Author(s)
Country
Year of publication
No. of cases
Site of involvement
Radiological study
Outcome
Arseni and Samitca
Romania
1
Skull
X-ray
NS
Orman and Roux
South Africa
2
Vault—frontal (1) and base (1)
X-ray and angiogram
NS
Kanaka et al.
India
1
Vault
X-ray
Behavior improved, recurrence after 6 mos
Teymoorian and Bagheri
Iran
4
Base
X-ray
Complete recovery (2), died at 4 mos (1), well up to 2 yrs (1)
Gokalp et al.
Turkey
1
Vault—Lt temporoparietal
X-ray
Complete recovery at postop 3 mos
Ozgen et al.
Turkey
1
Intrasellar
X-ray and CT
Complete recovery at postop 10 mos
Kanpolat et al.
Turkey
1
Base—cavernous sinus
CT
Unchanged ocular movement restriction at postop 12 mos
Gedikoglu et al.
Turkey
1
Parasellar
CT
Complete recovery at postop 3 mos
Benmoussa et al.
Morocco
2
Vault—parietal (1), occipital (1)
CT
Good (1), recurrence (1)
Aydin et al.
Turkey
1
Vault—intradiploic, parietal, and occipital
X-ray, CT
Died at early postop
Rivierez et al.
France
1
Base—cavernous sinus
CT, MRI
NS
el Khamlichi
Morocco
1
Base—cavernous sinus
X-ray and CT
NS
Pasaoglu et al.
Turkey
1
Base—infratemporal fossa
CT
Complete removal, No follow-up
Ennouri et al.
Tunisia
1
Vault—Lt temporal
CT and MRI
Well at early postop
Abbassioun and Amirjamshidi
Iran
7
Vault and base
X-ray, CT, and MRI
Well
Erman et al.
Turkey
1
Vault—Rt parietal
CT
Complete recovery
Turguta
Turkey
3
Base
X-ray and CT
Complete recovery (2), unchanged (1)
el-Kohen et al.
Morocco
1
Base—Lt jugular foramen
CT and MRI
Chemotherapy followed by motor improvement
Taghipour et al.
Iran
1
Base—foramen magnum
MRI
Complete recovery
Lath et al.
India
1
Base
CT
Well
Limaiem et al.
Tunisia
1
Vault—Rt frontal
CT
Recurrence requiring second operation
Raynham et al.
South Africa
3
Base
CT
Complete recovery
Hossain et al.
Bangladesh
1
Vault—Rt temporal
CT
Complete recovery
Sureka et al.
India
1
Base—posterior fossa
CT and MRI
Well at early postop
Yazdani et al.
Iran
1
Base and orbit
CT
Recurrence
Siddiqui et al.
India
1
Vault and orbit
CT
Complete recovery
Young males are most commonly affected (Teymoorian and Bagheri 1976). Because of the restricted geographic distribution of the echinococcal worms, persons of certain races are affected more commonly than others; however, the parasite has the capability of infecting persons of all races equally. No sexual predilection is recognized (Dandan 2008).
Pathology
Cranial hydatid cyst may occur in the skull bones (intraosseous) and in the intracranial space. In the skull, it may involve the cranial vault and skull base and may spread to the paranasal sinuses and orbit. Primary hydatid disease of bone due to E. granulosus occurs when a blood-borne scolex settles in the bone (Limaiem et al. 2009). It initially invades the diploe, and as it grows it widens the diploic space, and subsequently it extends in both directions (Dharkar 1996). The wall of the cyst consists of an inner endocyst (germinal layer) and outer ectocyst (laminated layer) (Nemati et al. 2010). In bone involvement, pericyst formation does not occur, thereby allowing aggressive proliferation in an irregular branching fashion along the line of least resistance, especially the bone canals. The parasite replaces the osseous tissue between trabeculae due to the slow growth of multiple vesicles. With time, the parasite reaches and destroys the cortex, with subsequent spread of the disease to surrounding tissues (Limaiem et al. 2009). Early cases present as an expansile osteolytic lesion in the diploe. The more advanced forms manifest as multilocular or unilocular destructive lesions with adjacent soft tissue masses (Teymoorian and Bagheri 1976). As the cyst grows, the bone undergoes pressure atrophy, and the inner or outer table of the skull ruptures. The inner table of the skull frequently ruptures, and the vesicular larva passes into the epidural space inducing symptoms of increased intracranial pressure. Less frequently, cysts may rupture the outer table of the skull at many spots and involve the scalp to produce prominence on the head (Aydin et al. 1992; Limaiem et al. 2009). When both outer table and inner table are destroyed, intra-cranial and extra-cranial spaces become communicated with each other (Fig. 5.1).
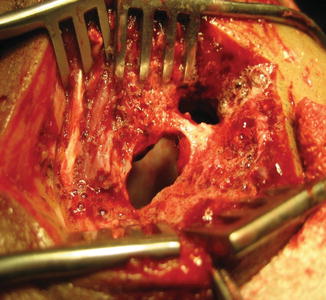
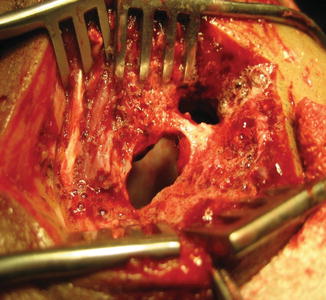
Fig. 5.1
Eroded bone seen perioperatively
Presentation
Cranial hydatid cysts present by their location in the skull. Nevertheless, if it ruptures, it may then show systemic features. Generally, four syndromes dominate the presenting clinical manifestations of cranial hydatid disease including increased intracranial pressure (48 %), skull deformity (48 %), cranial nerve palsies (42 %), and focal neurological disturbance (30 %) (Aydin et al. 1992; Limaiem et al. 2009).
When hydatid cyst involves the cranial vault, it may present with swelling on the head which causes the deformity of the head. It is usually painless and insidious in growth, but if it becomes infected, then it becomes painful. When frontal bone is involved, swelling is on the forehead and frontal region. When it involves the parietal bone, swelling will be on the parietal region. Accordingly, swelling may be on the temporal, occipital, or suboccipital region. The swelling is firm in consistency (Dharkar 1996). Scalp moves over the swelling if it is not ruptured externally. When it ruptures and involves the extra-calvarial soft tissues, swelling may be soft and cystic. If it becomes infected, all the features of acute inflammation may present in the form of swelling, redness, tenderness, and raised local temperature (Fig. 5.2).


Fig. 5.2
Infected hydatid cyst (abscess) showing all the features of acute inflammation
Cranial hydatidosis may present with the features of intracranial space-occupying lesion. Presenting features may be classified as (a) features of raised intracranial pressure and (b) focal neurological signs. Intracranial pressure may increase due to its volume or it may obstruct the cerebrospinal fluid (CSF) pathway. These patients may also present with seizure (Al-Akayleh 2003). Features of raised intracranial pressure are headache, nausea and vomiting, papilledema, blurring of vision, gait disturbance/ataxia, vertigo, diplopia, bradycardia, and hypertension. In advanced conditions, respiratory irregularity and deterioration of level of consciousness may occur (Greenberg 2001). Focal neurological signs are according to the location of the cyst in the cranial vault, like hemiparesis, hemisensory deficit, cognitive disorder, and visual deficit. Diagnosis of a hydatid cyst can sometimes be confused with other space-occupying lesions of the brain, especially abscesses, neoplasms, and arachnoid cysts (Anvari et al. 2009; Bahloul et al. 2009; Nemati et al. 2010). Hydatid cyst in the skull base usually remains silent unless it involves the adjacent structures. It may involve the cranial nerves and may present with the features of cranial nerve palsies. Patient may present with anosmia if the cyst involves the olfactory nerve in the anterior cranial fossa at the cribriform plate. It may involve the optic nerve, and orbit may present with visual impairment and proptosis (Fig. 5.3). Third, fourth, and sixth cranial nerves may be involved in the cavernous sinus or at their exit from the cranial cavity with diplopia and/or ophthalmoplegia. Hydatid cyst of the anterior cranial fossa enters into the paranasal air sinuses, which may precipitate development of sinusitis. Hydatid cyst of the middle cranial fossa may present with third, fourth, fifth, and sixth cranial nerve palsy. It may enter into the infratemporal fossa. Hydatid cyst of the posterior cranial fossa may present with features of (a) lower cranial nerve palsy like facial asymmetry, vertigo, impaired hearing, tinnitus and ringing in the ear, and regurgitation on swallowing; (b) long tract signs like weakness of one or both upper and lower limbs; and also (c) cerebellar signs like speech difficulty (dysarthria), gait disturbance, and ataxia. Raynham et al. (2009) reported three cases of skull base hydatid cyst, among them one involving the paranasal air sinus and presenting with complicated sinusitis; a second one involving the infratemporal fossa and presenting with painless right facial swelling, lateral displacement of ramus of the mandible, and sensory impairment of maxillary and mandibular division of the fifth cranial nerve; and a third one involving the left temporal bone and posterior cranial fossa and presenting with progressive weakness of legs, left arm, right face, and mixed sensorineural and conductive type of hearing loss.


Fig. 5.3
Infected hydatid cyst involving orbit developing proptosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree