Physiological reason
Clinical condition
Abnormally high CO2 production
Catabolic state
Hypoventilation
Unadjusted ventilator settings
Drugs
Respiratory muscle weakness
Reduced respiratory drive
Ventilation/perfusion mismatch
Lung collapse
Atelectasis
Pulmonary embolism
COPD
Alveolar/capillary barrier pathology
Interstitial pneumonia
ARDS
Pulmonary fibrosis
Barotrauma
Treating hypercarbic patients, with or without hypoxemia, whose lung compliance is diminished is challenging and relies heavily on imaging to achieve an accurate diagnosis and to monitor treatment.
Imaging Techniques
The portable chest X-ray is the initial screening tool and may identify lung parenchymal causes of hypercarbia but given the supine acquisition may not be a sensitive test. Since pulmonary embolism is on the differential diagnosis contrast enhanced CT is the gold standard imaging technique permitting comprehensive assessment of mediastinum, pleural space, lung parenchyma and pulmonary vasculature.
Central causes of reduced respiratory drive resulting in hypercarbia may be drug induced, which will often be clinically apparent. Neuropathy or myopathy is usually diagnosed on clinical grounds. Imaging using chest radiograph or CT may identify features of phrenic nerve injury and malignant or compressive causes.
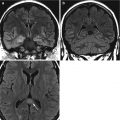
Following neurological evaluation brain imaging may be required to exclude a central cause for hypoventilation. While MRI is the reference standard for detecting brainstem disease, brain CT may be the initial test in view of access and safety. This does not preclude subsequent MRI if clinical suspicion is high.
Barotrauma
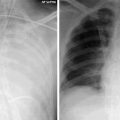
Barotrauma is a common complication of mechanical ventilation. There is evidence that it may occur in all mechanically ventilated patients but only presents as a clinical problem in approximately 10–20 %. Barotrauma is a consequence of alveolar distension in the context of prolonged ventilation with high airway pressures. Although most commonly occurring in patients with ARDS, barotrauma can become a problem in any mechanically ventilated patient (Fig. 21.1). Manifestations of barotrauma are mostly subtle. If patients become increasingly difficult to ventilate clinicians should look out for radiological signs such as subcutaneous emphysema, pneumopericardium, pneumomediastinum, and uncommonly pneumoperitoneum.


Fig. 21.1




A 55-year old female with respiratory failure on ECMO with difficult ventilation. Chest radiograph (left) shows widespread bilateral alveolar opacification with a subtle right pneumothorax (thin black arrow), pneumomediastinum (thick black arrow) and right lateral chest wall surgical emphysema (white star). The severity of the complications is more evident on the CT (right) allowing for better characterisation of the extent of the pneumomediastinum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree