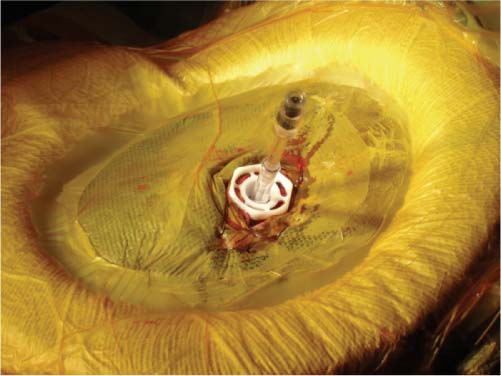
8 Brain biopsy allows neurosurgeons to access areas of the brain safely and accurately to determine the nature of an ongoing intracranial process. With the introduction of stereotaxis, the surgeon could now translate a three-dimensional (3D) database into the coordinate system of a rigid head frame and direct a biopsy needle to an area of interest during which the biopsy needle could be stabilized to prevent inadvertent displacement. Initially, biopsies were performed using computed tomography (CT) guidance; however, this imaging modality was rapidly replaced by magnetic resonance imaging (MRI) because of its ability to demonstrate the brain in multiple projections and its exquisite soft tissue discrimination and anatomic detail. Neuronavigational systems became popular in the 1990s and replaced frame-based stereotaxis for the performance of neurobiopsy. All of the above-mentioned biopsy techniques require the acquisition of preoperative images either several days or immediately before the surgical procedure is planned when the cranium is closed. Once the surgical procedure begins, the penetration of the skull and the incising of the dura will result in the subsequent loss of cerebrospinal fluid (CSF). This egress of CSF is unavoidable, but can lead to the displacement of the target tissue due to the shifting of the brain. Brain shift is one of the leading reasons for non-diagnostic brain biopsies. The degree to which the target tissue has moved cannot be easily determined during surgery and can necessitate that the tissue be examined by frozen section analysis by a pathologist to determine whether the procedure will lead to an accurate diagnosis of the underlying central nervous system (CNS) disorder. The only current surgical technique that will allow the neurosurgeon to compensate for the displacement of the brain that occurs during surgery is intraoperative MRI-(iMRI-) guided brain biopsy.1–5 During this procedure, the imaging is acquired in near-real time so that the advancement of the biopsy needle through the brain can be monitored by the surgeon until the target has been encountered. iMRI-guidance was used more than a decade ago to perform a brain biopsy with the first procedures using a 0.5 tesla (T) interventional MRI system.6,7 In 1997, we performed the first successful 1.5 T high-field brain biopsy using a closed short-bore iMRI system (Philips Healthcare, Andover, MA). In performing the first high-field brain biopsies there was no way to direct the biopsy needle toward the target or to stabilize the needle once the target had been reached. For these reasons, the biopsies were performed under general anesthesia to avoid the potential for displacement of the needle during the procedure. The ability to direct and stabilize the biopsy needle was achieved in 1999 when we combined the use of a disposable skull-mounted trajectory guide with the 1.5 T short-bore iMRI system.2,8 Lesions located in the supratentorial compartment and the posterior fossa can be safely sampled using iMRI-guidance and this trajectory guide. Even brainstem lesions can be accessed using iMRI-guidance because a needle trajectory that begins with a coronal entry point can be chosen that avoids the ventricular system. All patients receive intravenous (IV) antibiotics (cefazolin 1 g IV) and corticosteroids (dexamethasone 10 mg IV) before beginning the procedure. The neurosurgeon has previously reviewed all of the patient’s MRI studies to determine which imaging sequences will best demonstrate the lesion that is to be biopsied and in which scan orientations it will be best to image the biopsy needle as it passes through the brain. Low-grade brain tumors and demyelinating disease are best demonstrated on T2-weighted (T2W) orthogonal half-Fourier acquisition single-shot turbo spin-echo (HASTE) or turbo fluid-attenuated inversion-recovery (FLAIR) images. Secondary metastatic brain tumors or primary high-grade glial tumors are associated with blood-brain barrier breakdown and are best visualized on T1-weighted (T1W) images after the administration of gadolinium. Administration of the contrast agent is usually reserved until the time when the trajectory guide is being used for targeting to prevent the diffusion of the contrast material out into areas where the blood-brain barrier has broken down, which may not represent the true focus of confluent tumor tissue. Superficial and cerebellar lesions are usually imaged in the coronal and axial planes because the needle is generally passed the shortest distance from the surface of the brain to the target. Brain-stem and deep central supratentorial lesions are usually reached by passing the biopsy needle through the frontal lobe while the imaging is obtained in the coronal and sagittal planes. Brain biopsies can be performed under local or general anesthesia. We prefer to perform our MRI-guided brain biopsies under general anesthesia for several reasons. Because of the length of time that is required to perform an MRI-guided brain biopsy due to the necessity to obtain intraoperative imaging, it can be difficult for patients to remain calm and immobile for the entire procedure. The biopsy procedure can last from 1 to 3 hours depending on the complexity of the surgery. Many lesions are located in areas in the brain where it is difficult for a patient to maintain the head in the proper orientation for prolonged periods. If the procedure was performed under local anesthesia and the patient received IV sedation, it is possible that the patient may startle with the initiation of the scanning because of the loud noise that is associated with some of the MRI sequences. Abruptly displacing the head with the biopsy needle within the brain could lead to neurologic injury – or worse – because the head must be located at the center of the magnet during imaging, which is at least an arm’s length away from the flared openings of the MRI scanner. Once under general anesthesia the patient is brought from the main operating room to the iMRI suite where transfer is made from the transport cart to the padded MRI-compatible surgical table. The vast majority of brain biopsies are performed with the patient in the supine position. Even occipital and cerebellar biopsies can be performed in a supine patient by turning the head to the side and taping the ipsi-lateral forehead down onto the side of the surgical table to prevent inadvertent posterior rotation of the head. A shoulder roll is placed if the head is to be turned. If the lesion is in the posterior fossa, then the head is placed on folded towels instead of on a foam rubber donut because the edge of the donut can interfere with the passage of the biopsy needle; the donut will compress due to the weight of the patient’s head. One of the circular radiofrequency (RF) coils is placed underneath the head on either the towels or the donut in a plastic bag to prevent soiling of the coil (Fig. 8.1). The second coil is then wrapped in gauze and sandwiched between two sterile plastic sheets. The plastic in the center of the coil is then excised before the coil is stapled to the sterile drapes surrounding the surgical field. After the second RF coil is stapled to the surgical drapes in a location that is opposite to the first coil, an Ioban drape (3M Medical Products, Minneapolis, MN) is placed over the entire surgical field to establish and maintain a sterile environment. Positioning the RF coils in this way will allow the entire biopsy to be performed through one coil, which will enhance visualization of the target site during the biopsy by improving the signal-to-noise ratio and affording the high resolution imaging. To date, we have not needed to place any patient in the prone position to perform a cerebellar biopsy. Fig. 8.1 Brain biopsy is performed through one of the radiofrequency surface coils with the second coil placed under the head of the patient in a phased array. The alignment stem has been placed in the guide tube for alignment and the white plastic locking nut is used to secure the guide tube in place after an accurate trajectory to the target has been achieved. (Courtesy of Walter A. Hall and Charles L. Truwit.) The disposable Navigus trajectory guide8 that we use for brain biopsies is commercially available and manufactured by Medtronic Navigation, Inc., Louisville, CO (Fig. 8.2). The guide has two bases that can be attached to the skull either in a burr hole or to allow for a twist drill craniostomy. We prefer the base that rests in a burr hole because it allows for the visualization of the cortical surface and any blood vessels that may lie underneath the dura mater once it has been incised. In penetrating the skull with a twist drill it is possible to injure a superficial cortical vessel resulting in a subarachnoid hemorrhage. There is also another version of the trajectory guide base that is angled allowing for a more oblique angle to be attained thereby allowing for the sampling of inferior anterior frontal lesions where the skin incision is placed behind the hairline (Fig. 8.3).
High-Field Brain Biopsy
Preoperative Preparation
Anesthesia
Positioning
Procedure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree