Head And Neck Cancer, Non-Squamous
Todd M. Blodgett, MD
Alex Ryan, MD
Marios Papachristou, MD
Key Facts
Terminology
Neuroendocrine tumors (NET), small cell undifferentiated carcinoma, Merkel cell carcinoma (MCC)
Benign mixed tumors (BMT) or pleomorphic adenoma; Warthin tumor; parotid carcinoma (mucoepidermoid and adenoid cystic), primary lymphoma
Imaging Findings
FDG PET overall sensitivity for all NET approximately 76%
MCC
FDG PET usually shows intense uptake within primary and metastatic lesions for MCC
For non-MCC NET, FDG may show variability
Some head and neck NET may show very little FDG activity
Salivary
PET: Sensitivity and specificity 75% and 67%
30% false positive rate for malignancy (mostly due to Warthin tumor)
PET/CT may be used to find primary in NSCCHN metastases
Top Differential Diagnoses
Metastatic Disease from Small Cell Carcinoma of the Lung
Benign Mixed Tumor or Pleomorphic Adenoma
Warthin Tumor
Parotid Metastases
TERMINOLOGY
Abbreviations and Synonyms
Non-squamous cell cancer of the head and neck (NSCCHN)
Neuroendocrine tumors (NET), small cell undifferentiated carcinoma, Merkel cell carcinoma (MCC)
Benign mixed tumors (BMT) or pleomorphic adenoma; Warthin tumor; parotid carcinoma (mucoepidermoid and adenoid cystic), primary lymphoma
Definitions
Heterogeneous group of tumors of neuroendocrine origin
Merkel cells first described by Frederick Merkel in 1875
Believed to be slow-acting mechanoreceptors in the basal layer of the epidermis
Provide information about touch and hair movement
Tumors of the parotid and submandibular glands (salivary glands)
IMAGING FINDINGS
General Features
Best diagnostic clue
MCC: Aggressive cutaneous mass
NET: Mass involving the structures listed below
Salivary: Negative Tc-99m pertechnetate and positive FDG PET
Location
MCC: Sun-exposed skin (head and neck 50%), most common location periorbital area; about 40% occur along the extremities
MCC is thought to arise from hair follicles or dermal Merkel cells, although no definite evidence exists
NET: Salivary glands, larynx, sinonasal cavity, upper esophagus, and oral cavity for non-MCC NET tumors
Most salivary gland tumors arise within the parotid gland
Most parotid gland tumors are benign
Size: Range in size from a few millimeters to several centimeters; average size < 2 cm
Morphology: MCC: Firm violaceous or reddish nodular papule or plaque ± ulceration
Imaging Recommendations
Best imaging tool
CT scan with contrast or PET/CT with contrast
FDG PET likely helpful in MCC; other head and neck NET may have less FDG activity
FDG PET overall sensitivity for all NET approximately 76%
FDG PET may influence management in up to 25% of patients
Salivary: Combination FDG PET or PET/CT and salivary gland scintigraphy with Tc-99m pertechnetate
Protocol advice: IV contrast for CT; arms down for PET or PET/CT
Additional nuclear medicine imaging options
Radiolabeled octreotide not well-evaluated for NET tumors of the head and neck; better for evaluation of NET outside the head and neck
Correlative imaging features
CT findings
Primary lesion may show necrosis, enhancement, or mass effect for both MCC and non-MCC NET
Lymphadenopathy range 1.2-11 cm; mean 4.2 cm
Nuclear Medicine Findings
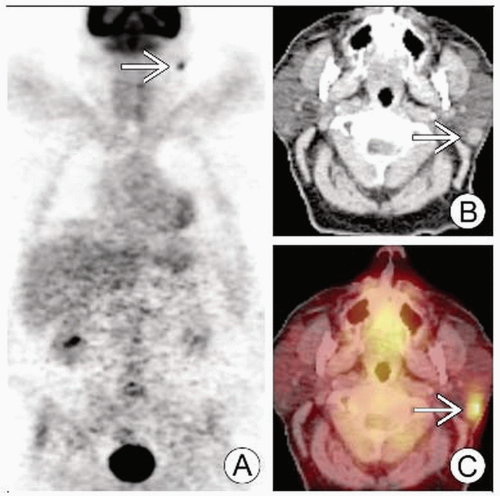
MCC
FDG PET usually shows intense uptake within primary and metastatic lesions for MCC
Average SUV max in one study 10.4
Several case studies and small series showing most MCC to be intensely FDG avid; occasional false negative
PET useful for staging, assessing tumor response, and surveillance
For non-MCC NET, FDG may show variability
Some head and neck NET may show very little FDG activity
Metastatic lesions may show photopenia compared to background normal activity
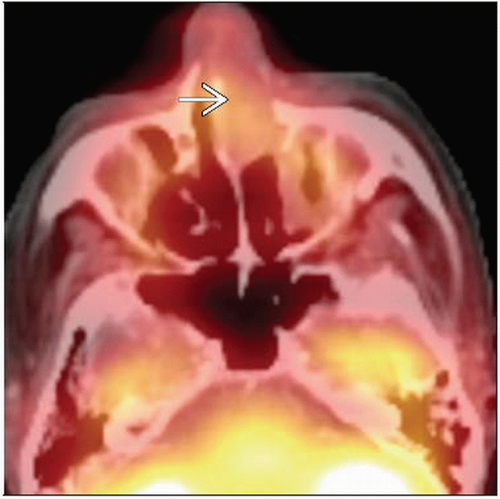
Salivary
PET: Sensitivity and specificity 75% and 67%
30% false positive rate for malignancy (mostly due to Warthin tumor)
High grade salivary tumors have been described as having wide range of maximum SUV values
In general, high grade salivary tumors have SUV greater than 5.0
Exception is adenoid cystic carcinoma, whose low SUV is attributed to slow growth
Normal salivary glands may have minimal to moderate uptake and diffuse asymmetric uptake
Mean SUV of normal parotid in one study was 1.9 ± 0.68
76% of patients in one study had asymmetric uptake, attributed to normal variance or inflammation
Some asymmetric appearances may be due to artifact secondary to head movement between emission and transmission scans
Tilted head position can also create appearance of asymmetry
PET and PET/CT show low accuracy for distinguishing between benign and malignant tumors due to high uptake of benign tumors
Inability to distinguish low grade malignant tumors from benign disease may have little clinical impact
Patients with low grade salivary cancer appear to show good prognosis after conservative treatment, similar to patients with benign salivary tumors
Overall major impact in clinical treatment planning is seen in 40% of patients
Staging
PET/CT may be used to find primary in NSCCHN metastases
Most primaries are located in thorax, head/neck, abdomen
In patients with high grade salivary cancer, PET/CT has been shown to
Significantly improve diagnostic accuracy for evaluating extent of tumor and tumor stages compared with CT alone
Superior for detection of cervical lymph node mets, distant mets, and second primaries
PET has been shown to have significant impact on management of patients with salivary gland cancers for initial staging and restaging
PET/CT provided correct staging in 85% of cases vs. 62% with CT
Whole-body scan superior to conventional imaging for detection of distant mets
Additional nuclear medicine options
MCC: Octreotide scan using somatostatin analog tagged with indium-111 as tracer used to detect metastases
Limited in assessing uptake in organs with physiologic uptake of octreotide such as liver, kidneys, spleen
Liver is one of the main sites of metastasis for MCC
Ga-67 scintigraphy: Sensitivity and specificity for differentiation of benign from malignant parotid masses 58% and 72% respectively
F-DOPA PET also shows some variability in the uptake
CT Findings
Criteria for malignant cervical lymph nodes
Presence of necrosis
Peripheral fatty hilum
Morphologic imaging generally poor for differentiating benign from malignant parotid tumors
Characteristics such as irregular margins and infiltration into parenchyma useful but not reliable
DIFFERENTIAL DIAGNOSIS
Melanoma
Primary MCC usually more red in color
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree