Fig. 10.1
Hip arthroplasty
At present, there is a wide range of prostheses with different new types of articulations such as metal on metal and ceramic on ceramic instead of metal on polyethylene, based on new scientific research and availability of improved metal alloys, which may reduce the wear up to 1/4,000.
The use of exchangeable neck/ball (modular prosthesis) in primary as well as revision surgery has enhanced the surgeons amatory to create a stable prosthesis in most conditions and facilitates future revision surgery.
In some designs, the stem and ball are one piece; other designs are modular, allowing for additional customization in fit.
The stem could be implanted with cemented or uncemented technique.
Over the past 40 years, there have been many improvements in the materials and the methods used to hold the femoral in place. Today, the most common used bone cement is an acrylic polymer called polymethylmethacrylate.
From 1980s, new implant designs were introduced to attach directly to bone without the use of cement. In general, these designs are larger and longer than those used with cement.
From the results of Implants National Registries, it seems to be that the uncemented technique is more indicated for younger patients. However, final decision regarding implant selection should be based on the quality and anatomy of the patient’s bone as well as on expected functional demands and expected life span of the patient.
All these issues have an impact on the choice of component fixation and, above all, on the choice of bearing surfaces.
The patient’s bone type/quality, the presence of bone loss on the acetabular or the femoral side as well as the presence of shortening or deformity are all factors that may influence the final decision to opt for cemented or cementless fixation and to determine whether additional augmentation or bone grafting will be required. Several rating systems for bone quality have been reported. The Dorr classification (Fig. 10.2) has the advantage of simplicity and reproducibility and is of practical value in the clinical setting. According to this system, cemented femoral components are often advocated for Type C bone. Severe osteoporosis is associated with increased risk of intraoperative fracture, both femoral and acetabular, necessitating great care in the preparation and insertion of the components. In this setting, the bone quality may be such that the use of cemented component(s) may be preferable to achieve a stable and durable construct.
Fig. 10.2
Dorrr femoral bone classification. Type A narrow canal with thick cortical walls (champagne flute canal). Type B moderate cortical walls. Type C wide canal with thin cortical walls (stove-pipe canal)
In the instance of THA after previous proximal femoral fracture or osteotomy where the hardware has been removed, the most distal screw hole should ideally be bypassed by at least two and a half times the diameter of the bone at that level to reduce the risk of periprosthetic fracture. This may then require that a revision-type long-stem femoral component be used in the primary setting.
Developmental dysplasia of the hip poses additional technical challenges. This is particularly seen in Crowe Types III and IV hips in which augmented acetabular reconstruction using metal and/or structural bone graft may be required. In addition, distortion of the femoral anatomy may require the use of either a fully modular femoral component to allow for correction of excessive femoral neck anteversion or even potentially a custom femoral component.
The tribology of materials is the main role in the follow-up of long-term implants. In recent years, technology has led to strong developments in this surgery developing more resistant materials and then determining a lower failure rate.
Nowadays, the aseptic loosening, normally due to the implants’ wear, represents more than 75 % of the failures in prosthetic surgery of the hip.
The coupling materials available are as follows:
10.2 Metal on Metal
These are fabricated from a harder cobalt–chromium alloy and thus consist of a metal-on-metal couple. This new combination creates a differential hardness between the two moving parts. This differential hardness determines that the metal is likely to release less particles into the body and wear less over time. In all hip prostheses, the femoral head wears quicker than the acetabular shell (except the metal-on-polyethylene ones (hard-on-soft)). The difference in hardness is a major advantage over the previous metal-on-metal prostheses and even more over the metal-on-polyethylene prostheses.
The metal-on-metal bearings are hard without being brittle and they are more resistant to scratching and wearing. There is a debate on the effect of metal ions released by the couple; the potential effect of these ions is not clear yet, but research is being done on that subject.
10.3 Ceramic on Ceramic
Ceramic-on-ceramic (COC) has been an excellent alternative bearing surface for total hip arthroplasties (THA) in young, high-demand patients with end-stage arthritis of the hip.
Ceramic material has been used for THA in Europe for 40 years with variable results.
Hamadouche et al. described minimal wear, a low rate of complications and limited osteolysis with COC THA after 18.5 years of follow-up. On the other hand, the revision rate in Europe and the USA from 1988 till 1996 varied between 3 and 44 %.
Subsequently, new generations of C–o–C BIOLOX-delta bearings were developed, eliminating this risk and presenting the superior tribological properties of ceramics.
As it is demonstrated, the reinforcing mechanism is fully activated within a region of a few micrometers. For the macroscopic performance of the material, it is very important that immediately at the beginning of crack initiation, the reinforcing mechanisms are also activated. Regarding this mechanism, one should keep in mind that the average distance between the reinforcing zirconia particles is approx. 0.3 mm, i.e., similar to the grain size. Thus, the reinforcement is activated immediately when any microcrack is initiated. This is of particular interest for the significant advantage of ZTA (BIOLOX®delta) under severe wear conditions.
10.4 Ceramic–Metal on Polyethylene
Polyethylene acetabular cups coupled with metal or ceramic femoral heads remain the most popular bearing combination in the hip. In the long term, the polyethylene cups wear and the micron and submicron wear particles result in osteolysis and loosening. Particles accumulate in peri-prosthetic tissues until a critical volume and concentration is reached, which results in osteolysis. Patients have different levels of reactivity to polyethylene particles and particle concentrations in tissues are dependent on access. It is important to reduce polyethylene wear rate in order to extend the osteolysis-free lifetime.
10.5 Hip Resurfacing
Increasing number of total hip replacements in young patients in recent years is accompanied by an increased number of revision operations due to excessive wear of the polyethylene in the young active patient, leading to osteolysis and loosening of the prosthesis. For this reason, there has been extensive research to find alternative bearings with better wear properties to cope with this tremendous devastating problem.
In conventional hip replacement surgery, the femoral head and a portion of the femoral neck are completely removed and replaced with a stemmed prosthesis, which is inserted into the medullary canal of the upper femur.
Hip resurfacing procedure shapes the femoral head and recaps it with a metal surface replacement. This preserved the normal bone of the upper femur and allows normal mechanics and weight-bearing loads across this area. Normal load forces through the bone of the upper femur keep the bone healthy and strong. The acetabulum of the hip joint is also resurfaced.
Surface hip arthroplasty (Fig. 10.3) has become more important in treating younger patients for osteoarthritis in the new century.
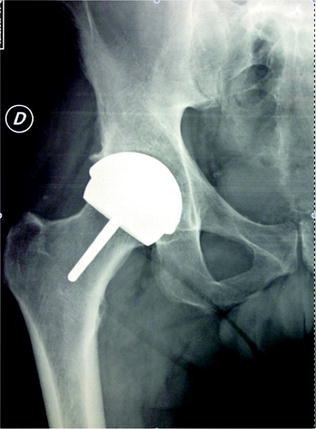
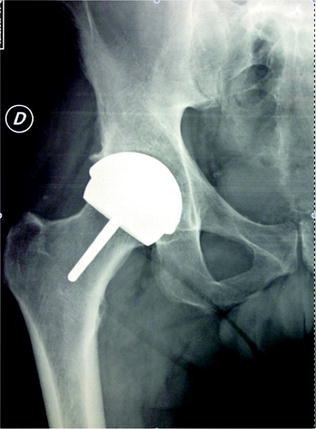
Fig. 10.3
Hip resurfacing
The resurfacing technique in the past, namely the Teflon prosthesis of Charnley and metal-on-polyethylene prosthesis of Wagner or Tharies prosthesis, is based on failure of the design and material properties of the implants, rather than failure of the resurfacing concept.
Due to a perfect operation technique, an up-to-date knowledge and fabrication of metal-on-metal articulations, the resurfacing technique is doing extremely well with clinical and radiological follow-up for more than 10 years.
The overall results were consistent with data produced from registry and high specialization centers in that the clinical outcome of large male patients was extremely encouraging, whereas the survival of the smaller joints was less satisfactory.
10.6 Hip Revision
Hip revision surgery, which is also known as revision total hip arthroplasty, is a procedure in which the surgeon removes a previously implanted artificial hip joint, or prosthesis, and replaces it with a new prosthesis. Hip revision surgery may also involve the use of bone grafts. The bone graft may be an autograft, which means that the bone is taken from another site in the patient’s own body, or an allograft, which means that the bone tissue comes from another donor (Fig. 10.4).


Fig. 10.4
Hip revision arthroplasty
Hip revision surgery has three major purposes: relieving pain in the affected hip, restoring the patient’s mobility, and removing a loose or damaged prosthesis before irreversible harm is done to the joint. Hip prostheses that contain parts made of polyethylene typically become loose because wear and tear on the prosthesis gradually produces tiny particles from the plastic that irritate the soft tissue around the prosthesis. The inflamed tissue begins to dissolve the underlying bone in a process known as osteolysis. Eventually, the soft tissue expands around the prosthesis to the point at which the prosthesis loses contact with the bone.
In general, a surgeon will consider revision surgery for pain relief only when more conservative measures, such as medication and changes in the patient’s lifestyle, have not helped. In some cases, revision surgery is performed when X-ray studies show loosening of the prosthesis, wearing of the surfaces of the hip joint, or loss of bone tissue even though the patient may not have experienced any discomfort. In most cases, however, increasing pain in the affected hip is one of the first indications that revision surgery is necessary.
Other less common reasons for hip revision surgery include fracture of the hip, the presence of infection, or dislocation of the prosthesis. In these cases, the prosthesis must be removed in order to prevent long-term damage.