Fig. 8.1
Female pelvic anatomy at the midpelvis plane
If the fetus is in vertex presentation and occiput anterior position, engagement in the birth canal usually occurs along the oblique diameter of pelvic inlet (13 cm), with the fetal occiput approaching the left iliopectineal eminence. After descent to midpelvis, the fetal head may not progress further down on this orientation due to the transverse narrowing caused by the above-mentioned ischial spines which would block head progression. Consequently, the head physiologically undergoes a movement of internal rotation approaching the pubis with the occiput and aligning its largest diameter (suboccipitobregmatic diameter 9.5 cm) with the widest diameter of the birth canal at the level of the midpelvis, which is in fact the anteroposterior (11.5 cm) (Fig. 8.2).
Fig. 8.2
Internal rotation movement of the fetal head at midpelvis plane
After the internal rotation, the head may now progress to the low pelvis and being finally delivered through a deflexion movement of the occiput below the pubic symphysis, which is the fulcrum of the movement itself [2].
The whole process of fetal head delivery has been the object of study of traditional obstetrics, and its detailed knowledge is based upon digital assessment of cephalic sutures and fontanels in respect of the landmarks of the birth canal. However, clinical evaluation of such findings particularly during the second stage of labor is commonly reported to be inaccurate and poorly reproducible [3].
First of all, the assessment of the occiput position in the birth canal by digital exploration has been consistently reported to be extremely inaccurate. Furthermore, the process of fetal head descent and rotation is suspected to follow different pathways depending on particular obstetric conditions, including persistent posterior occiput position, deflexion, or asynclitism. On this basis, the use of ultrasound in labor has been recently suggested in order to assist physicians in the assessment of fetal head rotation. The sonographic study combined with clinical findings may therefore refine the proper management of labor, particularly when an expedite delivery is indicated and the correct choice between a cesarean section and an operative vaginal delivery is warranted.
8.2 2D Ultrasound and Fetal Head Position: The Occiput Posterior
Intrapartum assessment of the fetal head position and rotation is of paramount importance and is traditionally based upon digital palpation of the posterior fontanel and sagittal suture and their correlation with specific landmarks of the maternal birth canal. In accordance with the aforementioned mechanism of physiologic vertex delivery, the degree of fetal head rotation in respect of the maternal pelvis may indirectly witness the level of fetal head descent in the birth canal.
However, the dynamics of labor may at times be altered by mechanic conditions which may affect the course of labor, interfering with fetal head progression in the birth canal. Among these conditions, a persistent posterior position of the fetal occiput in the birth canal is widely acknowledged and is considered the commonest fetal head malposition in labor.
Occiput posterior position is encountered in 5–15% of all deliveries [4, 5], but a significantly higher prevalence is described in the first stage of labor. In several cases, spontaneous conversion to an anterior occiput position has been demonstrated to occur [6], but this chance becomes much smaller in fetuses with persistent occiput posterior position in the advanced second stage. In this latter group, a high risk of cesarean section or operative vaginal deliveries is consistently reported and a globally increased incidence of maternal and perinatal complications is widely acknowledged [5, 7].
Accurate diagnosis of persistent occiput posterior position in the second stage of labor has therefore a critical role in the appropriate management of labor. Furthermore, correct determination of the head position is crucial before instrumental delivery. An error in such evaluation may result in inappropriate vacuum or forceps blade placement, both increasing the risk of fetal injury and or the failure rate of the instrumental procedure [8–10]. Failed instrumental delivery followed by cesarean section is associated with an increased decision-to-delivery interval and with a much increased risk of fetal trauma [11–13].
Lastly, some preventive measures can be undertaken in cases of cephalic malposition, as mediolateral episiotomy in occiput posterior position has been found to reduce significantly the risk of anal sphincter damage [14, 15].
However, digital examination is highly subjective, and using a birth simulator, some authors have independently shown that clinical diagnosis of occiput position was inaccurate in a relevant proportion of cases [3].
In this respect, an overt superiority of ultrasound vs. digital examination has been witnessed in the recent past. The exact position of fetal occiput in respect of the birth canal may be easily documented by suprapubic 2D ultrasound, using fetal orbits as the anatomic landmark (Fig. 8.3).
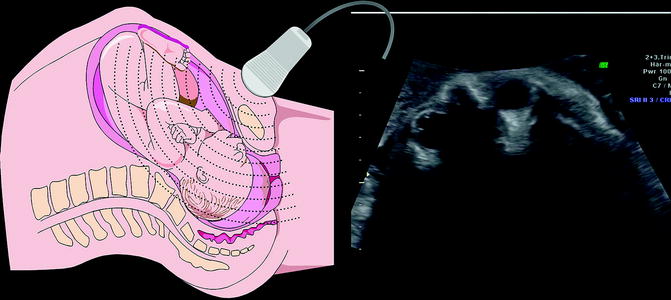
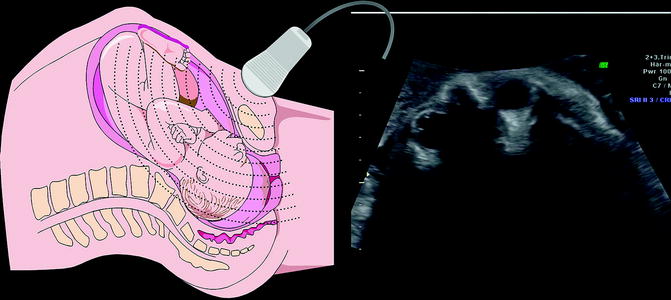
Fig. 8.3
Suprapubic 2D ultrasound, fetal orbits as the anatomic landmark of occiput posterior position
Furthermore, the orientation of the head midline and the degree of fetal head rotation may be also demonstrated at suprapubic or translabial ultrasound.
Using sonographic findings as the gold standard, some authors have demonstrated that digital examination is highly inaccurate with a rate of error ranging from 30% to 70% [6, 16–22] and significant error (>45°) ranging from 20% to 40%. Clinical evaluation is reported to be less accurate in cases of occiput posterior and transverse, when medical intervention is more likely to be needed [3, 17, 18, 20].
Reliability of digital assessment may be further decreased by the presence of caput succedaneum and molding, both of them more frequently associated with obstructed labor. Many authors have failed to demonstrate a significant difference in accuracy between experienced and inexperienced obstetricians [3, 18, 19], although this finding has been questioned by others [16].
Some authors [16] have assessed by suprapubic 2D ultrasound fetal head position just prior to instrumental delivery and demonstrated that digital examination during delivery fails to identify the correct fetal head position in about one quarter of cases.
At the light of these observations, in dubious cases or prior to the operative vaginal delivery, the use of 2D ultrasound to reassess clinical findings and confirm the occiput position would be highly recommended.
More recently, Blasi et al. have observed that among fetuses with occiput posterior in active labor, the persistence of posterior occiput position may be accurately predicted looking at fetal spine orientation. They have reported indeed a conversion to anterior occiput at delivery among almost all cases with anterior fetal spine and persistence of occiput posterior position among those with posterior fetal spine [23].
8.3 Fetal Head Rotation
In the second stage of labor, the degree of fetal head rotation in respect of anteroposterior axis of maternal pelvis is strongly related to the level of the presenting part in the birth canal. As mentioned above, in the commonest type of labor with a vertex presenting fetus, the internal rotation of the head at the level of ischial spines allows the head to pass from the mid- to the low pelvis just prior to delivery. The alignment of fetal head in comparison with obstetric conjugate is therefore a critical finding to assess the descent of presenting part and is traditionally investigated by digital examination of the sagittal suture.
However, clinical evaluation of this parameter is once more affected by low reproducibility, and in this respect, the use of 2D ultrasound to define the exact rotation of fetal head in the birth canal has been recently suggested.
Using the translabial approach, the transducer is placed transversally on the major labia. Subsequently, the echogenic line interposed between the two cerebral hemispheres (midline) is identified, and the angle formed by the midline and the anteroposterior diameter of the pubis is measured (so-called “midline” angle) as shown in Fig. 8.4.
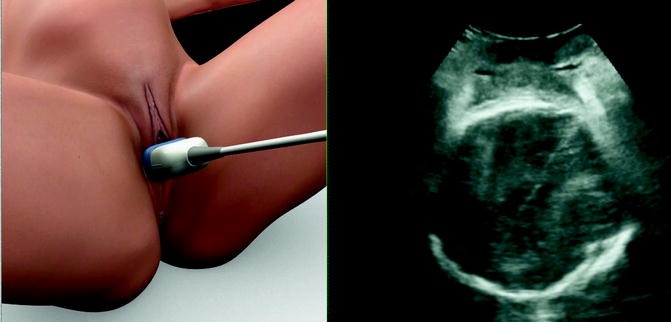
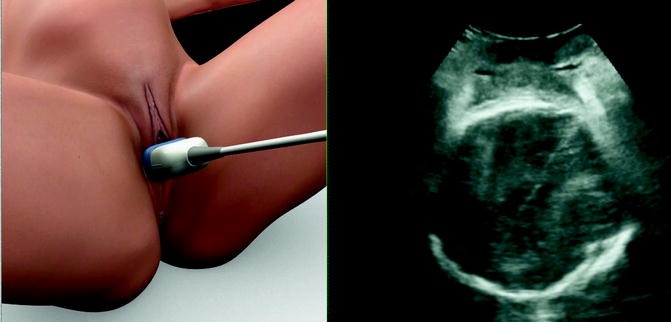
Fig. 8.4
Placing the transducer transversally on the major labia, the echogenic line interposed between the two cerebral hemispheres (midline) is identified, and the angle formed by the midline and the anteroposterior diameter of the pubis is assessed (so-called “midline” angle)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree