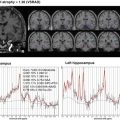
Fig. 15.1
Example of differences between MR image qualities. (a) Good quality image, (b) blurring artifact around frontal gyrus, (c) poor SNR
Moreover, several preprocessing steps such as geometrical distortion correction and intensity inhomogeneity correction are needed to improve the reliability of structural analysis. Intensity nonuniformity is caused by poor radio frequency coil uniformity, eddy currents, and insufficient sensitivity of the receiving coil. This issue has little impact on the visual diagnosis, but in automatic segmentation techniques, it can significantly degrade the reliability of these results [5]. Geometrical distortion is generated by gradient nonlinearity, nonuniformity of the static magnetic field, and distribution of magnetic susceptibility. The geometric distortions in MR images significantly degrade the reliability and precision of volumetric or morphometric measurements because their property can be changed by MRI manufacturer and time variation. This section introduces intensity nonuniformity correction methods, B1 correction [6] and nonparametric nonuniform intensity normalization [5], and distortion correction methods, Grad-unWarp [7] and phantom-based distortion correction [8].
15.2 Quality Control
It is important to use MRI data obtained with consistent scan parameters and on the same scanner to guarantee the reliability of the image analysis in longitudinal studies. Prior to the study, the site must pass the site qualification. Site qualification includes an examination in which a human volunteer is scanned twice at 1- or 2-week intervals with the study approved sequences loaded by a site local service engineer. The quality control team reviews human scans for the consistent scan parameters and good image quality between two sessions. If the human scan does not pass the review, the quality control team will ask to re-scan the human volunteer. After completely passing the review, the quality control team will provide site qualification. The quality control team will check whether the scan parameters satisfy certain scan protocols at each scan because image quality is dependent on the scan parameters, for example, field of view (FOV), slice thickness, transmit and receiver coil type, acquisition sequence, and software version (protocol check).
MRI has shown much promise as a biomarker of quantifying AD and other dementia progressions using morphometric or volumetric measurement of the brain atrophy [4]. However, its reliability and reproducibility depend on the image quality. The imaging artifact also affects image quality. So the image quality must be checked and handled to enhance standardization across sites and platforms and the reproducibility of longitudinal image analysis (image quality check).
In this section, we explain how to conduct image quality control. Each scan obtained from multiple imaging centers must be reviewed by the quality control team at the central data center. The quality control team ensures the scan protocol consistency and checks image quality in the acquired images. Moreover, a neuroradiologist checks the image data to identify any clinically significant findings. In the next section, we will describe the details of the consistency, image quality, and clinically significant findings of the checking protocol.
15.2.1 Protocol Check
Most of the clinical image data were contained in digital imaging and communications in medicine (DICOM) format. In 1982, the American College of Radiology (ACR) and the National Electrical Manufacturers Association (NEMA) formed a committee to develop DICOM standards for the interconnection of digital imaging devices [9]. The DICOM files contain information regarding the imaging scanners such as manufacturer name, scanner model name, modality type, and acquisition parameters in the DICOM TAG field. The quality control team checks the imaging parameters and, if not consistent with site notification, then contacts the Clinical Research Coordinator (CRC), technologist and site principal investigator, to notify them of imaging failure and ask for a repeat scan as soon as possible. Table 15.1 shows an example of DICOM TAG for checking the imaging parameters. For some parameters such as repetition time, echo time, field strength, and others, checks in rounded values are permitted. Especially, when the machine manufacturer or model is changed, the reproducibility of the imaging analysis is extremely degraded, and so the quality control team must check the machine change.
Table 15.1
DICOM TAG list for checking imaging parameters
DICOM TAG | Description |
|---|---|
(0008, 0070) | Manufacturer |
(0008, 0080) | Institution name |
(0008, 103e) | Series description |
(0008, 1090) | Model name |
(0018, 0023) | MR acquisition type |
(0018, 0050) | Slice thickness |
(0018, 0080) | Repetition time |
(0018, 0081) | Echo time |
(0018, 0082) | Inversion time |
(0018, 0083) | Number of averages |
(0018, 0087) | Magnetic field strength |
(0018, 0088) | Spacing between slices |
(0018, 0091) | Echo train length |
(0018, 0093) | Percent sampling |
(0018, 0094) | Percent phase fov |
(0018, 0095) | Pixel bandwidth |
(0018, 1000) | Device serial number |
(0018, 1020) | Software version |
(0018, 1100) | Reconstruction diameter |
(0018, 1250) | Receiving coil |
(0018, 1310) | Acquisition matrix |
(0018, 1312) | Phase encoding direction |
(0018, 1314) | Flip angle |
(0019, 107e) | Number_of_echoes |
(0021, 1057) | Locs_per_slab |
(0025, 1007) | Images_in_series |
(0028, 0030) | Pixel spacing |
15.2.2 Image Quality Check
Numerous artifacts in MR images that are not present in the original imaged object may be caused by improper technical operation of the imaging, while at other times they may be a consequence of natural processes or properties of the human body. Subject motion during the scan generates artifacts by inducing phase errors in the MRI signal. These artifacts can be classified into two types, blurring and ghosting artifacts. Blurring artifacts are produced by random movements, mainly in the phase-encode direction. Periodic motion associated with the movement of the lower jaw, eye, and the nasal cavity creates ghosting artifacts. Flow artifacts are caused by blood flow or fluids in the body. Fourier transform from a finite sampled signal causes truncation or gibbs artifacts as parallel lines adjacent to high-contrast borderline. Magnetic susceptibility within the internal magnetization of a tissue also causes artifacts due to interactions with an external magnetic field. Two different magnetic susceptibilities between air and tissues and/or metal and tissues cause local distortions in the magnetic field. Especially metal objects in the subject cause large distortions and significant susceptibility artifacts which result in a loss of signal in the image (metal artifacts). In normal MRI scanning, warp-around (aliasing) artifact occurs when FOV is smaller than an imaging object. The quality control team checks each MR image, and if any image does not have good quality, the quality control team recommends re-scanning. However, if the image quality will not be improved if the scan imaging is repeated, the protocol deviation must be logged or the image data have to be excluded. Checking items will be mentioned below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree