, when multiple (usually >10 adenomas) the condition is known as hepatic adenomatosis. There is female predominance.
Adenomas are asymptomatic until they present with pain, bleeding and rupture (malignant potential). If size > 3–5 cm, surgery should be considered.
On non-contrast CT, the lesions can appear isodense, hypodense due to the fat component or hyperdense due to haemorrhage.
At MRI, non-haemorrhagic lesions have variable T1 intensity and appear mildly hyperintense on T2-weighted images. Chemical shift imaging characteristically shows a drop of signal in the out-of-phase images.
After contrast administration, adenomas demonstrate moderate arterial enhancement and washout in the portal venous phase.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree