, Sugoto Mukherjee2, J. Jared Christophel3, Max Wintermark4 and Prashant Raghavan5
(1)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(2)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(3)
Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health Systems, Charlottesville, VA, USA
(4)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(5)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Abstract
The overwhelming majority of craniofacial traumatic injuries however are caused by motor vehicle accidents with about 70 % of these including some type of facial injury. The objectives of this chapter are to review the standard imaging techniques used to evaluate craniofacial trauma, discuss the various patterns of facial fractures with emphasis on the pertinent findings and relevant anatomical considerations, and finally present some special considerations pertaining to pediatric patients.
10.1 Introduction
The overwhelming majority of craniofacial traumatic injuries however are caused by motor vehicle accidents with about 70 % of these including some type of facial injury. The objectives of this chapter are to review the standard imaging techniques used to evaluate craniofacial trauma, discuss the various patterns of facial fractures with emphasis on the pertinent findings and relevant anatomical considerations, and finally present some special considerations pertaining to pediatric patients.
10.2 Imaging Evaluation
Plain films no longer play a significant role in evaluating craniofacial trauma. Facial injuries are best evaluated by CT using 1.25 mm or thinner images through the face. Images should include both soft tissue and bone algorithms, with coronal and sagittal reformatting. While axial, coronal, and sagittal images are sensitive at identifying fractures, 3D reconstructions play a significant role in surgical planning and should be made available.
First, the skin and soft tissues are inspected; traumatic soft tissue findings will direct the radiologist to more closely examine the adjacent deeper structures. The superficial bony structures are evaluated next, followed by the deeper bony structures. Finally, it is useful to consider typical fracture patterns and areas that are easy to miss, including the lamina papyracea, orbital rims and floor, nasolacrimal duct, carotid canal, temporal bones, and orbital apex. The craniocervical junction is often included on these examinations, and it is important to evaluate the occipital condyles and the atlas and axis vertebra and their joints.
10.3 The Facial Buttress Concept
The facial buttress concept describes the regions of thicker bone that provide structural support to the facial skeleton. The buttresses play key roles in maintaining facial stability (e.g., with mastication) and appropriate midface projection. Accordingly, repair of fractured buttresses is crucial to maintain form and function of the face, orbits, sinuses, nose, and teeth. As they have sufficient bone thickness to accept screws and anchor titanium plates, the buttresses are a focus of surgical planning for fracture repair. The strongest buttresses are vertically oriented: the medial nasomaxillary buttress and the lateral zygomaticomaxillary buttress (Fig. 10.1). The pterygomaxillary buttress has also been described but is less commonly addressed in fracture repair. The horizontal buttresses are weaker and include the superior orbital rims and frontal bones superiorly, the inferior orbital rims and nasal bones across the midface, and the maxillary alveolus and hard palate inferiorly (Fig. 10.1).
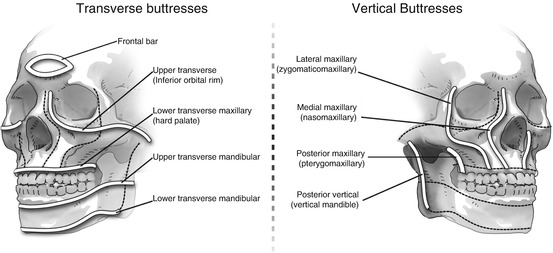
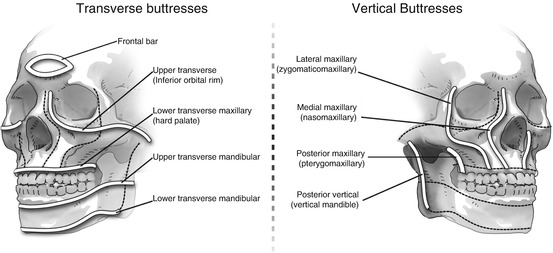
Fig. 10.1
Facial buttress graphic. The facial buttress system is divided into vertical and horizontal buttresses. As shown in the above figure, the vertical buttresses run on the medial and lateral aspects of the maxillary sinus/orbits and mandible, whereas the horizontal buttresses run below the orbits, above and below the teeth, and at the bottom of the mandible
10.4 Fracture Patterns
10.4.1 Nasal Fractures
The nasal bones are the most commonly fractured bones of the face. The nasal bone is thicker cephalically and becomes progressively thinner inferiorly. Eighty percent of nasal fractures occur within the thinner portion below the intercanthal line (axial line connecting the orbital rims at the level of the lateral canthi). The most common pitfall is confusing a suture line for a nasal fracture (and vice versa). Confusion is most frequently centered around the so-called high defect (thinning of the nasal wall) and low defect (nasomaxillary suture). Most nasal fractures occur in the transverse plane, while normal sutures and nasociliary grooves are longitudinally oriented and do not cross the midline; lucencies that cross the midline are fractures. Additionally, short lucent lines that reach the anterior cortex of the nasal bone, regardless of displacement, should be considered nasal fractures (Fig. 10.2).


Fig. 10.2
Nasal bone anatomy. The nasofrontal and nasomaxillary sutures and the groove for the nasociliary nerve are common mimics of nasal fractures. A lucency inferior to the nasofrontal suture should not cross the midline
The nasal bones comprise only one third of the structural support of the nose; the majority of the nasal structure is cartilage which can also be injured. Cartilaginous fractures can result in perichondrial separation resulting in hematoma formation. Cartilage hematomas interfere with native blood supply to the cartilage and can result in necrosis, infection, and long-term saddling of the nose. The radiologist should always evaluate the nasal septum for localized septal swelling or traumatic deviation. A septal hematoma can result in sclerotic septal distortion and disordered or obstructed airflow, or it can become a nidus for infection (Fig. 10.3). To avoid these complications, septal hematomas require prompt evacuation (Box 10.1).
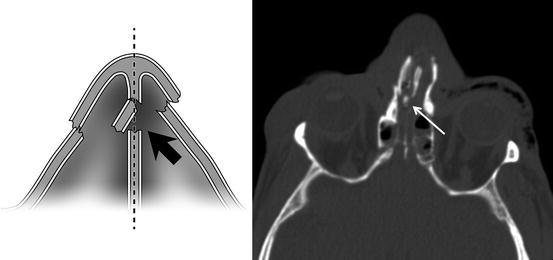
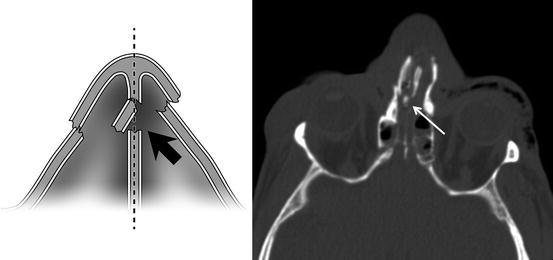
Fig. 10.3
Nasal septum fracture. In the setting of nasal trauma, it is important to identify traumatic deviation of the nasal septum (white arrow), and any associated soft tissue hematoma.
10.4.1.1 Box 10.1. Nasal Bone Fractures: Pearls and Pitfalls
Don’t confuse the high and low defects for fractures
Old or new? Remote fractures may mimic a recent fracture; look for soft tissue swelling
Most nasal bone fractures occur in the transverse plane
The nasociliary groove does not cross the plane of the nasal bone; but a fracture can
Look at the nasal septum to identify signs of septal hematoma (localized septal swelling or traumatic deviation)
10.4.2 Naso-Orbital-Ethmoid (NOE) Fractures
Naso-orbital-ethmoid (NOE) fractures involve the nasal bones, the ethmoid sinuses, and the medial orbital rims. This type of fracture tends to disrupt the confluence of the medial maxillary buttress with the upper transverse maxillary buttress (Fig. 10.4). Classically, the anterior nasal structures are displaced posteriorly into the lacrimal bones and ethmoid sinuses.
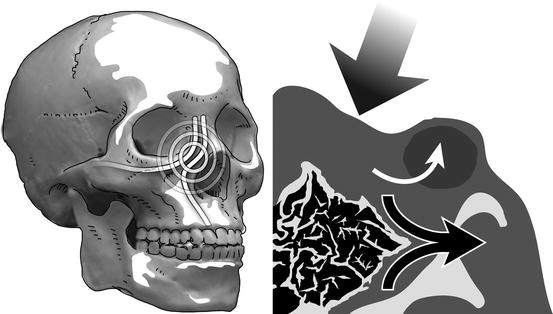
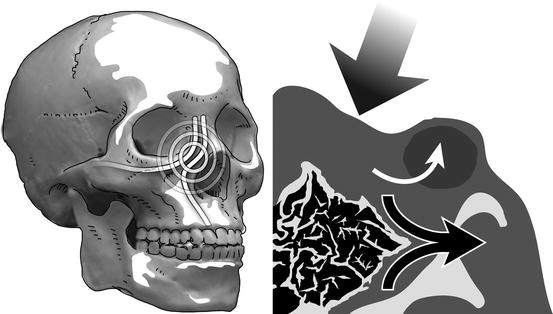
Fig. 10.4
NOE fracture. Posterior displacement of the anterior nasal bony structures can result in lateral displacement of the medial orbital walls causing proptosis
A key finding in NOE fractures is an increased distance between the medial orbital walls and the attachments of the medial canthal tendons (MCTs, which arise from the anterior and posterior lacrimal crests) (Fig. 10.5). Splaying of the medial orbital walls will result in telecanthus and malposition of the globes. Grading of NOE fractures depends on the status of the MCT: grade I involves MCT attachment to a large bone fragment of the lacrimal fossa; grade II demonstrates multiple smaller comminuted fragments; and grade III indicates avulsion of the MCT. Often accurate grading requires physical exam and/or intraoperative assessment (Fig. 10.6).
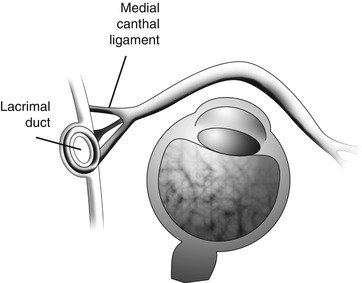
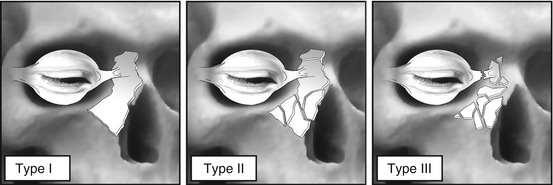
Fig. 10.5
Medial canthal ligament anatomy. The medial canthal ligaments are not visible on CT. However, their bony attachments anterior and posterior to the lacrimal crest can be identified
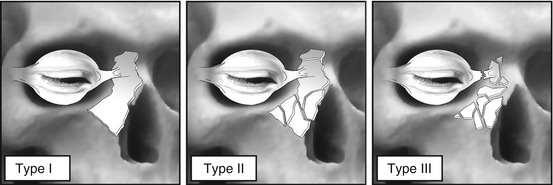
Fig. 10.6
Manson classification. The Manson system classifies NOE fractures based on the medial canthus. In type 1, the fractured piece is large and the insertion of the medial canthal ligament around the lacrimal fossa is intact. In type II, there is a comminuted fracture of the buttress and the canthus is attached to a small bone fragment. In type III, there has been avulsion of the ligament from its osseous insertion. The distinction between type II and type III cannot be done with imaging and requires physical exam
NOE fractures are commonly associated with frontal sinus fractures. Injury to the frontal sinus outflow tract (FSOT) may lead to formation of adhesions, obstruction, and subsequent frontal mucocele (Fig. 10.7). If the FSOT is involved, a frontal sinus obliteration procedure may be required (Box 10.2).
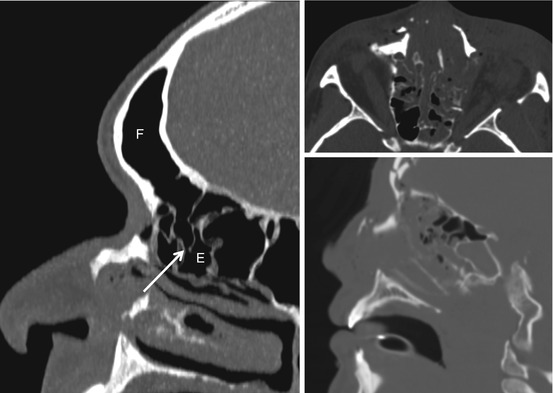
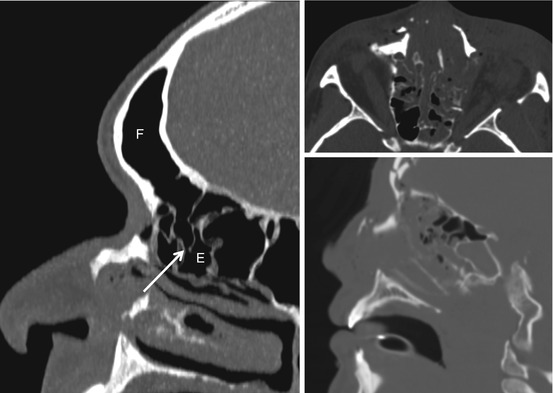
Fig. 10.7
Frontal ethmoid sinus drainage. The above image demonstrates the drainage pathway (arrow) between the frontal sinus F and the ethmoid sinuses E. A fracture that disrupts this drainage can predispose the patient for frontal sinus mucocele formation
10.4.2.1 Box 10.2. Naso-Orbital-Ethmoid (NOE) Fractures: Checklist
Evaluate for a fracture of the medial orbital wall in the region of the nasal lacrimal duct If present, is the fracture fragment large or comminuted?
Assess the distance between the two lacrimal fossae in the coronal plane, to identify a potential deformity that requires repair
Evaluate for disruption of the nasofrontal drainage pathways
10.4.3 Frontal Sinus Fractures
In general, fractures through sinus walls tear mucosa and produce hemorrhage; thus, in the acute phase, the absence of free fluid in a sinus cavity excludes a fracture. When the frontal sinus is fractured, only the anterior table is disrupted in approximately two thirds of cases. Repair for these is considered in the setting of cosmetic deformity. The implications are much more significant when the posterior table is involved; in this case, the degree of posterior table displacement and amount of pneumocephalus must be reported, as these are the indications for surgical repair. Posterior table fractures are associated with CSF leaks, meningitis, and traumatic brain injury. As discussed above, the status of the FSOT should be reviewed.
10.4.4 Orbital Fractures
10.4.4.1 Inferior Blowout Fracture
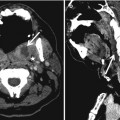
“Blowout” fractures occur as the result of a direct blow to the orbit by an object that is too large to enter the orbit. The force of the blow is absorbed by the thick orbital rim and is transmitted to the thin orbital floor. Alternative theories describe force transmitted through the globe to the orbital floor which is the path of least resistance in the orbit. The typical result is a fracture of the middle third of the orbital floor near the infraorbital canal; the orbital rim remains intact. (By strict definition, if the orbital rim is fractured, the floor fracture cannot be referred to as a “blowout.”) An important complication of orbital floor disruption is orbital entrapment. While the diagnosis of entrapment can only be made on physical exam, noting herniation of orbital fat, the inferior rectus muscle, or the inferior oblique muscle through the orbital floor is strongly suggestive. An abrupt kink in the herniated muscle as opposed to a smooth prolapse through the site of fracture is convincing evidence of entrapment. If the inferior rectus muscle remains flattened in cross section and in the correct position, the fascial sling is likely intact. Alternatively, if the muscle is round in cross section and inferiorly displaced, the fascial sling is likely disrupted increasing the likelihood of entrapment. Rounding of the inferior rectus is associated with development of enophthalmos with nonoperative treatment, and reporting of height-to-width ratio of this muscle can be useful in treatment planning. Regardless of imaging findings, an ophthalmologic exam is recommended for all orbital injuries and is critical to evaluate for entrapment; this is particularly true in the pediatric setting (Fig. 10.8).
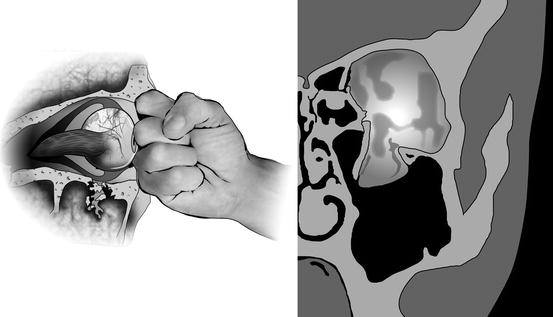
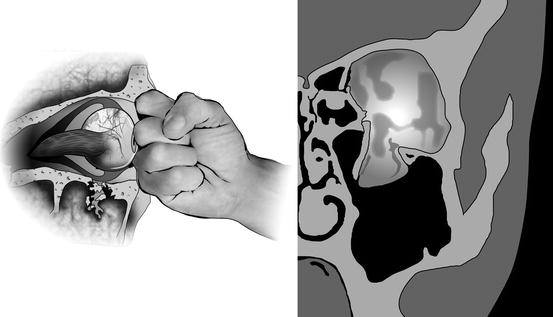
Fig. 10.8
Blowout facture. The above diaphragm demonstrates inferior displacement of the inferior orbital floor with some herniation of intraorbital fat. The inferior rectus muscle normally has a flat appearance. A more rounded appearance can be seen with a contused muscle and can raise suspicion for entrapment
10.4.4.2 Medial Blowout Fracture
Fractures of the lamina papyracea can be very subtle. Orbital emphysema in the absence of an obvious fracture of the orbital roof or floor suggests a medial wall fracture. Herniation of orbital fat and entrapment of the medial rectus muscle may occur through the fracture defect. If the fracture results in loss of the posterior medial orbital bulge (Fig. 10.9), the normal bony orbital volume will be increased and enophthalmos can result; this is actually the most common cause of enophthalmos.
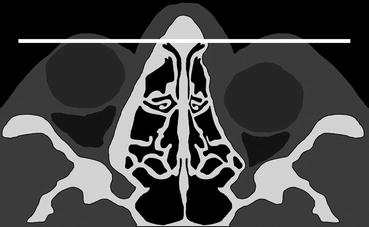
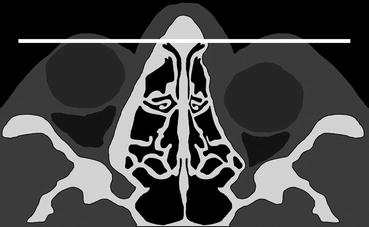
Fig. 10.9
Medial orbital bulge. The above diaphragm demonstrates loss of the normal orbital bulge, compared to the normal contralateral contour. This expands the orbital volume and can cause enophthalmos
10.4.4.3 Orbital Roof and Blow-In Fractures
Fracture of the orbital roof is more common in the pediatric population (see below). However, this fracture still occurs in the adult population and is frequently associated with frontal sinus and skull base fractures, dural tears, intracranial hemorrhage, and meningoencephaloceles. When orbital roof fractures demonstrate inferior displacement of fracture fragments into the soft tissues of the orbit, they are called “blow-in” fractures. While ocular injury is uncommon with “blowout” fracture, it has been reported in 14–29 % of patients with blow-in fractures.
10.4.4.4 Orbital Apex Fractures
Fracture of the orbital apex is rare and can be associated with optic nerve impingement. When this fracture is identified, it is important to evaluate for a retrobulbar hematoma and for a bone fragment impinging on the optic nerve. It is critical to realize that even a small fracture can cause nerve injury (Fig. 10.10) (Box 10.3).
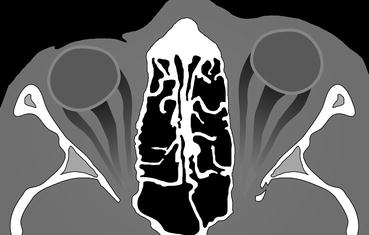
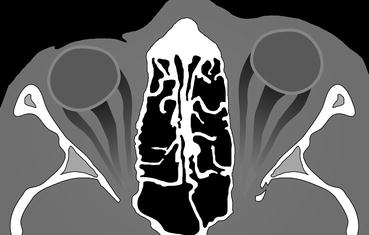
Fig. 10.10
Orbital apex fracture. The above diaphragm demonstrates how subtle a fracture involving the orbital apex can be. In the setting of trauma, careful scrutiny of this area is important because of the potentially devastating complication to the optic nerve and vessels
Box 10.3. Globe Trauma: Checklist
Evaluate the anterior chamber. Increased attenuation = hyphema. Decreased depth = corneal laceration or anterior subluxation. Increased depth is associated with open globe injury
Evaluate the lens. Remember it is usually dislocated posteriorly (but can be anteriorly)
Evaluate the posterior globe. Look specifically for blood or evidence for retinal or choroidal detachment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree