Fig. 1 a–f.
Femoral head avascular necrosis in six different patients studied with magnetic resonance imaging. a Coronal T1-weighted image shows the typical „band-like” sign (arrows). b Axial T2-weighted image shows the „double-line” sign (arrows). c Axial T2-weighted image shows the subchondral fracture („crescent” sign), in keeping with advanced disease (arrow). d Coronal STIR image in a 50-year-old woman, with known asymptomatic bilateral osteonecrosis and recent pain in the right hip, shows the subchondral fracture (thin arrow), bone marrow edema (thick arrow) and joint effusion. The osteonecrotic lesion on the left side (open arrow) is not associated with bone marrow edema. e On coronal T2-weighted image, the lesion (arrow) is well contained within the acetabulum. f Coronal T1-weighted image in a 45-year-old man shows a noncontained lesion of the noncollapsed right femoral head, extending slightly outside the lip of the acetabulum. The left hip shows a noncontained lesion
The lesion size and extent of femoral head involvement are important parameters in predicting outcome and determining treatment in FHAVN [8]. The size of lesions on plain radiographs may be difficult to assess and might not correlate with the size on MR imaging. The lesion location is also an important parameter in predicting femoral head collapse. It has been shown that a hip with an intact articular surface, combined with a well contained from the acetabulum necrotic lesion, has the best functional outcome following joint preserving surgery (Fig. 1 e,f) [8]. The presence of BME in patients with known FHAVN seems to correlate with pain and progression of the disease in terms of articular collapse. Following surgery with free vascularized fibular grafting, persistent or increased marrow edema and low SI within the upper part of the graft suggest failure [9].
Transient Osteoporosis/Regional Migration Osteoporosis
Transient osteoporosis of the hip (TOH), or transient BME syndrome, usually involves healthy middle-aged men; it rarely affects women, almost exclusively during the third trimester of pregnancy or the immediate postpartum period [10]. The syndrome is characterized by acute disabling pain in the hip and functional disability without a history of previous trauma. It has been considered by many authors as an initial and reversible form of FHAVN or alternatively as a variety of algodystrophy syndromes. Currently, it is believed to represent a distinct clinical entity without any sequelae following conservative treatment. With few exceptions, in patients with TOH, the clinical course is relatively short and may last up to 6–8 months, with rapid aggravation of pain and functional restriction of the hip during the first month after the onset [10, 11]. Osteopenia of the proximal femur may be present on plain radiographs at 3–6 weeks after the onset of the symptoms. Spontaneous clinical and radiological recovery is the rule. A characteristic BME signal on T1-weighted and fat-suppressed PD or STIR MR images has been demonstrated in patients with TOH (Fig. 2a–c) [11]. Sparing of the subchondral bone marrow, particularly on the medial aspect of the femoral head, is a well-recognized finding in TOH [11]. Joint effusion and mild synovitis, combined with periarticular soft tissue edema, are constant findings. The BME area is enhancing following contrast administration. In about 5% of patients, linear subchondral changes may appear and probably represent reversible microtrabecurar fractures.
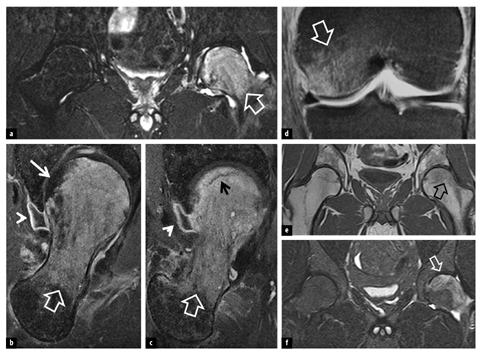
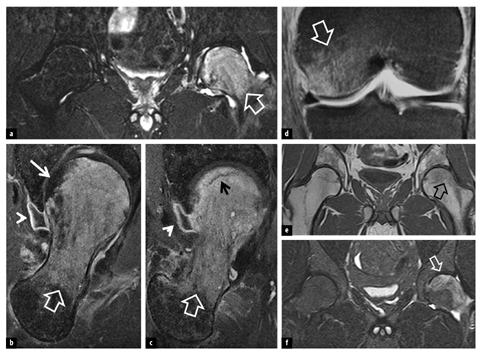
Fig. 2
A 40-year-old man with 2-month left hip pain and complete resolution of pain 8 months after onset of symptoms. a Coronal STIR magnetic resonance (MR) image shows the high signal intensity bone marrow edema-like area (arrow). b, c Oblique axial contrast-enhanced fat-suppressed T1-weighted MR images show homogeneous enhancement of the edematous marrow lesion (open arrows), sparing of subchondral area medially (thin arrow), a microtrabecular subchondral fracture (black arrow) and mild synovitis (arrowheads). A 35- year-old man with regional migrating osteoporosis. d Originally, the bone marrow edema lesion was located in the medial femoral condyle, as shown in the coronal fat-suppressed proton density weighted MR image (arrow). Coronal T1-weighted (e–) and STIR (f) MR images 18 months after d show bone marrow edema-like lesion in the left femoral head, in keeping with recent hip joint pain (arrows). The DEXA of the spine 16 months after the onset of symptoms showed marked osteoporosis (Z-score, -3.3)
Regional migratory osteoporosis (RMO) is defined as sequential polyarticular arthralgia of the weight-bearing joints, limited to the lower appendicular skeleton [12, 13]. The pattern of shifting symptoms is typically proximal to distal, with a mean migration interval of 4– 9 months. In patients with TOH, migration occurs in 5% to 41% [11]. Usually, the joint nearest the diseased one is the next to be involved, i.e., contralateral hip, or either ipsilateral knee or ankle. Rarely, the disorder migrates from the peripheral joints to the more proximal ones (Fig. 2d-f). As the MR imaging findings are identical to those of TOH, with a similar duration of symptoms, the diagnosis of RMO mainly depends on its clinical behavior [12, 13]. There are reports suggesting that systemic osteopenia or osteoporosis may coexist with RMO. Densitometric evaluation, preferably by means of spinal DEXA, may significantly contribute to treatment planning.
Stress Injuries
Osseous stress injuries represent a spectrum of disorders ranging from a stress reaction to a frank fracture. Stress fractures are classified as fatigue (abnormal forces applied on normal bone) and insufficiency (normal forces applied on weakened bone) [13]. The former are overuse injuries primarily afflicting competitive and recreational athletes and military recruits, and they account for more than 10% of all sports-related injuries. The latter occur in the elderly, mainly postmenopausal osteoporotic women, and are located most commonly in the pelvic girdle followed by the proximal femur and the spine. A combined fatigue and insufficiency fracture may occur in (a) young female anorexic gymnasts or long distance runners, and (b) osteoporotic middle-aged avid runners.
Early diagnosis and intervention are essential for prompt and effective rehabilitation, often preventing progression to a complete fracture. MR imaging has become the modality of choice in the evaluation of patients with a high index of suspicion for a stress injury. The application of fluid-sensitive sequences is mandatory for early diagnosis. In addition, MR imaging allows accurate grading of these injuries and provides useful information regarding prognosis and clinical management as it is able to detect different causes of associated symptoms. Sites of stress injuries with pain referred to the hip include the inferomedial femoral neck, superior and inferior pubic rami, acetabular roof, subcortical femoral head and very rarely the sacrum.
Stress response or stress reaction is a pre-fracture condition characterized by low signal on T1-weighted and high signal on T2-weighted and STIR sequences, and is caused by repetitive trauma to the bone marrow, without any fracture line (Fig. 3a) [14, 15]. Stress reactions are distinguished from (a) fatigue fractures, by the absence of a distinct fracture line, and (b) bone contusion only with history, by means of one single traumatic effect occurring in the latter. Bone bruise is rare in the hip, both in the growing skeleton and in adults.
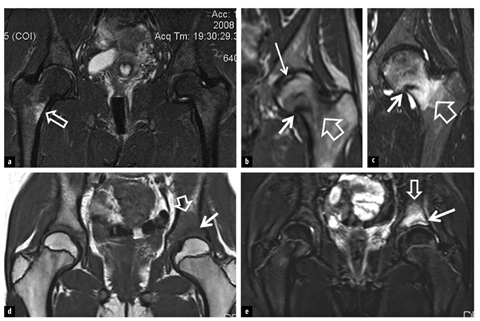
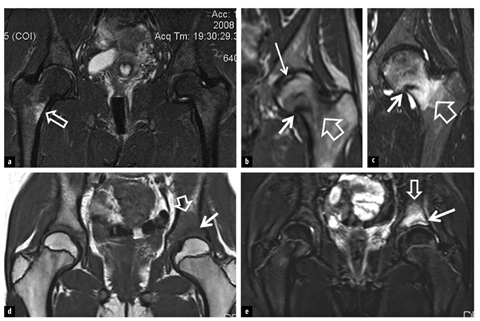
Fig. 3 a–e
a A 30-year-old obese woman who started playing tennis in an attempt to lose weight is referred with right hip pain after practicing for 6 weeks. The coronal STIR magnetic resonance (MR) image shows bone marrow edema in the medial femoral metaphysis in keeping with stress reaction (arrow). b, c A 22-year-old long-distance female runner presents with pain in the left hip joint. The coronal T1-weighted (b) and STIR (c) MR images show a fatigue fracture (thick arrows) surrounded by bone marrow edema (open arrows) and an old subchondral fatigue fracture (b) with no associated bone marrow edema (thin arrow). Coronal T1 (d) and STIR (e) MR images of a 9-year-old female elite dancer show a fatigue fracture in the acetabulum (arrows) surrounded by bone marrow edema (open arrows)
Fatigue fractures are shown as low SI linear structures on all pulse sequences, extending up to the cortex. The fractures are surrounded by hypointense areas on T1- weighted images and hyperintense areas on fat-supressed PD/T2-weighted or STIR images because of the BME and hemorrhage (Fig. 3b-e) [14, 15]. MR imaging has been shown to be 100% accurate in differentiating stress fractures from other causes of sports-related disorders in the hip. MR imaging can be quite useful for the follow- up of elite athletes because, by using fat-suppressed sequences, it allows the depiction of return of the bone marrow signal to normal in about 3 months. The majority of stress fractures have a good prognosis and are healed in a few weeks with conservative treatment. Surgical operation is required for displacement of a stress fracture, usually in cases of delayed diagnosis or when it develops on the outer aspect of the femoral neck, where tensile forces predominate and it might become unstable. Insufficiency fractures exhibit imaging findings that are identical to those of fatigue fractures.
Femoroacetabular Impingement and Osteoarthritis
Femoroacetabular impingement (FAI) is caused by a conflict between the acetabulum and the femur [16]. This may be due to an abnormal shape of the femur, overcoverage of the acetabulum or supraphysiologic range of motion [17]. Extra-articular factors, such as abnormal torsional alignment of the femur, can also cause FAI. Commonly, several of these factors are combined. FAI results in premature osteoarthritis of the hip.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







