Heart
Angiocardiography
Diagnostic catheterization has largely been replaced by echocardiography (including transoesophageal echocardiography), radionuclide ventriculography and MR imaging. Angiocardiography is usually used as part of an interventional therapeutic procedure and can be performed simultaneously with cardiac catheterization during which pressures and oximetry are measured in the cardiac chambers and vessels that are under investigation. The right heart, left heart and great vessels are examined together or alone, depending on the clinical problem.
Indications
1. Congenital heart disease and anomalies of the great vessels – mostly in the paediatric population. Either for diagnosis or therapeutic procedures such as transcatheter closure of patent foramen ovale, atrial septal defect (ASD), ventricular septal defect (VSD) and patent ductus arteriosus.
2. Valve disease, myocardial disease and assess ventricular function. Balloon valvuloplasty and, in selected centres, transcatheter aortic valve implantation (TAVI) can be performed to treat stenotic valvular disease.
Contrast medium
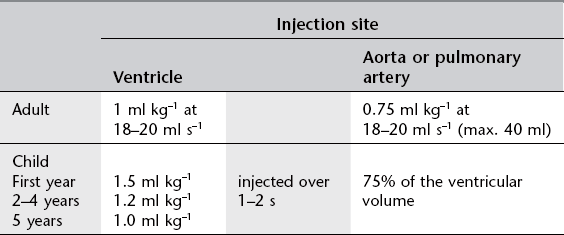
Low osmolar contrast material (LOCM) 370 mg I ml−1 (see Table 8.1).
Equipment
1. Biplane digital fluoroscopy and cine radiography with C-arms to facilitate axial projections
2. Pressure recording device
3. Electrocardiogram (ECG) monitor
4. Blood oxygen analyser
5. Catheter:
(a) For pressure measurements and blood sampling: Cournand (Fig. 8.1), 4–7F

Figure 8.1 Cournand catheter. End holes: 1 Side holes: 0.
(b) For angiocardiography: National Institutes of Health (NIH) (Fig. 8.2) or pigtail (Fig. 8.3), 4–8F.
Figure 8.2 National Institutes of Health (NIH) catheter. End holes: 0 Side holes: 4 or 6.

Figure 8.3 Pigtail catheter. End holes: 1 Side holes: 12.
Technique
1. Right-sided cardiac structures and pulmonary arteries are examined by introducing a catheter into a peripheral vein. In babies the femoral vein may be the only vein large enough to take the catheter. If an atrial septal defect is suspected, the femoral vein approach offers the best chance of passing the catheter into the left atrium across the defect. In adults the right antecubital or basilic vein may be used. The cephalic vein should be avoided as it can be difficult to pass the catheter past the site where the vein pierces the clavipectoral fascia to join the axillary vein. The catheter, or introducer, is introduced using the Seldinger technique. (The NIH catheter must be introduced via an introducer as there is no end hole for a guidewire.)
2. In children it is usually possible to examine the left heart and occasionally the aorta by manipulating a venous catheter through a patent foramen ovale. In adults the aorta and left ventricle are studied via a catheter passed retrogradely from the femoral artery.
3. The catheter is manipulated into the appropriate positions for recording pressures and sampling blood for oxygen saturation. Following this, angiography is performed.
Image acquisition
Using digital angiography at 7.5 frames s–1 with alignment to the anatomical axes of the heart, i.e. the X-ray beam is angulated relative to the axial planes of the heart rather the orthogonal planes of the body. The long axis of the heart is usually oblique to the long axis of the patient’s body and cardiac angiography suites have movable C-arms which allow correct positioning by movement of the equipment alone without disturbing the patient. Supplementary angulations of the X-ray beam from the cardiac axes are used to profile those areas of the heart under examination. Useful views are:
1. 40° cranial/40° left anterior oblique (LAO) (hepatoclavicular or four-chamber) view – the beam is perpendicular to the long axis of the heart and aligns the atrial septum and posterior interventricular septum parallel to the beam
2. Long axial 20° right anterior oblique (RAO) (long axial oblique) view – the lateral tube and image intensifier are angled 25–30° cranially, to align with the long axis of the heart, and 20° RAO.
Coronary arteriography
Indications
1. Diagnosis of the presence and extent of ischaemic heart disease
2. After revascularization procedures
3. Congenital heart lesions
4. Therapeutic percutaneous coronary intervention – balloon angioplasty and stenting.
Diagnostic arteriography can be supplemented by intravascular ultrasound (US) to determine the nature and extent of plaque within the vessel wall and, in some centres, with angioscopy. Pressure wire studies to determine fractional flow reduction (FFR) across stenoses prior to angioplasty/stenting can be performed; particularly useful in assessment of intermediate lesions.
Equipment
1. Digital angiography with C-arm
2. Pressure recording device and ECG monitor
3. Selective coronary artery catheters:
(a) Judkins (Fig. 8.4) or Amplatz (Fig. 8.5) catheters – the left and right coronary artery catheters are of different shape. These can be used for both femoral or radial approaches (usually utilizing smaller Judkins for the left coronary artery)
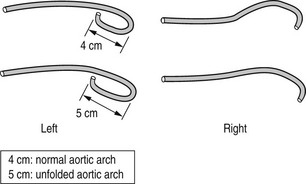
Figure 8.4 Judkins coronary artery catheters. End holes: 1 Side holes: 0.
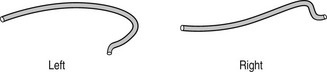
Figure 8.5 Amplatz coronary artery catheters. End holes: 1 Side holes: 0.
(b) Tiger II catheter (Fig. 8.6) – specifically designed for right radial approach. Single catheter used for both left and right coronary arteries (reduces procedure time, radiation exposure and less manipulation leading to less radial artery spasm)

Figure 8.6 Tiger II coronary artery catheter. End holes: 1 Side holes: 0.
(c) For assessment of grafts: Judkins, Simmons and others (for both femoral and radial approaches).
Technique
The catheter is introduced using the Seldinger technique via the radial (most commonly), brachial or femoral artery and advanced until its tip lies in the ostium of the coronary artery.
Image acquisition
Optimum visualization of vessels is obtained with images acquired perpendicular to the vessel under examination so multiple, compound projections using rotation around the patient axis as well as cranio-caudal angulations of the X-ray beam are utilized for each coronary vessel.
Angiography (7.5 frames s–1) is performed in the following projections:
(* though each projection will show good visualization of various segments of the other coronary artery).
Complications
In addition to the general complications discussed in Chapter 9, patients undergoing coronary arteriography may be liable to:
1. Arrhythmias – such as non-sustained atrial fibrillation with right heart catheterization or non-sustained ventricular arrhythmia with left ventriculography
2. Ostial dissection by the catheter
3. Access site complications (more commonly seen with femoral approach) – local haematoma, femoral artery pseudoaneurysm or arterio-venous fistula.
Cardiac CT
The rapid evolution of multi-detector CT scanner technology over the last 5 years has resulted in cardiac CT and coronary CT angiography becoming well-established techniques in the investigation and management of cardiovascular disease. Greater temporal resolution, sophisticated ECG-gating software and post processing algorithms and, very importantly, radiation dose-reducing strategies allow cardiac CT to be used widely. CT has a high accuracy in detecting coronary vessel stenoses and a very high negative predictive value in excluding significant disease.
Indications
1. Patients with known or suspected chronic coronary artery disease
2. Assessment of suspected anomalous coronary artery anatomy
3. As a screening test in symptomatic patients with typical chest pain but a low clinical probability of significant coronary artery disease
4. As a screening test in asymptomatic but high-risk patients or patients with atypical chest pain
5. Assessment of coronary artery grafts, including left internal mammary artery (LIMA) grafts
6. As an alternative to diagnostic coronary angiography when planning percutaneous angiographic intervention or as post-procedure follow-up.
7. Assessment of left atrium and pulmonary vein anatomy prior to electrophysiological studies and ablation.
Contraindications
Patient preparation
1. Avoid caffeine – this includes tea, coffee and caffeine-containing soft drinks (including ‘decaffeinated’ varieties), ‘energy’ pills and Viagra-type medication.
2. Drugs – patients should take all their normal cardiac medication as usual on the day of the test.
3. Thorough explanation of the procedure to the patient aids compliance, particularly with regard to breath-hold (suggest patient takes a ‘ breath’ when instructed – less likely to move during scan and avoids ‘Valsalva’ manoeuvre affecting contrast bolus entering chest).
breath’ when instructed – less likely to move during scan and avoids ‘Valsalva’ manoeuvre affecting contrast bolus entering chest).
4. 18G cannula in right antecubital fossa – siting cannula in right arm reduces artefact as contrast crosses the mediastinum. For graft studies this avoids streak artefact obscuring origin of LIMA grafts.
5. Assess suitability for administration of β-blockers and sublingual nitrates (see below).
Beta-blockers
Optimal imaging quality and radiation dose are significantly influenced by heart rate, which ideally should be between 55–65 bpm. With basic precautions and simple monitoring, safe and dose-titratable heart rate reduction can be achieved in the majority of patients using β-blocker administered within the radiology department. Metoprolol is commonly used and can be given orally or intravenously, or in combination.
• The patient may already be on oral β-blockers (either as regular medication or specifically prescribed by the referrer for the purposes of the examination). In most cases the scan can proceed without further medication.
• If the patient is not on β-blockers, requires heart rate reduction to optimize scan and has no contraindication to β-blocker administration, metoprolol can be given orally or i.v.
(Contraindications to β-blockade include heart failure, significant aortic stenosis, heart block, asthma/COPD, use of other antiarrhythmic medication including calcium channel blockers and digoxin.)
• Metoprolol 100 mg orally 1 h prior to scan. Pulse and blood pressure monitored regularly until heart rate reaches desired level. (If the heart rate does not reach a satisfactory level additional metoprolol can be given intravenously whilst the patient is on the scanner.)
• Metoprolol can be given solely in i.v. form (or to ‘top up’ oral dose where optimal heart rate has not been achieved with oral administration) just before the start of the scan with the patient on the scanner table. 5–30 mg i.v. given in aliquots of 5 mg titrated against heart rate.
Nitrates
Sublingual glyceryl trinitrate 400–800 µg (1–2 tablets) can be given a few minutes prior to scanning to produce coronary dilatation and improve image quality. Temporary effect of hypotension is unlikely to be an issue with the patient lying on the CT table and transient physiological elevation of heart rate usually resolves by the time of image acquisition. (Contraindications to nitrates include: hypotension, hypovolaemia, severe aortic valve stenosis, hypertrophic cardiomyopathy, recent MI, severe anaemia, recent ‘Viagra’-type medication.)
Technique
Cardiac CT remains a high radiation dose procedure and careful attention to dose reduction measures, whilst maintaining image quality, is essential. The use of ‘prospective’ rather than ‘retrospective’ scanning and, where possible, single heart beat acquisition reduce radiation dose very significantly.
Scan technique will be determined by the clinical question to be answered and by patient heart rate; the exact protocol will be determined by the manufacturer and model of the CT scanner.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree