and Linh T. Ho1
(1)
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Case 5.1
History
A 55-year-old man with recently diagnosed hepatocellular carcinoma (HCC) . PET-CT requested for staging.
Findings
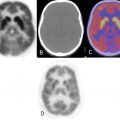
The small HCC is associated with focal enhancement at the dome of the liver on the contrast-enhanced axial image (Fig. 5.1a) but is not appreciated on the non-contrast-enhanced image (Fig. 5.1b). The HCC is not associated with hypermetabolism as shown on the fused PET-CT image (Fig. 5.1c) and the FDG PET image (Fig. 5.1d). Contrast-enhanced CT would be the follow-up study of choice since this HCC is not 18 F-FDG avid.
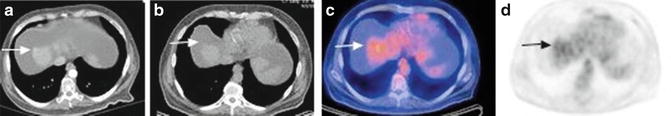
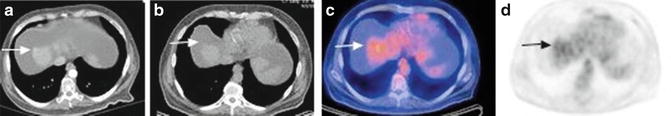
Fig. 5.1
Pearls and Pitfalls
The reported sensitivity of PET-CT for the detection of HCC is 55 % while for CT is 90 %, thus CT with IV contrast is the preferred study for diagnosis, staging, and restaging of HCC.
Hypermetabolism in the hepatic tissue adjacent to a lesion can be seen up to 3 months following transarterial chemoembolization as a reaction to the infarcted tumor.
Mild hypermetabolism in the parenchyma peripheral to the tumor occurs 2–3 days following radiofrequency ablation (RFA) . The recommended ideal imaging time is 24–48 h following RFA because the cellular damage caused by thermocoagulation in RFA is immediate.
Discussion
PET-CT has low sensitivity for the detection of HCC partly due to the high levels of glucose-6-phosphatase in the liver which dephosphorylates FDG-6-PO4 allowing it to leave the cell. Unlike the liver, other tissue do not have glucose-6-phosphatase, and thus FDG-6-PO4 is trapped within the cell allowing radiotracer accumulation and visualization. High-grade HCCs are less well differentiated and thus have less glucose-6-phosphatase.
Every year, there are nearly half a million people diagnosed with HCC. HBV or HCV infections and probably nonalcoholic liver disease are risk factors for HCC. The most common sites of extrahepatic metastatic HCC are the lung, abdominal lymph nodes, and bone.
Case 5.2
History
A 75-year-old man with newly diagnosed gallbladder carcinoma . PET-CT was requested to evaluate for metastatic disease.
Findings
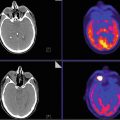
A 2.7 × 1.4 cm intensely active soft tissue lesion within the gallbladder (Fig. 5.2), with SUVmax of 5.7, represents the primary neoplasm. In addition, there is mild wall thickening of the gallbladder with pericholecystic fluid, with no definite discernible activity, probably due to inflammation.
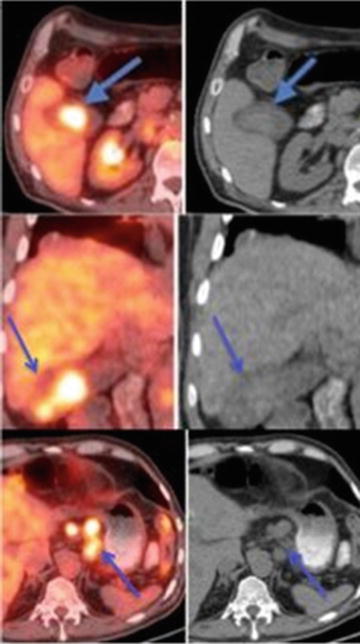
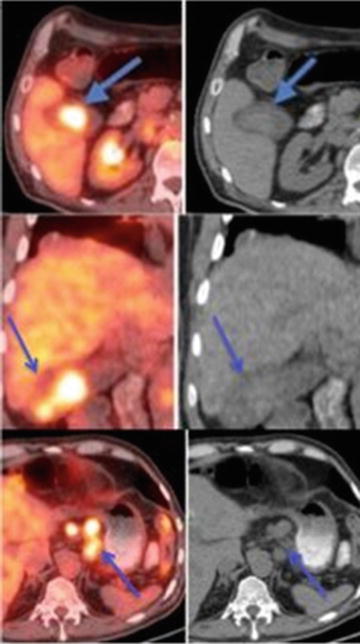
Fig. 5.2
Several celiac axis (Fig. 5.2), retroperitoneal, and retrocrural lymph nodes are seen, consistent with metastases. The largest celiac axis adenopathy (near the stomach) measures 1.6 × 1.7 cm and has a SUVmax of 5.6.
Pearls and Pitfalls
PET-CT is valuable for detecting regional lymph node involvement and distant metastases that are not diagnosed by multi-detector CT (MDCT).
PET-CT shows no significant advantage over MDCT for the diagnosis of the primary gallbladder tumor.
PET is helpful in detecting residual gallbladder carcinoma after cholecystectomy but has low sensitivity for detecting carcinomatosis.
Discussion
PET-CT shows a significantly higher positive predictive value (94.1 % vs. 77.5 %, p = 0.04) than that found for MDCT in the diagnosis of regional lymph node metastasis. In addition, PET-CT also demonstrates a significantly higher sensitivity (94.7 % vs. 63.2 %, p = 0.02) than MDCT in the diagnosis of distant metastases. A SUVmax of 3.65 was found to be the best cutoff value for detecting a gallbladder malignant tumor. PET-CT findings resulted in a change of management in 17 % of patients deemed resectable after standard workup.
Case 5.3
History
A 67-year-old man underwent an ERCP with biopsy revealing cholangiocarcinoma . PET-CT requested for staging.
Findings
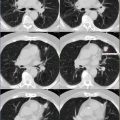
There is an ill-defined, intensely hypermetabolic large mass involving the medial segment of the left lobe and the anterior segment of the right lobe of the liver (Fig. 5.3, arrowheads), consistent with the known cholangiocarcinoma (CC). The tumor likely involves and engulfs the gallbladder due to the apparent indistinctness of the gallbladder wall. A small, active hepatoduodenal lymph node is present (not shown). In addition, there is also mild hypermetabolism involving the entire pancreas (Fig. 5.3, arrows) due to post-ERCP pancreatitis. Hypermetabolism surrounding the biliary stent is due to foreign body reaction, but in this case, there may also be tumor involvement.
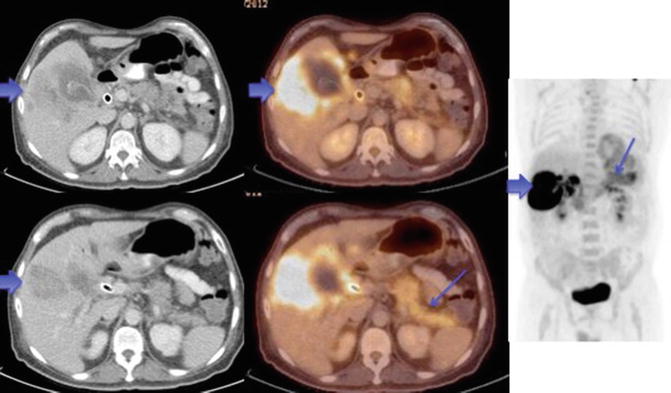
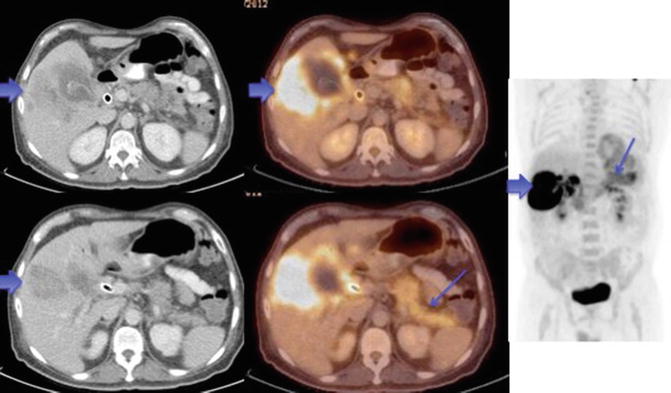
Fig. 5.3
Pearls and Pitfalls
PET-CT is valuable for detecting regional lymph node involvement and unsuspected distant metastases that are not diagnosed by MDCT.
Hypermetabolism could be seen in patients with primary sclerosing cholangitis or known granulomatous disease as well as biliary stents, which could mimic neoplasm.
Discussion
For cholangiocarcinoma, PET-CT shows significantly higher accuracy over CT in the diagnosis of regional lymph nodes (75.9 % vs. 60.9 %, p = 0.004) and distant metastases (88.3 % vs. 78.7 %, p = 0.004). There is no significant advantage of PET-CT over multi-detector CT (MDCT) for the diagnosis of a primary biliary tumor. FDG PET was shown to change management in 30 % of patients with CC. Additionally, FDG PET-CT is useful in patients with CC (except for infiltrating type) for detection of recurrent disease and for assessment of treatment response.
Case 5.4
History
A 73-year-old woman with recently discovered pancreatic head mass .
Findings
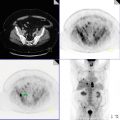
There is a 7 × 7 × 4 cm hypermetabolic pancreatic head mass with a SUVmax of 13 (Fig. 5.4).
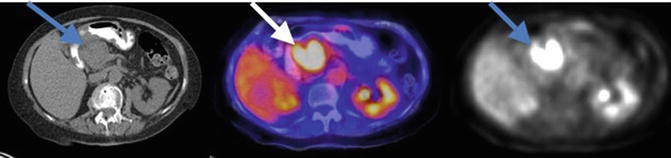
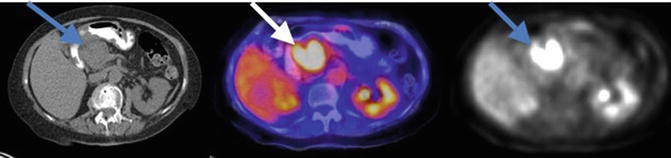
Fig. 5.4
Pearls and Pitfalls
For accurate staging of pancreatic carcinoma, the size of the tumor, relationship to adjacent vessels, and invasion of nearby tissue and spread of disease outside the pancreas must be assessed. Endoscopic ultrasound (EUS) has been found to be more accurate than CT in local staging of pancreatic malignancies and in predicting vascular invasion and resectability.
Pancreatic cancer spreads to regional lymph nodes followed by the liver and lung. Osseous metastases are rare.
PET can reliably detect hepatic, peritoneal, and other distant metastases that are at least 1 cm.
Discussion
The pancreatic head is defined as the segment to the right of the left border of the superior mesenteric vein (SMV) . The body extends from the left border of the SMV to the left border of the aorta. The narrow segment between the head and body is defined as the neck. The segment of pancreas posterior to the SMV is the uncinate process. PET-CT is helpful in differentiating benign and malignant pancreatic masses using a SUVmax cutoff of 2.5.
Case 5.5
History
Patient had a Whipple procedure for moderately differentiated pancreatic adenocarcinoma . PET-CT performed to assess response following chemotherapy.
Findings
There is peripheral increased FDG uptake at the liver surface (Fig. 5.5) with SUVmax up to 5.3 consistent with peritoneal carcinomatosis. Some of the foci of hypermetabolism demonstrate no CT correlate and some show peritoneal thickening or nodularity.
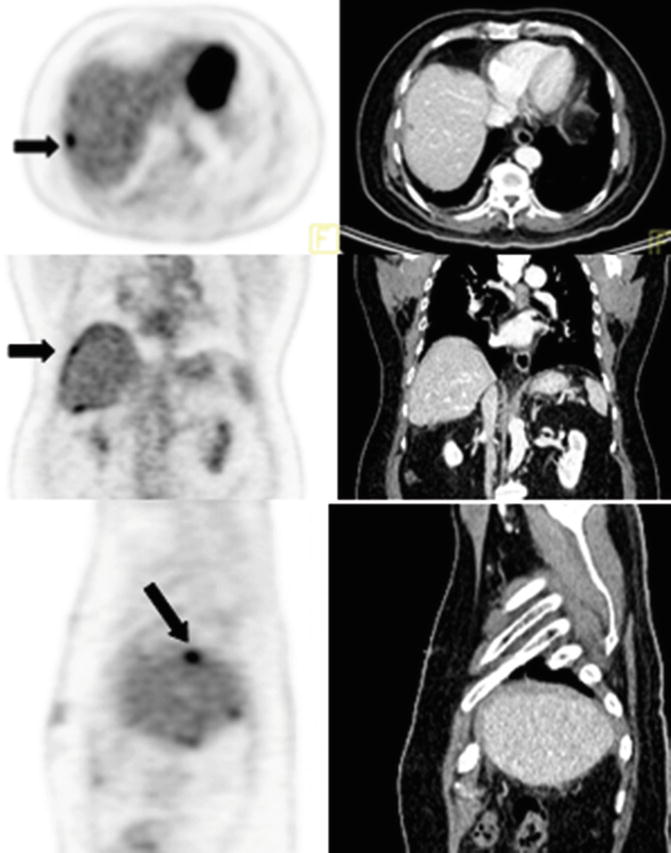
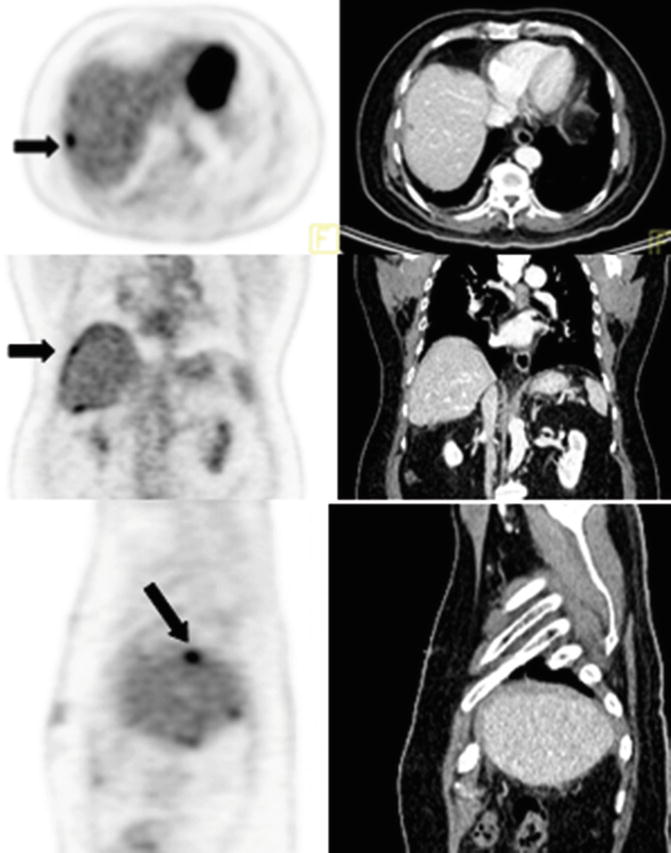
Fig. 5.5
Pearls and Pitfalls
Peritoneal metastases can appear to lie within the liver. Careful evaluation of the coronal and sagittal images is helpful in differentiating peritoneal implants from peripheral hepatic lesions particularly if the peritoneal deposits are not evident on CT.
Discussion
Tumors that may involve the peritoneal cavity include malignant peritoneal mesothelioma, pseudomyxoma peritonei, and metastases from the stomach, colon, appendix, gallbladder, pancreas, ovary, breast, lung, uterus, and lymphoma. CT has a sensitivity of 43 % and positive predictive value of 100 % for evaluation of peritoneal carcinomatosis, while PET-CT has a sensitivity of 78 % and positive predictive value of 96 %.
Case 5.6
History
Patient with moderately differentiated adenocarcinoma of the ampulla who is status post hepaticojejunostomy, right hemicolectomy, and partial hepatectomy in February 2010 had his last chemotherapy dose 2 months ago.
Findings
Patient had interval progression of right paratracheal and precarinal adenopathy and interval development of multiple right axillary and subpectoral nodes.
Pearls and Pitfalls
The histological differentiation of periampullary cancer is more important than the anatomical location. Pancreatobiliary histology carries a worse prognosis than intestinal histology in periampullary cancers.
Discussion
Periampullary cancers can arise from the pancreas, duodenum, distal common bile duct (CBD), or the ampullary duct. Ampullary carcinoma most commonly presents as obstructive jaundice in 80 % of patients and is treated with a Whipple procedure (pancreaticoduodenectomy). Pneumonia, abdominal infection, anastomotic leaks, and delayed gastric emptying are the most common complications following a Whipple procedure.