Vice-Chair for Radiology Informatics
Section Head of Musculoskeletal Radiology
University of Washington and Harborview Medical Center
Seattle, WA
Catherine Maldjian, M.D.
Albert Einstein College of Medicine
Chief, Musculoskeletal Radiology
Bronx-Lebanon Hospital Center
New York, NY
With Contributions By
Hyojeong Mulcahy, M.D.
Assistant Professor, Musculoskeletal Radiology
Director of Resident Education in Musculoskeletal Radiology
University of Washington and Harborview Medical Center
Seattle, WA
Christin M. Brown, M.D.
Lieutenant Commander, U.S. Navy
Senior Fellow and Acting Instructor, Musculoskeletal Radiology
University of Washington and Harborview Medical Center
Seattle, WA
BareBonesBooks.com
Seattle, WA
2009
Publication Information
Copyright © 2009 Felix S. Chew, M.D.
ISBN-13: 978-0-9824076-1-5
ISBN-10: 0-9824076-1-0
All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form or by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner.
The publishers have made every effort to trace the copyright holders for borrowed material. If they have inadvertently overlooked any, they will be pleased to make the necessary arrangements at the first opportunity.
PREFACE
This is an atlas of fractures, as demonstrated by x-ray images (radiographs and computed tomography). It is intended for the use of anyone with an interest in fractures.
The 369 cases in this atlas are arranged anatomically. In Chapter 1, we illustrate fractures and dislocations involving the hand, beginning with injuries to the distal phalanges of the fingers, continuing with injuries of the distal interphalangeal, proximal interphalangeal, and metacarpophalangeal joints, and ending with injuries of the carpometacarpal joints. In Chapter 2, we consider fractures and dislocations of the wrist, including fractures and dislocations of the individual carpal bones and combinations of carpal bones, perilunate injuries, radiocarpal injuries, distal radius injuries, and isolated distal radioulnar joint injuries. Chapter 3 begins with forearm injuries, including Galeazzi, Monteggia, and Essex-Lopresti fracture-dislocations, continues with elbow fractures and dislocations, and ends with humeral shaft fractures. In Chapter 4, we illustrate fractures and dislocations about the shoulder and shoulder girdle, including the proximal humerus, scapula, clavicle, and thoracic cage. We show examples of fractures and dislocations of the spine in Chapter 5, beginning with the craniocervical junction, including the cervical, thoracic, and lumbar regions, and ending with the sacrum. Chapter 6 begins with injuries of the pelvic ring and includes injuries of the acetabulum, hip joint, and proximal femur. In Chapter 7, we show injuries of the femoral shaft and knee. Chapter 8 covers injuries of the lower leg and ankle. In Chapter 9, we illustrate fractures and dislocations of the talus, calcaneus, midfoot, and forefoot, ending with the toes. Chapter 10 is devoted to fractures and dislocations of the face. References are placed at the end of the book.
There are 939 radiologic images presented in this atlas. Most of images are drawn from cases seen at Harborview Medical Center (Seattle, WA) the Level 1 Trauma Center that serves the states of Washington, Wyoming, Alaska, Montana, and Idaho. Additional cases were drawn from the teaching collections of the University of Washington and from my personal teaching collection. A few images have been previously published and are used with permission. I would like to acknowledge the many friends and colleagues who freely contributed cases to this effort.
Felix S. Chew, M.D.
DISCLAIMER: The information provided in this work is for educational and informational purposes only, and should not be considered as offering medical advice. If you think that you may have a broken bone or other illness, please check with a qualified physician or other appropriate health care provider.
Table of Contents
Chapter 1. Hand
Chapter 2. Wrist
Chapter 3. Forearm, Elbow, and Upper Arm
Chapter 4. Shoulder and Thorax
Chapter 5. Spine
Chapter 6. Pelvis and Hip
Chapter 7. Thigh and Knee
Chapter 8. Lower Leg and Ankle
Chapter 9. Foot
Chapter 10. Face
References
Abbreviations and Acronyms
Chapter 1. Hand
by Catherine Maldjian, M.D., and Felix S. Chew, M.D.
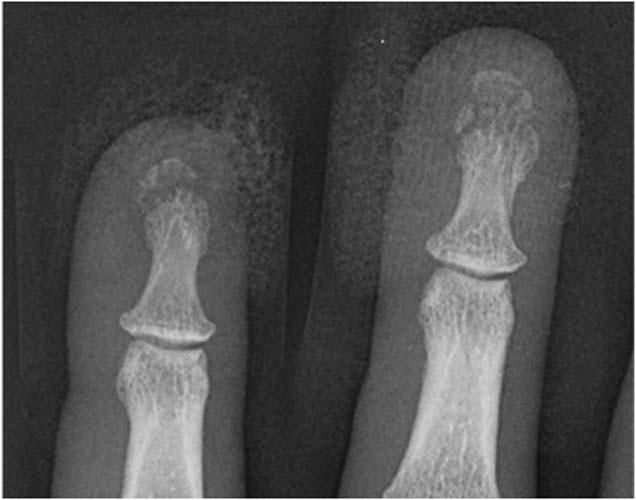
Case 1-01. Phalangeal tuft fractures. PA radiograph of the index and middle fingers centered over the DIP joints. This case demonstrates comminuted phalangeal tuft fractures. Over 50% of all phalangeal fractures involve the distal phalanx, most often involving the ungual tuft. These can be comminuted or non-comminuted. Fibrous septa extending from periosteum to skin resists displacement. Lacerations of the nail bed may occur with this fracture pattern. 42% of phalangeal fractures involve the middle finger [1-3].



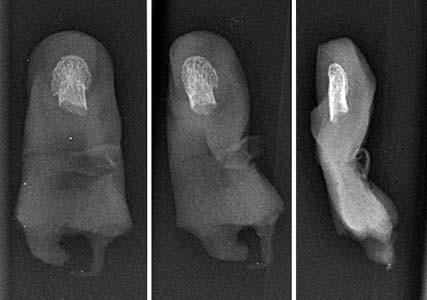
Case 1-02. Phalangeal tuft fracture with nail bed injury. Multiple radiographs of the hand. There is a comminuted fracture of the distal phalangeal tuft of the thumb, as might occur with a self-inflicted, accidental hammer blow. There is a laceration of the nail bed (arrow).

Case 1-03. Fingertip amputation. PA radiograph of the index and middle fingers. There is an amputation of a part of the distal phalanx of the index finger. Fingertip injury is treated with revision amputation if over 50% of the distal phalanx is absent or nail bed is significantly damaged. Bone is resected to the level of the residual nail bed. Complications of surgery include the formation of neuromas.

Case 1-04. Mallet finger. Lateral radiograph of a finger centered over the DIP joint. This case demonstrates a fracture at the dorsal aspect of the base of distal phalanx with slight flexion of the DIP joint. This site constitutes the insertion of the common extensor tendon insertion. This injury is a fracture/avulsion of the common extensor tendon insertion at dorsal base of the distal phalanx. A direct blow to the fingertip with forced flexion at the DIP joint, as from a baseball, gives rise to this fracture pattern, also known as baseball finger. On the lateral projection, the resultant unopposed flexion from extensor avulsion resembles a mallet. This injury may also be called a mallet finger. Most cases of mallet finger are pure avulsion of the ligament with no fracture. Only 25 percent of cases of mallet finger will demonstrate an avulsion fracture [4].
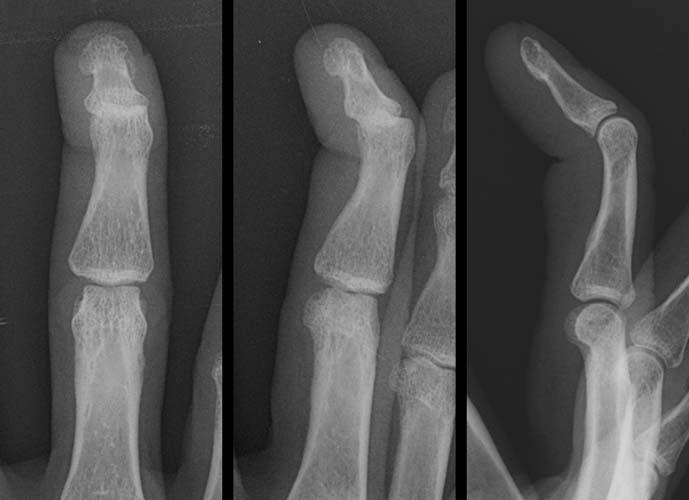
Case 1-05. Mallet finger. PA, oblique, and lateral radiographs of the middle finger. There is an isolated flexion deformity at the DIP joint, without fracture. This lesion is a soft tissue mallet finger, with rupture of the common extensor tendon.

Case 1-06. Simultaneous mallet fingers in a soccer goalie. Lateral radiograph of the middle and ring fingers. There are fractures at the bases of the distal phalanges of the middle and ring fingers on their dorsal aspects, without flexion deformity. Unlike a baseball, a soccer ball is large enough to cause simultaneous mallet fingers in adjacent digits. Axial compression of the finger tip against the middle phalanx, rather than forced flexion, may also produce fractures of the distal phalanx similar to mallet finger, but in these cases, there is preservation of the extensor tendon [5].



Case 1-07. DIP dislocation. PA, oblique, and lateral radiographs of the middle finger. There is dorsal dislocation of the distal phalanx. Dislocations in the hand are usually dorsal and easily reducible, often by the patients themselves at the time of injury. The mechanism of injury is is hyperextension.



Case 1-08. DIP dislocation. PA, oblique, and lateral radiographs of the ring finger. There is volar dislocation of the distal phalanx with crush injuries of the soft tissues. Volar dislocations in the hand are uncommon and often irreducible.



Case 1-09. Thumb dislocation. Oblique and PA radiographs of the thumb. There is dislocation of the IP joint with dorsolateral dislocation of the distal phalanx. These are uncommon injuries. Hyperextension and rotation are the mechanism of injury. A ruptured palmar plate can become interposed into the joint preventing non-surgical reduction.



Case 1-10. Medial condylar fracture of the middle phalanx. PA, lateral, and oblique views of the middle finger. This case demonstrates a fracture at the medial tip of the middle phalanx at the medial condyle or medial condylar fracture. This displaced, intra-articular fracture is best seen on an oblique view, and may require open reduction and internal fixation. Bicondylar T- or Y-shaped fractures may occur. Intra-articular malunion may lead to joint symptoms. Stable fixation of the small fragment can be technically challenging. The condylar advancement osteotomy has been developed to address this fracture pattern [6].


Case 1-11. Oblique phalangeal fracture. PA and oblique radiographs of the ring finger. There is an oblique fracture of middle phalanx extending to the joint surface. The mechanism of injury for oblique fractures is axial loading. Incongruity at the articular surface typically needs to be addressed surgically when it exceeds 2-3 mm.



Case 1-12. Crush injury of the thumb. Lateral, oblique and PA radiographs of the thumb. There is a near amputation with fracture through the proximal phalanx Circumferential soft tissue deformity and fracture deformity are at the same level; however, complete detachment has not occurred.



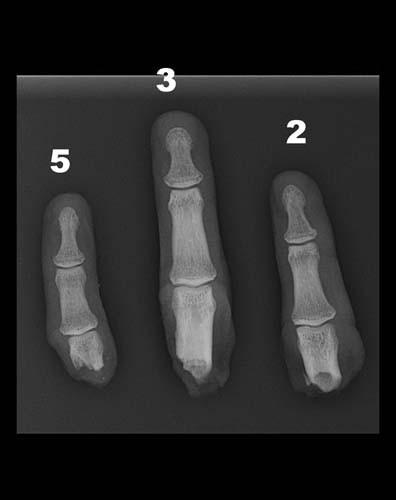
Case 1-13. Degloving injury with amputation. PA, oblique, and lateral views of the hand, and amputated fingertip. There is an amputated displaced digit with complex multiple finger fractures from blast. This is consistent with degloving injury of middle finger. Open degloving injuries, such as this, involves separation of all the soft tissues including the skin. In closed degloving injuries, the skin is not torn, but is separated from the underlying soft tissues. Replantation can be attempted when amputation is distal to the flexor digitorum superficialis insertion at the base of the middle phalanx.

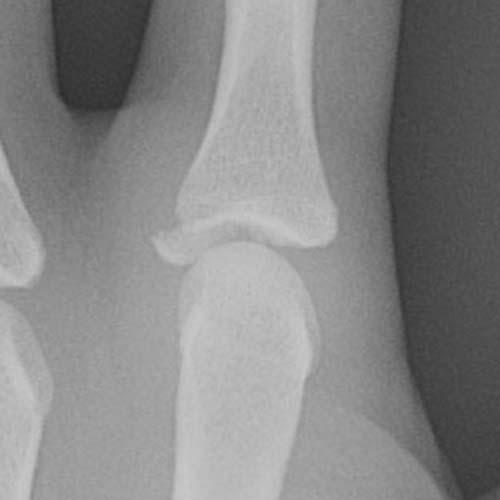
Case 1-14. PIP dislocation. Lateral view of the digit. There is dorsal dislocation of the middle phalanx. Dislocations are simple, which are easily reduced, or complex, which are irreducible [7]. A small calcific fragment is seen at the dorsal aspect of the proximal phalanx, likely a proximally displaced tiny avulsion from the volar aspect of the middle phalanx. These injuries are virtually always accompanied by volar plate detachment.



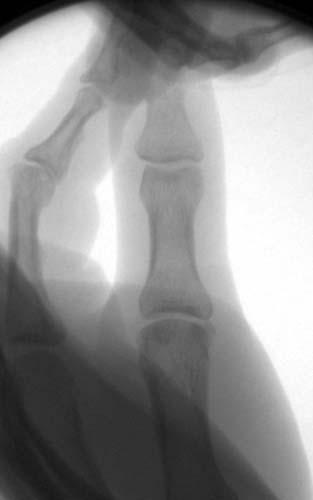
Case 1-15. Multiple PIP dislocations. Injury to hand while bowling. PA, oblique, and lateral views of the fingers. The middle and ring fingers demonstrate dorsal PIP dislocations with ulnar subluxation. PIP joint dislocations are the most frequent dislocations in the hand. Mechanism of injury for dorsal PIP dislocation is forced hyperextension with axial compression. Dorsal dislocation is associated with volar plate detachment, therefore, volar plate does not impede reduction in pure dorsal dislocation. Collateral ligament injuries may be associated.

Case 1-16. Volar plate fracture. Lateral view of a digit centered over the middle phalanx. This case demonstrates small avulsion fragment at the base of the middle phalanx on its volar side. Volar plate avulsion occurs from hyperextension injury that typically involving a small fragment of bone that is difficult to see. When a larger fragment is avulsed, dislocation is not uncommon and this is an unstable injury. Triple joint injury has been described with volar plate injury associated with dislocation [8].

Case 1-17. Volar plate fractures. Lateral view of the digits. There is are tiny fracture fragments (arrows) at the volar aspect of the base of the middle phalanges of the index and middle fingers, consistent with volar plate injuries. The mechanism of injury is hyperextension injury to the volar plate. Volar plate is present at the PIP joint and MCP joint, and avulsion injury manifests at the base of the proximal or middle phalanx.



Case 1-18. Ulnar PIP dislocation. PA, oblique, and laterals view of the ring finger. The PIP joint of the ring finger is dislocated towards the ulna. The lateral view shows that all three phalanges of the ring finger are in the same coronal plane, so there is no dorsal or volar component to the dislocation. Dislocations in the coronal plane are associated with collateral ligament injuries or avulsions. In this case, the radial (lateral) collateral ligament is disrupted. It is possible that the ulnar (medial) collateral ligament is also torn.

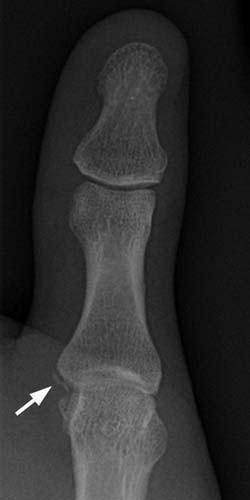
Case 1-19. PIP collateral ligament avulsion fracture. PA, Oblique, and Lateral views of the index finger. Soft tissue swelling surrounds the PIP joint. There is an avulsion fracture (arrow) of the medial margin of the middle phalanx of the index finger at the PIP joint, indicative of an ulnar (medial) collateral ligament avulsion. This injury may occur with forcible radial deviation of the PIP joint. If the ligament tears without fracture, stress views may be necessary to demonstrate the lesion.



Case 1-20. Volar PIP dislocation. PA, Oblique, and Lateral views of the little finger. There is volar dislocation of the PIP joint. Volar dislocation is very unusual.

Case 1-21. Proximal phalanx fracture. PA view of the third digit centered over the proximal phalanx. There is an oblique fracture of the proximal phalanx. The oblique fracture is due to axial loading / compression which gives rise to tangential shear stress to the bone maximized at 45 degrees. The oblique fracture line is denoted by its 45 degree angle. Indirect forces can generate a fracture by three mechanisms: tension, compression, and rotation. The fracture pattern elicited by these indirect forces is transverse, oblique, and spiral, respectively. Combined angulation and compressive forces gives rise to combined transverse and oblique fractures in the long bones.

Case 1-22. Proximal phalanx fracture. PA and oblique view of the index finger. There is a longitudinal fracture of the proximal phalanx extending into the PIP joint. Longitudinal fractures can arise from an indirect force at the tip of the digit, although the fracture occurs more proximally.

Case 1-23. Proximal phalanx fracture. PA and oblique view of the index finger. There is a spiral fracture of the proximal phalanx extending into the MCP joint.


Case 1-24. Multiple crush injuries. Radiographs of the hand. There are comminuted fractures of the proximal phalanges of all of the fingers, with near amputations. These injuries occurred in an industrial accident.

Case 1-25. Multiple finger amputations. Radiograph of the hand; radiograph of the amputated fingers. There are amputations of the index, middle, and little fingers through the proximal phalanges, with near amputation of the ring finger. These injuries occurred in an accident with a table saw.

Case 1-26. Gamekeeper thumb. PA view of the thumb. Avulsion fracture (arrow) of the proximal phalanx of the thumb at the attachment of the ulnar collateral ligament is seen, consistent with gamekeeper’s thumb. Mechanism of injury is valgus stress and hyperextension. In skiing, this occurs when the falling on an outstretched hand and the thumb hyperextends beyond the ski pole. This causes injury to the ulnar collateral ligament (UCL). The UCL of thumb is the most frequently injured collateral ligament in the hand. When the physis is open, this fracture pattern results in a Salter III injury.
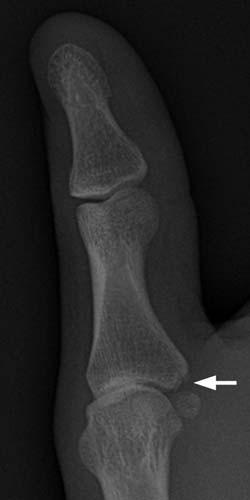
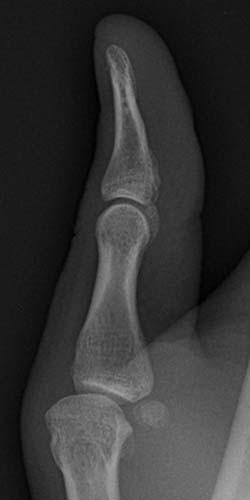
Case 1-27. Gamekeeper thumb. PA, oblique, and lateral views of the thumb. There is an avulsion fracture (arrow) of the proximal phalanx of the thumb at the attachment of the ulnar collateral ligament. The fragment of bone is very thin, just the thickness of the cortex.

Case 1-28. Gamekeeper thumb. PA views of the thumb without stress and with radial stress. This case illustrates a pure ligamentous injury manifesting as widening of the joint space (arrow) on stress view with no bony avulsion fragment. Without stress, the injury is radiographically occult. Complete tears may require surgery, in particular if there is displacement at the tear, with the torn ligament edges unopposed. Adductor aponeurosis can interpose between the distal and proximal edges of the torn ligament, known as a Stener lesion, and is an indication for surgery [9].


Case 1-29. Index MCP ulnar collateral avulsion fracture. PA view of the 2nd through 5th digits; Photographic magnifications. There is avulsion of the second metacarpophalangeal joint at the distal insertion of the UCL. Radial flexion leads to ulnar collateral ligament injury. Indications for surgery include over 2-3mm of displacement of avulsed fragment, over 20% of articular surface involvement of ulnar fragment. In addition, the abductor digiti quinti can cause ulnar deviation in the fifth digit and injury of the fifth MCP joint UCL is more likely to be treated with open reduction and internal fixation [10-11].



Case 1-30. First MCP dislocation. Oblique, PA, and lateral views of the thumb. There is dislocation of the 1st MCP joint with dorsolateral dislocation of the first proximal phalanx. Proximal volar plate disruption can show displacement of sesamoids with the proximal phalanx, whereas distal volar plate disruption does not cause relocation of the sesamoids away from the metacarpal head. Collateral ligament injuries are associated.



Case 1-31. Third MCP dislocation. Oblique, PA, and lateral views of the hand. There is dislocation of the third MCP joint with dorsolateral dislocation of the middle finger (arrow).



Case 1-32. Multiple MCP dislocation. Oblique, PA, and lateral views of the hand. There is dorsal dislocation of the second, third, and fourth MCP joints. A cast obscures detail on the images. This injury was sustained in a fall from a 30 foot height.



Case 1-33. Boxer’s fracture. Radiographs of the hand. There is a boxer’s fracture (arrow) through the necks of the fifth metacarpal, with volar angulation and marked dorsal soft tissue swelling.



Case 1-34. Boxer’s fracture in a 15-year-old male. Radiographs of the hand. There is a subtle volar bowing deformity (arrows) of the neck of the fifth metacarpal.



Case 1-35. Boxer’s fractures. Radiographs of the hand. There are boxers fractures through the necks of the fourth and fifth metacarpals, with volar angulation and soft tissue swelling.



Case 1-36. Third metacarpal neck fracture. PA, oblique, and lateral views of the hand demonstrate fracture of the third metacarpal neck. This is a transverse fracture of the metacarpal neck with volar angulation. The mechanism of injury is axial loading and bending, similar to a boxer’s fracture.


Case 1-37. Fourth metacarpal shaft fracture. PA and lateral views of the fourth metacarpal. There is a spiral fracture of the fourth metacarpal shaft. Indirect rotational forces comprised of tensile, compressive, and shear components gives rise to a spiral fracture.



Case 1-38. Gunshot wound. PA, Oblique, and lateral views of the hand. Small bullet and bone fragments are scattered through the hand along the path of the projectile. The bullet entered the hand at the third metacarpal, passed through the fourth MCP joint, and exited through the proximal phalanx of the little finger, amputating it. Low velocity gunshot wounds have less soft tissue deformity than high velocity gunshot wounds [12]. Mechanism of injury is direct loading along the path of the projectile. Entry and exit wounds may be seen and infection is a potential complication because foreign material is often drawn into the wound.
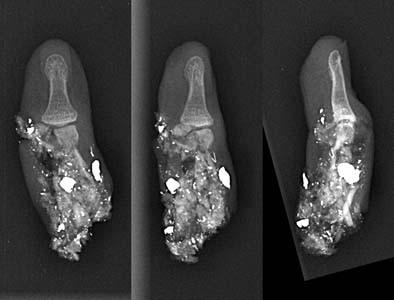
Although the amputated portion of the little finger was recovered at the scene and brought to the hospital with the patient, it was too severely damaged to replant.


Case 1-39. Extra-articular first metacarpal fracture. PA and lateral views of the hand. There is a transverse fracture through the proximal shaft of the first metacarpal that does not involve the articular surface. These fractures are typically treated without surgery.

Case 1-40. Bennett fracture. PA view centered over the basal joint. Fracture dislocation of first metacarpal base consisting of oblique fracture of the first metacarpal base and dorsal subluxation/dislocation of the dorsal fracture fragment [13]. Initial description was by a surgeon for whom the fracture pattern is named [14]. This is an oblique fracture incurred by mechanism of axial loading of a partially flexed 1st metacarpal. The dorsolateral pull of the abductor pollicis longus proximally and medial pull of the adductor pollicis on the metacarpal distally gives rise to the dorsal subluxation/dislocation component of this injury. This injury is unstable and is treated surgically in many cases by percutaneous pinning; however, associated dorsal ligament complex tear necessitates open reduction with repair of the ligament [15].

Case 1-41. Bennett fracture. Coronal 2-dimensional reformatted image from a CT of the wrist. There is a non-comminuted intra-articular fracture (arrow) at the base of the first metacarpal (Bennett fracture). These injuries constitute one-third of all fracture of the first metacarpal and are named after the surgeon who first described them.

Case 1-42. Rolando fracture. Oblique view of the thumb. A 3-part Y-shaped fracture at the base of the first metacarpal is seen consistent with a Rolando fracture. This is a comminuted, usually T or Y-shaped, intra-articular fracture of the base of the first metacarpal. Comminution distinguishes this fracture pattern from the more common Bennett fracture. If very comminuted, then it is not amenable to surgical correction and would be treated conservatively.
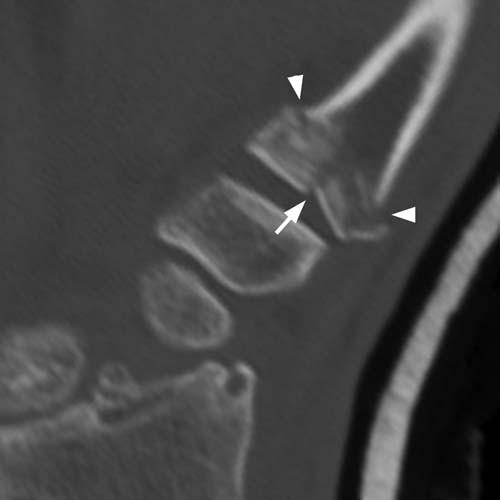
Case 1-43. Rolando fracture. Coronal 2-D reformat of a CT of the basal joint. There is a comminuted intra-articular fracture at the base of the first metacarpal. This fracture pattern is similar to, but less common, than the Bennett fracture. This fracture was named after Dr. Silvio Rolando [16]. Originally described as a three part fracture, consisting of the metacarpal shaft and two metacarpal base fragments (dorsal and volar), more extensive comminution can be seen. In the three part fracture, the fracture pattern assumes a Y or T shaped with metaphyseal fracture lines (arrowheads) that join into a vertical intra-articular fracture line (arrow) that separates the metacarpal base into dorsal and volar components.


Case 1-44. Volar dislocation of the fifth CMC. PA and lateral views of the wrist. The proximal end of the fifth metacarpal appears to have an articulation (arrow) with the triquetrum, which at first glance might be mistaken for normal. The fifth metacarpal (*) overlaps the distal articular surface of the hamate, indicating that there has been dislocation. On the lateral view, the fifth metacarpal (*) is projected volar to the second through fourth metacarpals, indicative of volar dislocation. The most common dislocation of the CMC joints is the fifth CMC joint, constituting approximately 50% of all CMC dislocations. This injury is often accompanied by another metacarpal dislocation (80%). Two-thirds are dorsal dislocations.



Case 1-45. Fifth CMC fracture-dislocation. PA, oblique and lateral views of the hand. The base of the fifth metacarpal (short arrow) appears to be floating and does not articulate with a carpal bone. It is also very anterior in position relative to the remaining metacarpals, consistent with 5th carpo-metacarpal volar dislocation. There is also a fracture of the fourth metacarpal (long arrow). Metacarpal dislocations are typically dorsal. Volar dislocation may be associated with volar plate entrapment and difficult to reduce. Of the CMC joints, the 5th CMC joint is the most prone to dislocation. Fractures of fourth and fifth metacarpal base often occur in conjunction with dislocations or subluxations.



Case 1-46. Fourth and fifth CMC fracture-dislocation. PA, oblique, and lateral views of the wrist. There is dorsal dislocation of the 5th cmc joint and fracture at base of the fourth metacarpal. Fractures of fourth and fifth metacarpal base often occur in conjunction with dislocation or subluxation.



Case 1-47. First CMC dislocation. PA, oblique and lateral views of the wrist. There is dorsal and lateral dislocation of the first metacarpal at the CMC joint. Pure dislocation of the first CMC joint is rare. Longitudinal force along the long axis of the metacarpal during flexion of CMC joint results in tear of the dorsal capsule and necessitates open reduction with repair of the ligament [15].


Case 1-48. Second CMC dislocation. PA and oblique views of the hand. The base of the second metacarpal (black arrows) overlaps the trapezoid bone, indicating that their normal articulation has been disrupted.

Lateral view of the hand shows the normal articulation between the trapezium and the first metacarpal, but no articulation between the trapezoid and the second metacarpal. There is an empty space (white arrow) where the second metacarpal should articulate with the trapezoid. The second metacarpal overlaps the third and fourth on this view, indicative of dorsal dislocation. Dislocation of the 2nd CMC joint is rare.

Case 1-49. Dislocation of the third CMC and scaphoid-trapezoid-trapezium joints. PA view of the hand. Percutaneous pinning was performed for 4th and 5th CMC joint dislocations, but the accompanying dislocations of the third metacarpal from the capitate and of the trapezoid and trapezium from the scaphoid were unrecognized at the time of surgery. This complex injury was sustained in a motorcycle crash.



Case 1-50. Multiple CMC joint dislocations. PA, oblique, and lateral view of the wrist. There are comminuted intra-articular fractures of the bases of the fourth and fifth metacarpals, with the fragments of the articular surfaces overlying the hamate. The bases of the second and third metacarpals overly the distal carpal row on the AP and oblique views. On the lateral views, the dislocated second through fifth metacarpal bases (arrow) may be seen dorsal to the carpal bones. This injury was sustained by a pedestrian who was struck by an automobile.



Case 1-51. Partial amputation through the CMC joints. PA, oblique, and lateral view of the hand. There is gross diastasis of the second through fifth CMC joints, with small sharply marginated fragments. The dorsal soft tissues are swollen. This injury was sustained in an industrial setting. All of the extensor tendons to the fingers were severed in the injury.


Case 1-52. Sesamoid fracture. Lateral view of the thumb. Magnified image shows sesamoid fracture (arrow) at the thumb MCP. Transverse fracture of sesamoid occurs form direct impact or hyperextension injury. Differentiation from a bipartite sesamoid can be made on the basis of non-corticated edges.


Case 1-53. Gunshot wound. AP and Lateral views of the hand. There are multiple uniform size and shaped metallic densities consistent with birdshot. There are multiple mildly displaced fractures involving the distal radius and ulna, the second through fifth metacarpals, and the proximal phalanges of the middle and ring fingers. Presumably, there are multiple carpal bone fractures, but these are largely obscured by the metal pellets. Shotgun pellets spread out as they travel away from the muzzle, unlike high-velocity missile projectiles such as rifle bullets, thereby causing a larger potential area for injury. Close range shotgun wounds can be fatal and cause as much damage as high velocity rifles. Factors that also play a role in severity of injury also include size and weight of pellets, with pellets over 0.14 inches in diameter (American standard birdshot size 2 and greater) causing more serious injuries [17].



Case 1-54. Blast injury. AP, oblique, and Lateral views of the hand and forearm. The hand has been completely destroyed, with large and small fragments of the digits and distal carpal bones overlying the proximal wrist and forearm. The soft tissues are largely obscured by a bulky dressing that was placed in the field. Holding an explosive device in a tightly closed fist would be the expected mechanism for a severe injury like this, but the patient could not remember what happened. The absence of metal fragments is indicative of a non-military device.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree